Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Original Article(ISSN: 2643-6760) 
A 10 Year, Single Centre Experience to Assess Role of Negative Suction in Resolution of Persistent Postoperative Air Leak for Empyema Thorax in Paediatric Patients Volume 4 - Issue 4
Natasha L Vageriya*, Rasik Shah, Shivaji Mane, Taha Daginawala and Prathamesh More
- Department of Pediatric Surgery, GGMC & Sir JJ hospital, India
Received: February 20, 2020; Published: March 02, 2020
Corresponding author: Moustapha Ndiaye, Hospital intern, Senegal
DOI: 10.32474/SCSOAJ.2020.04.000194
Abstract
Objectives: To evaluate whether external negative suction is more advantageous than only water seal in pediatric patients developing post-operative persistent air leak undergoing decortication for empyema thorax.
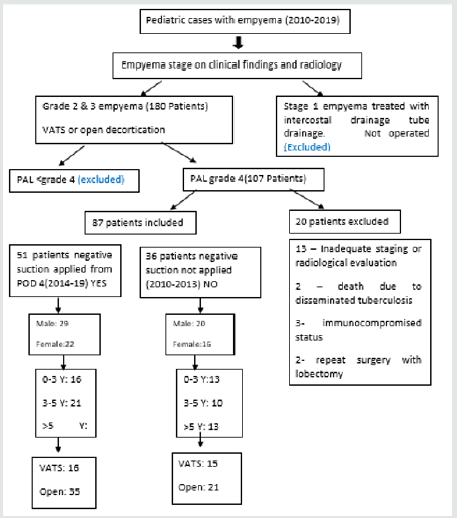
Methods: A retrospective analysis was done of all patients being admitted for empyema thorax at our centre from 2010 – 2019. Of these, total 180 patients with stage 2 and 3 empyema were identified and evaluated closely. Age distribution, sex prevalence, investigations performed, and treatment received was noted. Postoperatively patients developing persistent air leak (PAL) were compared with respect to grade of empyema, surgery performed, and postoperative negative suction applied or not. Their time to resolution of air leak after first 4 days post operatively was compared.
Results: Of 180 patients 107 had grade four persistent air leaks even after 4 days of underwater seal drainage, of these 20 patients were excluded as per exclusion criteria. Remaining 87 patients were divided in two comparable groups. From 2010 – 2013 patients were not receiving postoperative negative suction for PAL they were managed on under-water seal drainage only. During this period, 36 such patients were found. Their time for resolution of air leak was compared with 51 patients who had received negative suction for PAL from 2014-2019. The primary end point was the time elapsed between placement and removal of drains. All the data was analysed, and comparisons done. This was then subjected to statistical analysis and tests. No significant difference was found in the two groups. Whether the negative suction was applied or not the time to stoppage of air leak or recovery was identical.
Conclusion: In Pediatric patients undergoing decortication for empyema thorax; either VATS or Open; applying negative suction to intercostal drainage offers no additional advantage in closure of PAL or recovery.
Abbreviations:PAL: Persistent Air Leak; VATS: Video Assisted Thoracosopic Decortication; CECT: Contrast Enhanced Computed Tomography; STS: Society of Thoracic Surgeons
Introduction
Empyema thorax is a prevalent condition especially in the poor socioeconomic strata in developing countries like ours. American Thoracic society has described 3 stages of empyema. While most literature supports use of appropriate antibiotics with or without chest tube drainage for stage 1, Video assisted thoracosopic decortication (VATS) or fibrinolytics for stage 2 and open decortications for stage 3, the treatment modalities for transitions of each of these require treating doctors’ decision. All of these are associated with due morbidity and longer hospital stay. After surgical treatment, PAL can add to the morbidity and needs to be addressed. Although not much literature exists on application of negative suction as a part of its management, it is well known. But its efficacy needs to be weighed against the pain, decreased mobility and cost associated with it. In this study we have done retrospective analysis of these patients and compared the number of days in which intercostal drainage tube could be removed in patients who received or did not receive a negative suction to under water seal drainage tube for PAL.
Material and Methods
This is a retrospective case control study, examining all
pediatric patients admitted for empyema thorax who underwent
decortications and developed PAL. This study was approved by the
institutional review board at GGMC and sir JJ hospital and individual
consents waived. Exclusion criteria were patients with stage 1
empyema; no air leak postoperatively; with inadequate staging
or not evaluated by contrast enhanced computed tomography
(CECT), immune compromised status, undergoing repeat surgery
lobectomy;, for the ease of comparison and to avoid bias. Of 180
patients with stage 2 and 3 empyema; only 107 had grade four
persistent air leaks even after 4 days of underwater seal drainage,
of these 20 patients were excluded as per exclusion criteria.
Remaining 87 patients were divided in two comparable groups.
All the patients included in study were divided in 2 groups; group
1 with stage 2 and 3 empyema had received negative suction of -10
to-20 cm of water for post-surgery air leak from 2014-2019 and had
51 patients. The control group was comparative group of stage 2
and 3 empyema who had not received negative suction for PAL from
2010-2013 consisting of 36 patients. Staging was done on basis of
CECT findings. Data was obtained from the medical record section
of the hospital, with patient history and investigation records with
images and in hospital charts with complete pre and postoperative
data available. The number of days from surgery till ICD removal
after first 4 days of underwater seal drainage was compared (Figure
1) and subjected to statistical analysis.
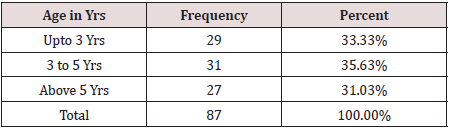
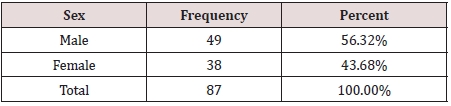
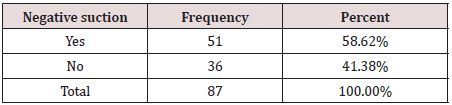
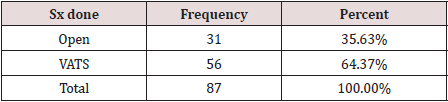
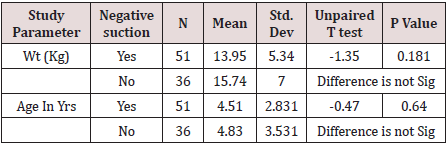
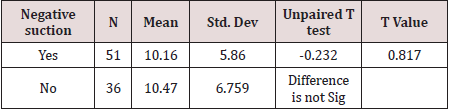
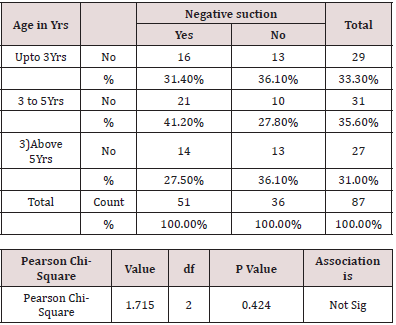
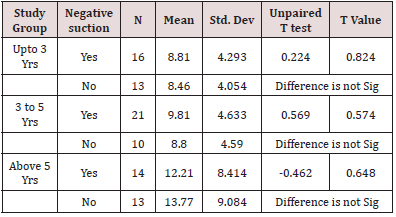
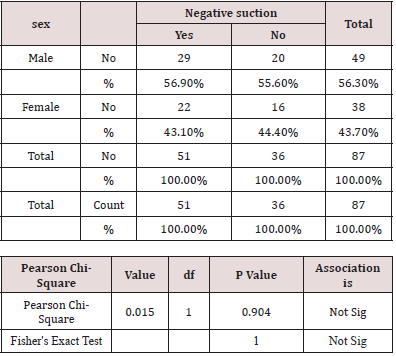
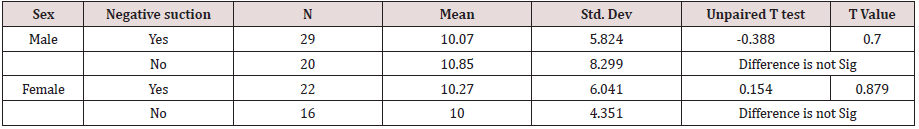
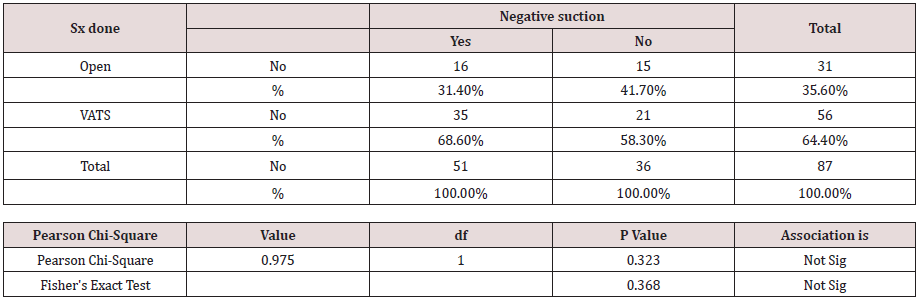
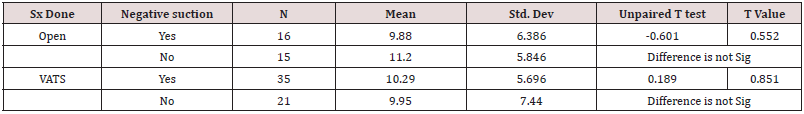
Results: Over 10 years 87 patients included in study with stage 2 or 3 empyema having grade 4 PAL were identified. Age of patient ranged from 3 months to 11 years (Table 1). There were 49 boys and 38 Girls (Table 2). In first group patients undergoing surgery: VATS or open decortication subjected to negative suction – 10 to -20 cm of water were compared with the second group not subjected to negative suction (Tables 3&4). Initially baseline parameters were compared (Table 5). After data collection, data entry was done in Excel. Data analysis is done with the help of SPSS Software version 15. Quantitative data is presented with the help of Mean, Standard Deviation, Median and IQR, comparison among study groups is done with Unpaired T test. Qualitative data is presented with the help of Frequency and Percentage table; association among various study parameters is assessed by Chi-Square test (Fisher Exact test for 2*2 tables). P value less than 0.05 is taken a significant level.
This comparison was done collectively by unpaired t test and the difference was not found to be significant (Table 6). Also the comparison was done in identical groups; age wise (Tables 7&8), sex wise (Tables 9&0), as per CT grading (Table 11) and surgery wise (Tables 12&13) ; appropriate statistical analysis was done subjecting to Pearson chi square test and Fisher Exact test. In all these comparisons the difference was not found to be significant. Hence whether the negative suction was applied or not the time to stoppage of air leak or recovery was identical. Thus, from this study we infer; negative suction has no additional advantage in early closure of PAL hence recovery of patient.
Discussion
The definition for the term PAL varies in multiple published
studies and proposed definitions of PAL range from an air leak
lasting four days to greater than ten days postoperatively [1]. Based
on recent literature several authors have recommended defining
a PAL as an air leak lasting beyond postoperative day 4. This
definition is consistent with The Society of Thoracic Surgeons (STS)
database definition for a PAL as an air leak exceeding the otherwise
necessary length of stay [2]. PAL is the most prevalent postoperative
complication with reported occurrence of 18-26% to higher rates
45-58% surgeries; more so after infectious conditions [2]. After
decortication procedures whether video assisted or open, PAL is
very prevalent and associated with significant morbidity. Some
surgeons theoretically believe that suction has the advantages of
favouring the apposition of parietal and visceral pleurae, promoting
the sealing of air leaks [3,4]. This approach seems more reasonable,
particularly after pulmonary lobectomy when a greater pleural
residual space is created compared with minor resections. On the
other hand, suction applied to the tubes may lead to an increase
in the volume of air leaking from the parenchyma, hindering the
sealing process [5]. Hence, the benefit of active suction applied to
the underwater seal drainage for reduction of postoperative leaks
is inconclusive. Application of active suction to underwater seals in
an attempt to close these and decrease hospital stay thus needs to
be evaluated along with morbidity associated with it.
In English literature multiple papers have been published
addressing PAL and various options for management including
application of negative suction to underwater seal drainage tube
for early sealing [6]. However majority of these studies are in adults
and mainly after lung resection. Yet no standardization could be achieved in favor of or against using suction with mixed results. Very
little literature approaches PAL in pediatric patients post empyema
thoracis. Also, in developing countries like ours it is difficult to afford
or provide hemlich valve, portable suctions and digital thoracic
drainage, as most of children suffering from empyema thorax are
from lower socioeconomic groups. Hence traditional underwater
seal drainage is kept post procedure for all these patients at our
institute. These children are observed for air leak and patients with
grade four air leak, as per Cerfolio classification of air leaks [7],
persistent even after 4 days after surgery are subjected to negative
suction application to under-water seal.
In this study we retrospectively evaluated records of all pediatric
patients undergoing decortication from 2010-2019. We found
that patients treated between years 2010-2013 with PAL were
managed only with underwater seal drainage till the resolution
of air leak. From year 2014 to 2019 such patients were put on
negative suction to drainage system at -10 to -20 cm of water to
early closure of leaks and subsequently Intercostal drains removed
and patients discharged. All these patients were divided in three
age groups having stage 2 or 3 empyema on CT scan undergoing
decortication either VATS or open accordingly. Two groups were
made from these as per whether negative suction was used or not
and compared, where we found no significant difference between
the two. Applying negative suction to intercostal drainage for PAL
increases the morbidity of children by increasing the pain, reduced
mobility and adds to the cost of management without offering any
additional advantage in decreasing the air leak early. On reviewing
English literature, we found a few studies supporting our findings
although done in adults and for PAL after lobectomy [8]. Even by a
meta-analysis of all articles comparing the application of negative
suction to drainage and patients managed without it, there was
no significant difference between suction and non-suction on the
duration of prolonged air leaks [6].
Conclusion
In Pediatric patients undergoing decortication for empyema thorax; either VATS or Open; applying negative suction to intercostal drainage offers no additional advantage in closure of PAL or recovery.
References
- Singhal S, Ferraris VA, Bridges CR (2010) Management of alveolar air leaks after pulmonary resection. Ann Thorac Surg 89: 1327-1335.
- Michael Rolf Muller, Beatrice A Marzluf (2014) The anticipation and management of air leaks and residual spaces post lung resection. J Thorac Dis 6(3): 271-284.
- Brunelli A, Monteverde M, Borri A, Salati M,Marasco RD et al. (2004) A Comparison of water seal and suction after pulmonary lobectomy: a prospective randomized trial. Ann Thorac Surg 77: 1932-1937.
- Brunelli A, Sabbatini A, Xiume F, Refai MA, Salati M, et al. (2005) Alternate suction reduces prolonged air leak after pulmonary lobectomy: a randomized comparison versus water seal. Ann Thorac Surg 80: 1052-1055.
- Marshall MB, Deeb ME, Bleier JI, Kucharczuk JC, Friedberg JS, et al. (2002) Suction vs water seal after pulmonary resection: a randomized prospective study. Chest 121: 831-835.
- Bo Deng Qun, You Tan Yun, Ping Zhao Ru, Wen Wang Yao, Guang Jiang (2010) Suction or non-suction to the underwater seal drains following pulmonary operation: meta-analysis of randomised controlled trials. European Journal of Cardio-Thoracic Surgery 38(2): 210-215.
- Karen C Dugan, Balaji Laxmanan MD, Septimiu Murgu MD, Kyle Hogarth D (2017) Management of Persistent Air Leaks. Department of Medicine, Section of Pulmonary and Critical Care, University of Chicago, Chicago, IL 152(2): 417-423.
- Christos Prokakis, Efstratios N Koletsis, Efstratios Apostolakis (2008) Routine Suction of Intercostal Drains Is Not Necessary After Lobectomy: A Prospective Randomized Trial. World Journal of Surgery 32: 2336-2342.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...