Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Research Article(ISSN: 2643-6760) 
A Comparison of the Time Efficiency and the Economics of Bone Graft Surgery vs. Computer-Aided Implant Surgery for Implant Placement in the Sinus Region: A Randomized Prospective Clinical Trial Study Volume 6 - Issue 3
Ghazwan Almahrous1, Sandra David Tchouda2, Nathalie Rançon3, Jean Luc Bosson4 and Thomas Fortin5*
- 1Department of Oral Surgery, University Claude Bernard, Lyon, France
- 2Medical Unit, University Hospital of Grenoble, France, France
- 3Department of Oral Surgery, Hospices Civils de Lyon, France
- 4Medical-Economic Evaluation Unit, University Hospital of Grenoble, France, France
- 5Oral Surgery department, Claude Bernard University, France
Received: May 10, 2021 Published: May 18, 2021
Corresponding author: Thomas Fortin, Oral Surgery Department, Claude Bernard University, Dental School, Lyon, France
DOI: 10.32474/SCSOAJ.2021.06.000236
Summary
Objective: To compare the time efficiency and the economics of Bone Graft Surgery (BGS) and Computer-Aided Implant Surgery (CAIS) for implant placement in patients with maxillary atrophy as well as the comparison of planned, placed, and loaded implants. Materials and Methods: Patients with extremely atrophic maxilla in need of implant placement were selected for a randomized controlled study clinical trial. The patients were divided randomly into two treatment groups: one group treated by using sinus grafting before implant placement and the group treated by using residual bone to place the implant by computer-aided implant surgery. Thirty Patients were assigned for each treatment group. The study provided a comparison of the time efficiency and economics of the two treatment groups.
Results: The results revealed a significant difference in terms of total surgical time duration and cost of treatment without prosthesis: p= 0.000. The time efficiency of time was 53.33 min for one implant while that of the CAIS group was 29 min for one implant; there was no significant difference in implant surgery duration p= 0.928; implant 2 surgery duration, p= 0.227 The Economic efficiency of the two groups was as follows: 1346.41 € for one implant in the BGS group versus 945.36 € for one implant in the CAIS group. While there was no significant difference in consultation fees p= 0.131and second implant surgery costs p= 0.584. And there was significant difference in assistant costs p= 0.000; treatment planning costs p= 0.000, implant surgery costs p= 0.006, and implant loading costs p= 0.048. In addition, there was no significant difference in the number of missing teeth p= 0.695; loaded implant p= 0.057 versus there was a significant difference in number planned implants p= 0.0074; implants p= 0.034 between the groups.
Conclusion: This study shows that Computer-Aided Implant Surgery seems to be more economical and time-efficient than the established conventional surgery by sinus lift and bone graft in dental implant placement, and the cost of treatment has increased for the sinus grafting procedures in Bone Graft Surgery. Also, the number of placed implants and planned implants was affected by the technique of implant placement. All planned implants were placed by Computer-Aided Implant Surgery while 81.5% of patients have placed their planned implants by bone grafting surgery.
Keywords: Dental Implant; Surgical Guide; 3D Imaging; Planning Software; Sinus Graft
Introduction
Implants allow the edentulous area to be reconstructed without damaging the teeth adjacent to the implant, and implant placement will satisfy the patient and facilitate the chewing ability [1]. Dentists are responsible for making appropriate therapeutic decisions and this requires an understanding of the outcome of treatment approaches and the benefits of alternative therapies, involving an assessment of longevity as well as physiologic, psychologic, and economic effects [2]. Patient-Reported Outcome Measures (PROMs) are used as status assessment to determine health care or treatment, and usually reported in the form questionnaires filled out by the patient, each patient replying directly to the questionnaire [3]. Several implant techniques have been used to avoid anatomical obstacles to implant placement. Sinus atrophy, one such anatomical obstacle prevents implants from being placed of an appropriate length of the implant. Thus, reducing the expanded size of the sinus cavity (partially or completely), by using appropriate surgical procedures, is important to remove this obstacle [3]. Grafting the sinus floor is a surgical technique for the maxillary sinus and has become the most common surgical intervention for increasing alveolar bone height prior to implant placement of adequate length. Sinus lifting procedures are performed to provide the required height of proper and stable bone tissue around the implants [4,5]. In digital dentistry, the introduction of novel hardware and software based on D3 images from CBCT for implant placement has been overcome without the damage to the neighboring vital anatomy [6]. The use of computer-guided surgery in virtual implant placement involves several stages: a diagnostic step (clinical and radiographic examination), a planning step (using planning software), and a surgical step (using a surgical guide) [7].
Since of our first publication on Image-Guided Surgery [8], many applications for planning implant placement have been proposed in advance. Good Control of the implant axis in prosthetic tooth position is one of the main advantages of computer-guided technology in implant dentistry [9]. The research for the clinical, technical, and economic outcomes for computer-guided surgery is rare in the current dental literature. In this context, scientific validation of surgical computer-guided planning is paramount for understanding the impact of using a 3D digital model surgical guide for implant placement in the final position avoiding eventual anatomical structures and modifying well-established conventional protocols in implant dentistry [7,10]. The benefits of static computer-aided implant surgery (s-CAIS) have been presented as the reduced costs of processing, less clinical treatment time, and simplified technical production with precision implant placement [11]. Therefore, adopting a fair approach in terms of a valuebased public policy perspective and an innovations evaluation in medical care is the main objective of economic assessment, and not only to reduce the cost of medical care [12]. A few studies are investigating looking at CAIS for PROMs as well as the economic effects that include time efficiency and treatment costs [13]. This article compares the economic effects for two-implant placement technique surgeries in the case of sinus atrophy with a null hypothesis, positing that there isn’t a significant difference between the two-implant placement surgery methods in terms of economic impact and with a Confidence Interval (CI) of 95%.
Methods
Trial Design, Inclusion/Exclusion
This was a randomized trial clinical study in a parallel group design at the Center for Dental Care, Teaching and Research, University Claude Bernard, Lyon 1, and was supported by the Civil Hospices of Lyon, France; under the name SINIMAGE (REF HCL: 2008.514/15). This randomized controlled trial (RCT) study followed the principles of the Helsinki Declaration and was approved by the local ethics committee (CPP 08/095, Ref. A 08- 230, 9 December 2008). Patients with a maxilla-free end atrophied sinus and needed dental implants to hold denture prosthesis were invited to participate in the study. Sixty patients were selected to participate in study; all had strong bone resorption for the sinus floor (i.e., a height of the alveolar bone less than 5 mm). Implant placement could be performed on all patients according to two techniques, the first by Bone Graft Surgery (BGS) via sinus lift (considered an ideal treatment), and the second by Computer- Aided Implant Surgery (CAIS) via using a surgical guide (depending on implant planning software).The participants were eligible to be treated with either BGS or CAIS and were fully informed about the study and provided written informed consent.
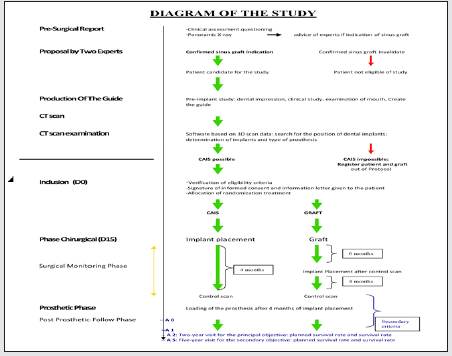
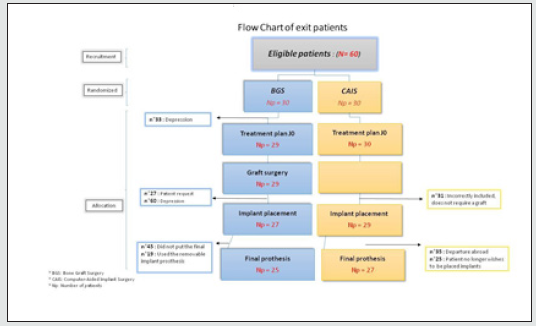
All the patients of the study were eligible and met the inclusion and exclusion criteria; the period of acceptance of inclusion within the study was two years. Study patients were distributed into two treatment groups using a random draw with sealed envelopes that included the name of the surgical technique to which they would belong, BGS or CAIS. The first patient joined the study in July of 2009; the last dental prosthesis was loaded in 2015. Then, after loading the prosthesis, an annual examination was conducted over the following five years. (Figure 1).
Inclusion Criteria
a) Patient’s age is over 18 years.
b) Patient has an indication for treatment by sinus lift.
c) Analysis of the patient’s scan shows that the treatment was possible via CAD.
d) Patient is without extraction within the last three months, has free end maxillary.
e) Patient has a non-contact prosthesis in the occlusal lateral movements.
f) Patient has an antagonistic arcade of natural teeth or implants.
g) Patient is a non-smoker or has stopped smoking as of 3 months prior.
Exclusion Criteria
a) Patient is unable to understand the doctor’s orders for legal, psychological, and linguistic reasons.
b) Difficulty in following up the patient to study (imminent change, insufficient motivation).
c) Pregnancy.
d) Patient is at risk of infective endocarditis or transmission of Creutzfeldt - Jakob disease.
e) Patient has severe/acquired immune deficiency.
f) Patient has a malignant jaw lesion or a history of radiotherapy of the mandible.
g) Patient has severe hemopathy, hemophilia, chronic renal failure, autoimmune disease or any disease that had required organ transplant, poorly controlled diabetes, osteoporosis, rheumatic arthritis, or psychiatric illness.
h) Patient is receiving antimitotic or immunosuppressive therapy, under high doses of corticosteroids.
i) Patient has a drug addiction.
j) Patient has engaged in smoking in the last three months.
k) Patient does not have his or her liberty.
Eligibility for Treatment was Established by the Following Procedures
a) Panoramic x-rays by a Planmeca ProMax® 2D (Planmeca Oy, Asentajankatu, Helsinki, Finland) device in the Center for Dental Care. The indication of Bone Graft Surgery was confirmed by two expert surgeons within the Center for Dental Care.
b) The associated laboratory of the Center for Dental Care fabricated the wax models and surgical guides.
c) 3D Imaging of patients was performed via Cone-beam CT by the Imaging Department of Edouard Herriot Hospital, in Lyon, France.
d) The Center’s surgeons used software based on 3D imaging for dental implants, the EasyGuide™ dental implant planning software (Keystone-Dental, Inc, Burlington, MA, USA). The Center’s surgeons determined the possibility of using the surgical guides to benefit the residual maxillary bone, (Figure 1).
e) Patient inclusion and exclusion criteria were assessed by clinical examination, 30 of whom would be treated via sinus floor elevation procedures, Bone Graft Surgery (BGS) treatment, whoe the other patients were treated using guided surgical Computer-Aided Implant Surgery (CAIS) (Figure 2).
The Case Report Form (CRF) for each treatment group included the details of the patients’ treatment as well as their answers to questions about treatment. Patient-Reported Measures (PROMs) evaluated the pain, patient satisfaction, difficulty, complications, and recommendations, with the results being similar between the two treatment groups [14]. Surgical details in the CRF have included the clinical description of the patient’s condition (i.e., number of missing teeth, number of planned Implants, number of placed implants, and number of implants loaded with the prostheses), along with the times and economic costs of the curative surgeries.
Time efficiency was evaluated by measuring the mean duration of total treatment surgeries and the mean number of implants loaded with a prosthesis; duration of total treatment surgeries was the sum of the surgical times of treatment for the patient. In addition, the economic efficiencies was evaluated of the two treatment groups by measuring the mean costs of treatment and the mean number of implants loaded with a prosthesis; economic costs were assessed for treatment from the planning treatment costs to implant loading costs.
Treatment Stages were Determined in the CRF for Each Group and All Details of Treatment were Recorded in it. Stages of Treatment were Determined as Follows
a) The implant planning stage, only for the Computer-Aided Implant Surgery group.
b) The grafting stage, graft surgery, and second graft surgery (when needed), only for the Bone Graft Surgery group.
c) The implant placement stage, implant placement, and second Implant placement (when needed), for both groups.
d) The implant loading stage; for the two groups.
e) This article will assess the time efficacy and costs for the surgeries of the two treatment groups, plus provide a description of the clinical status of the patients.
Surgical Procedure
Panoramic images of all patients confirmed the possibility of using the Bone Graft Surgery technology for the placement of implants (sub-sinus alveolar bone height < 5 mm) while 3D images of CBCT for all patient was confirmed by using the Easy Guide™ Dental Implant Planning Software and the possibility of using the Computer-Aided Implant Surgery (height and width of residual alveolar bone of maxilla at the sinus side more than 10mm x 5mm). Implants XiVE® (Dentsply Sirona Inc., Charlotte, NC, USA) and ANKYLOS® implants (Dentsply Sirona Inc.,) were placed for all patients and ranged in length from 8 to 13 mm and from 3.5 to 5.0 mm in diameter. Internal-Connection dental implants by PrimaConnex® Tapered Implant (Keystone Dental, Inc.) were used. Definitive prostheses were affixed to the implants by cement used in the oral surgery department.
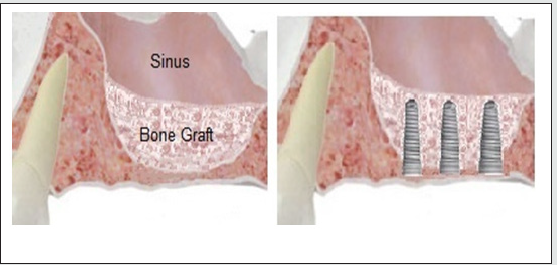
Group of Bone Graft Surgery (BGS)
The 30 patients in this group were treated via sinus bone graft in two-stages (Figure 3)
First Stage: A window was opened in the lateral wall of the maxillary sinus, after which the Schneiderian Membrane was lifted, followed by the placement of the bone allograft PHOENIX allograft bone (TBF GénieTissulaire, Mions, France) under the sinus membrane. After the bone graft was completed, it was supported by placing a DynaMatrix®membrane (Keystone Keystone Dental, Inc.) membrane for tissue regeneration, after which the flap was tightly closed.
Second Stage: Examination of sinus scan was performed before the start of the second stage to confirm the newly formed bone tissue. Bone integration of graft normally occurs 6 to 8 months after the implant insertion maneuver. After anesthesia was obtained, the pilot hole in the maxillary crest was drilled to achieve a suitable diameter to insert the implant. Finally, a cover screw was placed on the implant and then the surgery flap closed tightly.
Group of Computer-Aided Implant Surgery (CAIS)
30 patients for this group were treated by using a surgical guide created with EasyGuide™ Dental Implant Planning Software (Figure 4). Before the implant placement operation, a resin cube (a fiducial marker) was attached to the surgical template, and the positioning of implants was determined by EasyGuide™ Planning Software (Keystone Dental Inc.). A surgical template with the cube was installed and holes were made in it by a digitally controlled drilling machine according to the planning Software EasyGuide™ (Keystone Dental Inc.).
It has been suggested that the use of CAIS reduces procedural invasiveness. Several clinical studies of the surgical team have shown the reliability of computer-aided techniques for dental implant placement [15, 16].
After anesthesia, the surgical guide was fixed on the maxillary. The holes in the surgical guide determine the position and orientation of the implants in the maxillary. Surgical guide holes acted as the entrance to drill sleeves to create a cavity in the residual bone crest. Drills of several sizes were used in preparing the positions of implant insertion. Then the surgeon placed the implant in specified positions. Finally, a cover screw was placed and the surgery flap was tightly closed.
Statistical Analysis
The null hypothesis was considered in the statistical analysis, and it was determined that there was not an effect of the implant placement surgery on the variables that compared the two groups with P-value less than 0.05 as statistically significant. Descriptive statistics and normality tests were used to find out the distribution of these values which have been described by mean with SD (Standard Deviation); range (lowest and highest values); median with the interquartile range (IQR) for quantitative data, and percent values for qualitative data.
The differences between the two groups were compared by using the Mann-Whitney test and the association between them by using the Chi-Square test, considering a P-value of < 0.05. Statistical analysis has performed to compare time efficiency and economic cost differences between the two surgeries of implant placement, in addition to a comparison of the clinical status of the patients in the two surgical groups.
Results
Sixty participant patients were included in the SINIMAG study, distributed randomly for placement in the two groups of treatment, (BGS) and (CAIS). Some patients were dropped out of the study during the different stages of treatment.
Bone Graft Surgery Group (BGS)
30 patients participated for SINIMAG in the BGS group; some of them were dropped out of study during the different stages of the treatment, according to the CRF.
Planning Treatment: 30 patients were planned for treatment for inserting the bone graft by lifting the lower Schneiderian membrane.
Graft Surgery: 29 patients received the bone graft (one patient withdrew from the study due to depression, which did not allow further sinus treatment).
Implant Surgery: 27 patients had placed 75 implants (One patient requested to be removed from the study and another patient was excluded from the study after the failure of a bone graft and placed the implants by CAIS).
Implant loading: 25 patients had 68 implants loading with a fixed prosthesis (One patient used the removable implant prosthesis and another patient did not put the final prosthesis).
Computer-Aided Implant Surgery (CAIS)
30 patients participated for SINIMAG in the CAIS group; some of them were dropped out of the study during the stages of the treatment, according to the CRF:
Planning Treatment: 30 patients were planned for treatment by CAIS (3D imaging by CBCT, implant planning software, and guided surgical template).
Implant Surgery: 29 patients had placed 69 implants (one patient withdrew from the study due to a mistake in his entering the study - a misinterpretation of the x-ray films survey, which showed that the patient did not require bone grafting).
Implant Loading: 27 patients had 64 implants loading with a fixed prosthesis (one patient traveled abroad and another patient no longer wanted to be have implant placement).
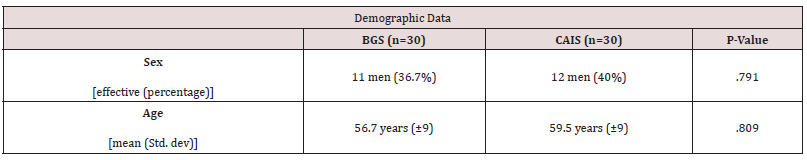
Baseline demographic patient data (Table 1) exhibited a mean age at inclusion similar in the two groups at a 5% threshold; 56.7 years ± 9.2 years (BGS group) vs. 59.5 years ± 9 years (CAIS group), p = 0.809. Also, the distribution by gender was similar within the two groups: 40% of men in the CAIS group vs. 36.7% in the BGS group, p = 0.791.
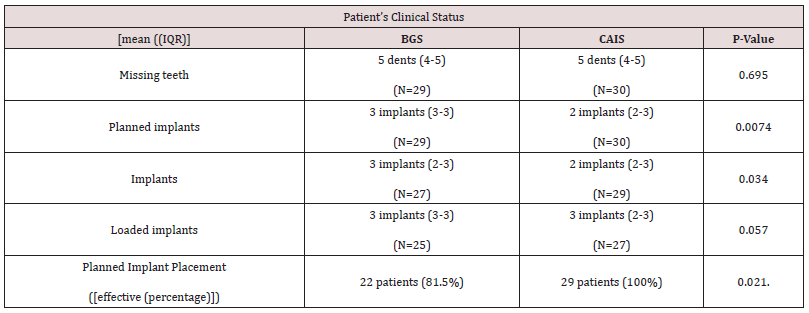
Patient’s Clinical Status
The median of the number of missing teeth was the same within the two treatment groups and also between the interquartile range; 5 teeth [IQR: 4; 5] and there was no significant difference in the number of missing teeth for both groups of treatment. The number of implants at the planning stage was NI: 87 implants for N: 29 patients in the BGS group vs. NI: 73 implants for N: 30 patients in the CAIS group (Figure 5). There was a significant difference in the number of planned implants between the two treatment groups and the median number of implants planned was greater in the BGS group at the threshold of 5%. The median of implants planned was 3 implants [IQR: 3: 3] in the BGS group vs. 2 implants [IQR: 2: 3] in the CAIS group, p = 0.0074. Also, the median number of implant placements is greater in the BGS group at the threshold of 5%; the median implant placement was 3 implants [IQR: 2; 3] in the BGS group vs. 2 implants [IQR: 2; 3] in the CAIS group. The number of implants at the implant placements stage was NI: 75 implants for N: 27 patients in the BGS group vs. NI: 69 implants for N: 29 patients in the CAIS group. There was a significant difference in the number of implant placements between the two treatment groups, p = 0.03. Also, there was no significant difference in the number of loaded implants between the two treatment groups, p = 0.057. The median number of loaded implants was 3 implants [IQR: 3; 3] in the BGS group vs. 3 implants [IQR: 2; 3] in the CAIS group. In addition, the proportion of patients who placed all planned implants was higher in the CAIS group 29 patients 100% vs.22 patients 81.5% in the BGS group at the threshold of 5%. There was a significant difference in the number of patients who placed all planned implants and the technique of implant placement surgery affected the number of patients (Table 2).
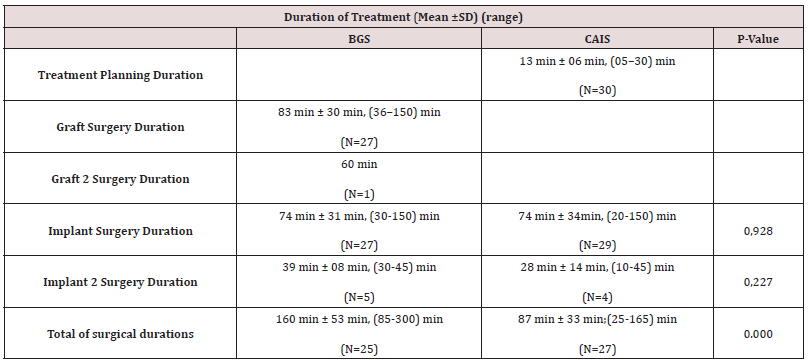
Times of Surgery Treatment
All durations of surgery were evaluated in hours (Table 3). Treatment planning duration was used only in the CAIS Group, all the aspects of the planning phase were based on guided surgery to help surgeons implant successfully. A surgical guide was created from dental implant planning software to effect implant placement accuracy. The duration of Treatment Planning by the expert was calculated by hour; the mean duration was 13 minutes ± 06 minutes with a range 05 to 30 minutes. On the other hand, the sinus lift (Graft Surgery) was used to graft bone into the maxillary sinus and it was performed only for the BGS group; thus, the mean time duration for the BGS was 83 min ± 30 min with range of 36 min to 150 min. One patient had a second bone graft surgery as a result of bone graft surgery failure; the duration of this surgery was 60 min. At the implant placement stage, 27 patients placed 75 implants in the BGS group vs. 29 patients placed 69 implants in the CAIS group. The mean duration of intervention for implant placement was similar for the two treatment groups at the threshold of 5%, 74 min ± 31 min in the BGS group vs. 74 min ± 34min in the CAIS group. There was no significant difference in duration of intervention between the two treatment groups; the surgical technique to place the implants did not affect the duration of intervention for dental implant placement; p = 0.928.
The second implants were placed for some patients who had failed implants, 5 patients placed second implants in the BGS group vs. 4 patients who placed second implants in the CAIS group. The mean duration of intervention for second implants placement was slightly longer for the graft treatment group at the threshold 5%; 39 min ± 08 min in BGS group vs 28 min ± 14 min in the CAIS group. There was no significant difference in duration of the second intervention of implant placement between the two treatment groups; p = 0.227. The total of surgical durations of treatment was determined up to the stage of loaded implants, collected to reflect all periods of surgical interventions for treatment (Treatment Planning Duration, Graft Surgery Duration, Graft 2 Surgery Duration, Implant Surgery Duration, and Implant 2 Surgery Duration). The number of patients who loaded implants was 25 patients in the BGS group vs. 27 patients in the CAIS group. The mean duration of the total of surgical durations was longer for the bone graft surgery treatment group and there was a significant difference in total duration of interventions between the two treatment groups; mean = 160 min ± 53 min in the BGS group vs. 87 min ± 33 min in the CAIS group; p= 0.000. Time efficiency was evaluated by measuring the mean duration of total treatment for surgeries and the mean number of loaded implants. The time efficiency was 160 min for 3 implants in the BGS group (53.33 min for one implant) vs. 87 min for 3 implants in the CAIS group (29 min for one implant). Thus, the time efficiency of the CAIS group was better than that of the BGS group.
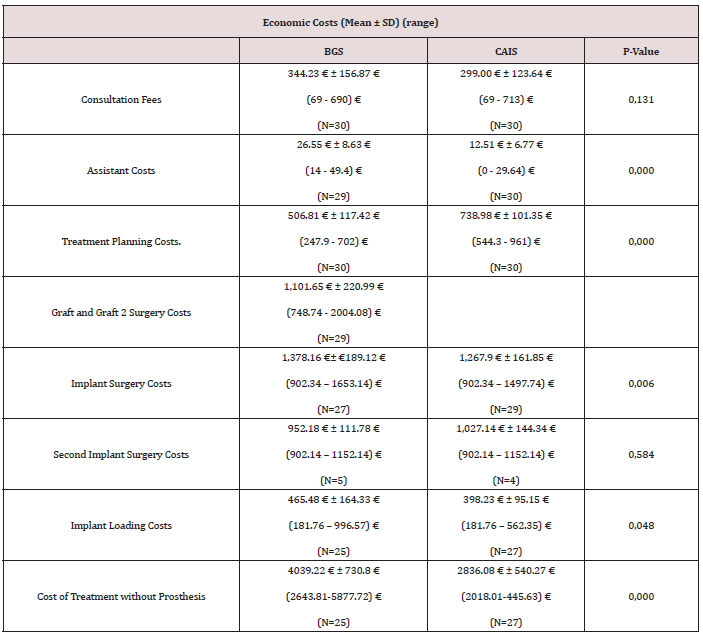
Economic Costs
The cost of the consultation was assessed at 23 € and also the hourly cost of the treatment plan study by the software of planning was estimated at 23 €. The hourly cost of the assistant was assessed at 9.88 € (Table 4).
References
There was no significant difference in consultation fees between the two treatment groups for all study patients and the mean of consultation fees was similar the two treatment groups, 344.23 € ± 156.87 € with range (69 - 690) € for the BGS group vs. 299.00 € ± 123.64 with range (69 - 713) € for the CAIS group; p= 0.131. The cost of graft surgery and second graft surgery cost were only available in the BGS group in addition to second graft surgery; their mean was 1,101.65 € ± 220.99 € with range (748.74 - 2004.08) €.There was a significant difference for each of the assistant costs, treatment planning costs, and implant surgery costs between the two treatment groups at the threshold of 5%. The mean of assistant costs was an increase in the BGS group; 26.55 € ± 8.63 € for BGS group vs. 12.51 € ± 6.77 € for CAIS group; p= 0.000. The mean of the treatment planning costs was an increase in the CAIS group in due to the cost of the perforating the surgical guide, used in the CAIS group; 506.81 € ± 117.42 € for the BGS group vs. 738.98 € ± 101.35 € for the CAIS group; p= 0.000. And the mean of costs implant surgery costs was slightly higher in the BGS group than in CAIS group; 1,378.16 €± €189.12 € for the BGS group vs. 1,267.9 € ± 161.85 € for the CAIS group; p= 0.006.
The mean of costs of the implant loading stage was similar the two treatment groups and there was no significant difference between the two treatment groups; €431 ± €200.9 in the group vs. €398.23 ± €95.15 in the CAIS group; p= 0,183. Twenty-seven patients for CAIS group and twenty–five for BGS group were in the implant loading stage. Costs of treatment were the sum of costs for all stages of treatment along with additional consultation fees and assistant costs up to the stage of implant loading, without cost of prosthesis. Five patients for BGS group and four patients for CAIS group were required a second implant surgery. The second implant surgery costs were similar between the two groups there was no significant difference, p= 0,584.
The technique of implant placement surgery affected the mean of costs of treatment; there was a significant difference in costs of treatment between the two treatment groups. The mean of costs of treatment reflected an increase in the BGS group compared to the CAIS group; 4039.22 € ± 730.8 € with range (2643.81-5877.72) € for the BGS group vs. 2836.08 € ± 540.27 € with range (2018.01- 445.63) € for the CAIS group; p= 0.000. The economic efficiency of each group was evaluated by measuring the mean costs of treatment and the mean number of loaded implants. Economic efficiency was 4039.22 €/3 implants in the BGS group, 1346.41 € for one implant vs. 2836.08 €/3 implants in the CAIS group, 945.36 € for one implant. It is noted that the economic efficiency of the CAIS group was better.
Discussion
This single-center trial was conducted for comparing the time efficiency and the economics for the two Implant placements in the sinus region. Two types of surgery protocols were performed for implant placement (according to the protocols followed) and all the data was recorded in the CRF (Case Report Form) of treatment; thirty patients by Bone Graft Surgery which used a bone graft in the pre-implant stage, which is considered the ideal treatment for in maxillary atrophy; and thirty patients by Computer-Aided Implant Surgery which used a guided surgery technique to insert the implants in their planned locations. Patients in the groups were randomly selected, so there was no significant difference in gender or age of patients. Also, on the result of random selection, there was no significant difference in patients’ ages, sex, and the number of missing teeth which was the same within the two treatment groups; the median 5 missing teeth.
Computer-Assisted Implant Technology is used for planning of implant placement and it is a valuable tool for the treatment of the morphologically complicated oral-maxillofacial region. The evaluation of bone morphology in three dimensions allows surgeons to evaluate and perform accurate virtual surgery preoperatively [17]. Another advantage is the accuracy of computer-aided implant surgery which places the implant at a distance of 1.5 mm from adjacent elements using the surgical guide. This gives the possibility of placing implants parallel to the sinus wall. The planning for treatment via dental implant planning software allows the possibility of planning and placing implants in front and behind the sinus in the bone residual maxillary; the size of the sinuses determines the number of implants placed. This justifies that implant placement surgery affects the number of planned implants and implant placements. There was a significant difference between the two treatment groups.
In addition, the technique of implant placement surgery affected the number of patients who placed all planned implants, and there was a significant difference between the two groups; P = 0.021. All patients (100%) of the CAIS group were placed with all planned implants While 5 patients (18.5%) did not place the same number of planned implants in the BGS group. Today, time resources are of great interest in daily dental practice, and yet studies that conduct time analyzes are still rare in current literature, particularly of digital implant placement.
Time efficiency reflects the extent of the effort needed for a certain procedure or goal and this efficiency is a measurable value, quantitatively determined by the ratio of output to input [18]. Only a few studies have investigated efficiency parameters comparing conventional and new treatment based on digital devices. CRFs included stages of treatment with recorded periods of surgeries. A comparison of surgical periods was performed between the two treatment groups in the treatment stages (treatment planning duration, graft surgery duration, graft 2 surgery duration, implant surgery duration, and implant 2 surgery duration). All study patients participated in stages of implant surgeries and second implant surgeries. There was no significant difference in the duration of the surgical intervention to place the implant and the duration of the second implant intervention. The mean of duration was similar and slightly longer for the graft treatment group in implant placement intervention. The duration of surgical intervention was dependent on the experience of the surgeon in implant placement.
For comparison, the sum of the periods of all surgical interventions was different between the two treatment groups, and there was a significant difference in the total duration of interventions. The mean duration of the total of surgical durations was longer for the bone graft treatment group. This is because implant placement was conducted in two stages for the BGS group, and the two-stage surgical treatment extended the time of the treatment [19]. In contrast, the CAIS group included the implant planning period and was not present in the BGS group. Also, the mean duration of treatment planning was 13 minutes much less than the mean duration of bone graft intervention which was 83 minutes. This investigation shows that the CAIS seems to be more time-efficient than the BGS surgery. The efficiency of time was 53 minutes for one implant in the BGS group versus 29 min for one implant in the CAIS group. In addition, the most economically efficient treatment was identified on measuring the mean of costs of treatment and the mean number of loaded implants, and it is noted that the economic efficiency of the CAIS group was better, in that there was a significant difference in costs of treatment between the two treatment groups with the mean of the BGS group 4039.22 € vs. 2836.08 € for CAIS group; p = 0.000.
There was a significant difference for each of the Assistant Costs and Treatment Planning Costs between the two treatment groups. Assistant Costs in the BGS group were more due to the increased period of surgeries in this group, performing a bone graft inside the maxillary sinus before the implant placements (Table 3), while treatment planning costs were high in the CAIS group due to costs of the surgical guide before the implants placement. There was a significant difference in implant surgery costs between the two treatment groups due to was a significant difference in the number of implant placements as well (Table 2). Cost of treatment without prosthesis was affected by the technique of implant placement surgery and there was a significant difference between the two treatment groups. There was an increase in costs of treatment in the BGS group compared to the CAIS group, 4039.22 € with a big difference in the lowest treatment cost 2643.81 € of and the highest cost 5877.72 € in the BGS group2836.08 € with the lowest treatment cost 2018.01€ and the highest cost 445.63 € in the CAIS group. The main reason for this increase was the costs of BGS and BGS 2 in the BGS group compared to planning costs (cost of guide and implant planning) in the CAIS group. CAIS Group was better in terms of economic efficiency, it was 945.36 € for one implant versus 1346.41 € for one implant in the BGS group. Previously published SINIMAGE comparison results, there were no statistically significant differences between BGS and CAIS regarding the majority of PROMs [20] . In this article the results of the comparison showed an increase in the duration and cost of treatment in the BGS group, the main reason being the use of two stages in a sinus lift procedure. The results of the comparison showed an increase in duration and cost of treatment in the BGS group, the main reason being the twostage sinus-lifting procedure.
Conclusion
The prospective clinical trial study showed that the number of the placed implants and planned implants were affected by the implant placement surgery technique. All planned implants were placed in the CAIS group while 81.5% of them were placed in BGS group. This investigation shows that Computer-Aided Implant Surgery seems to be more time-efficient than the established conventional surgery, Bone Graft Surgery. Of note as well, the cost of treatment without prosthesis was affected by the technique of implant placement surgery and was increased in Bone Graft Surgery, so the economic efficiency of computer-aided implant surgery was better than that of Bone Graft Surgery for implant placement in the sinus region.
Conflict of interest
The authors declare no conflict of interest.
References
- Allen F, McMillan A (2002) Food selection and perceptions of chewing ability following provision of implant and conventional prostheses in complete denture wearers. Clinical Oral Implants Research 13(3): 320-326.
- Guckes AD, Scurria MS, Shugars DA (1996) A conceptual framework for understanding outcomes of oral implant therapy. The Journal of Prosthetic Dentistry 75(6): 633-639.
- Weldring T, Smith SMS (2013) Patient-Reported Outcomes (PROs) and Patient-Reported Outcome Measures (PROMs). Health Serv Insights 6: 61-68.
- Thor A, Sennerby L, Hirsch JM, Rasmusson L (2007) Bone formation at the maxillary sinus floor following simultaneous elevation of the mucosal lining and implant installation without graft material: An evaluation of 20 patients treated with 44 Astra Tech implants. J Oral Maxillofac Surg 65(7 Suppl 1): 64-72.
- Stern A, Green J (2012) Sinus lift procedures: an overview of current techniques. Dent Clin North Am 56(1): 219-233.
- (2021) Evaluation of Accuracy of Dental Implant Positioning Placed using Digitally Planned 3D Printed Surgical Stent: A Case Series.
- Amorfini L, Storelli S, Romeo E (2011) Rehabilitation of a dentate mandible requiring a full arch rehabilitation. Immediate loading of a fixed complete denture on 8 implants placed with a bone-supported surgical computer-planned guide: A case report. J Oral Implantol. 37 Spec No:106-113.
- Fortin T, Coudert JL, Champleboux G, Sautot P, Lavallée S (1995) Computer-assisted dental implant surgery using computed tomography. J Image Guid Surg 1(1): 53-58.
- Kupeyan HK, Shaffner M, Armstrong J (2006) Definitive CAD/CAM-guided prosthesis for immediate loading of bone-grafted maxilla: A case report. Clin Implant Dent Relat Res 8(3): 161-167.
- Fasbinder DJ (2010) Digital dentistry: innovation for restorative treatment. Compend Contin Educ Dent 4: 2-11.
- van Noort R (2012) the future of dental devices is digital. dent mater 28(1): 3-12.
- Kamae I, Thwaites R, Hamada A, Fernandez JL (2020) Health technology assessment in Japan: A work in progress. Journal of Medical Economics 23(4): 317-322.
- Joda T, Derksen W, Wittneben JG, Kuehl S (2018) Static computer-aided implant surgery (s-CAIS) analysing patient-reported outcome measures (PROMs), economics and surgical complications: A systematic review. Clin Oral Implants Res 29 Suppl 16: 359-373.
- Almahrous G, David Tchouda S, Sissoko A, Rancon N, Bosson JL, Fortin T, et al. (2020) Patient-Reported Outcome Measures (PROMs) for Two Implant Placement Techniques in Sinus Region (Bone Graft versus Computer-Aided Implant Surgery): A Randomized Prospective Trial. International Journal of Environmental Research and Public Health 17(9): pp.2990.
- Verstreken K, Van Cleynenbreugel J, Marchal G, Naert I, Suetens P, van Steenberghe D,et al. (1996) Computer-assisted planning of oral implant surgery: A three-dimensional approach. Int J Oral Maxillofac Implants 11(6): 806-810.
- Fortin T, Bosson JL, Coudert JL, Isidori M (2003) Reliability of preoperative planning of an image-guided system for oral implant placement based on 3-dimensional images: An In vivo Int J Oral Maxillofac Implants 18(6): 886-893.
- Kanno T, Mitsugi M, Sukegawa S, Hosoe M, Furuki Y (2008) Computer-simulated bi-directional alveolar distraction osteogenesis. Clin Oral Implants Res 19(12): 1211-1218.
- Grünheid T, Patel N, De Felippe NL, Wey A, Gaillard PR, Larson BE, et al.(2014) Accuracy, reproducibility, and time efficiency of dental measurements using different technologies. Am J Orthod Dentofacial Orthop 145(2): 157-164.
- Krasny K, Krasny M, Kamiński A (2015) Two-stage closed sinus lift: A new surgical technique for maxillary sinus floor augmentation. Cell Tissue Bank 16(4): 579-585.
- Almahrous G, David Tchouda S, Sissoko A, Rancon N, Bosson JL, et al. (2020) Patient-Reported Outcome Measures (PROMs) for Two Implant Placement Techniques in Sinus Region (Bone Graft versus Computer-Aided Implant Surgery): A Randomized Prospective Trial. Int J Environ Res Public Health 17(9): 2990.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...