Lupine Publishers Group
Lupine Publishers
Case Report(ISSN: 2644-1306) 
Persistent Pulmonary Symptoms in two Adolescents: Could It be a Lung Tumor? Volume 1 - Issue 3
Soldatou Alexandra1*, Syggelou Angeliki1, Stamataki Sofia2, Taprantzi-Potamianou Polyxeni1 and Lydia Kossiva1
- 1Second Department of Pediatrics, University of Athens Medical School, Greece
- 2Department of Pediatric ENT, P & A Kyriakou Children’s Hospital, Greece
Received: May 27, 2019 Published: June 14, 2019
*Corresponding author: Alexandra Soldatou, Second Department of Pediatrics, University of Athens Medical School, Greece
DOI: 10.32474/TRSD.2019.01.000112
Abstract
We report on two adolescents with primary endobronchial tumors. They both presented with subacute onset of respiratory symptoms, poor response to conventional medical therapy and pulmonary function test findings suggestive of intrathoracic obstruction. Due to prompt bronchoscopic evaluation, timely resection of the tumors was performed.
Keywords: Atypical carcinoid tumor; Primary endobronchial tumor; Pulmonary neuroendocrine tumor; Intrathoracic obstruction
Introduction
Primary endobronchial tumors in childhood are extremely rare. Because of low clinical suspicion and the variable ways of presentation, they are often misdiagnosed as benign conditions resulting in delayed diagnosis [1]. Herein we report two cases of primary endobronchial tumors in adolescents who presented to the Emergency Department of a tertiary pediatric hospital.
Case 1
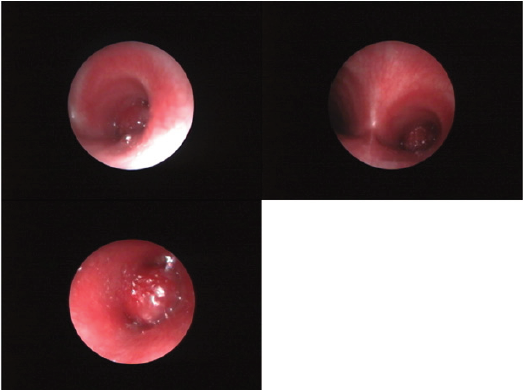
Figure 1: Pictures from bronchoscopic evaluation of case 2. The bronchial tumor occupies completely the right mainstem bronchus.
A 14-year-old female presented with acute onset of cough, fever and chest pain. She had a one-month history of cough treated with broad-spectrum antibiotics and bronchodilators. Several hours prior to admission, she developed fever up to 39.5 oC with chills and chest pain with radiation to her back on deep inspiration. Her past medical and family histories were unremarkable. She was a well-developed adolescent female in no acute distress, 98% oxygen saturation in room air and normal breath sounds on auscultation. Laboratory studies revealed leukocytosis (WBC, 16.6 x 103/μl) with a predominance of neutrophils (80%), elevated C-reactive protein (CRP, 89 mg/L) and erythrocyte sedimentation rate (ESR, 75mm). A chest radiograph revealed left upper lobe atelectasis and infiltrate, and a small effusion in the left lung lingula (Figure 1).
A new course of antibiotics and bronchodilators was given with prompt clinical and laboratory response. Blood cultures remained negative. Despite systematic bronchodilation, she developed diffuse wheezing on auscultation. A flow-volume curve obtained at that time revealed a pattern compatible with intrathoracic airway obstruction. Chest computed tomography (CT) confirmed the radiographic findings: atelectasis and infiltrate of the left upper lobe.
Due to the persistence of the airway obstruction, she underwent bronchoscopic evaluation where a lesion obstructed the left upper bronchus completely and the left main stem bronchus by 60%. A radial endobronchial ultrasound demonstrated intraluminar invasion (2cm) resulting in post obstructive atelectasis. The biopsy of the lesion was compatible with an atypical carcinoid tumor of the lung. Our patient underwent left upper lobe lobectomy. More than 20 lymph nodes examined were disease-free. Three years post operatively she remains asymptomatic with negative follow up chest CT and bronchoscopy
Case 2
A 15-year-old male presented with a two-day history of fever
up to 40 oC with chills, mild cough and right-sided chest pain. He
had an eight-month history of persistent cough despite the use
of inhaled bronchodilators. Two months prior to presentation he
was hospitalized with right lower lobe pneumonia. A rightward
mediastinal shift found on chest X-ray (CXR) at that time prompted
a chest CT scan that revealed situs inversus with dextrocardia and
the presence of a mass obstructing the right mainstem bronchus.
No further investigation was performed as his parents declined
consent. There were no further remarkable findings from his past
medical and family history.
Upon admission, he was a well-developed male in no acute
distress. Oxygen saturation measurement was 98% in room air.
Significant findings on physical examination were reduced air
entry in the right lung field and heart sounds best heard on the right
side of the chest. Laboratory studies revealed elevated WBC count
(15 x 103/μl) with a predominance of neutrophils (84%) and an elevated CRP 178mg/L. A right middle lobe density was found on
CXR examination. Blood and sputum cultures were negative.
Despite treatment with antibiotics, steroids, bronchodilation
and physiotherapy, he remained symptomatic with decreased breath
sounds in the affected side and a flow-volume curve pattern was
compatible with intrathoracic airway obstruction. Bronchoscopic
evaluation revealed a lesion obstructing completely the right
mainstem bronchus. Following cardiothoracic consultation, it
was decided to proceed with laser photoresection of the lesion
in a specialized medical center in the United Kingdom. Histologic
evaluation of the lesion set the diagnosis of typical carcinoid. He
underwent repeated bronchoscopies for the removal of the lesion.
The patient was placed on close monitoring protocol.
Discussion
Our cases underline the importance of early diagnosis of
endobronchial lesions in pediatric patients. Sub-acute onset
of respiratory symptoms, poor response to standard medical
treatment, along with findings on pulmonary function tests
suggestive of intrathoracic obstruction prompted further
radiological and endoscopic investigation in only a few days. A
small series review from France revealed a mean delay between
symptoms appearance, diagnosis and surgical treatment of 5.6
months [2]. Isolated reports however describe pediatric patients
who were treated as asthmatics for years (2 -5.5 years) prior to
diagnosis [3,4].
Endobronchial lesions should be considered in children with
persistent pneumonia or respiratory symptoms despite adequate
treatment. Primary bronchial tumors seldom occur in children,
and represent a rare cause of pulmonary obstruction. The most
frequent histologic subtype is well-differentiated neuroendocrine
tumor (NET), or carcinoid [5].
Symptoms of the obstructive nature of the tumor are variable;
small pediatric patient series report the following presenting
symptoms: recurrent pulmonary infection, pneumonia, cough,
haemoptysis, chest pain, weight loss and persistent wheezing
[1,2,5]. A significant asymptomatic percentage of adult patients
(as high as 25%) has been reported [6,7]. Evidence of atelectasis/
collapse on chest X-ray and CT heighten the index of suspicion.
Rarely symptoms such as flushing, diarrhea, palpitation, shortness
of breath consistent with carcinoid syndrome may occur. Those
symptoms are caused by serotonin release from the tumour. In
pediatric patients, carcinoid syndrome is extremely rare [8]. Our
patients did not exhibit symptoms of carcinoid syndrome.
The lung is the second most common site of occurrence of
well-differentiated NETs, after the gastro-entero-pancreatic axis.
The 2004 World Health Organization classification recognizes
four major histopathologic types of lung NETs: low-grade typical
carcinoid, intermediate-grade atypical carcinoid, high-grade small
cell and large cell carcinoma. Among pulmonary NETs, typical and atypical carcinoid tumors of the lung are generally indolent, but
capable of very late recurrence or metastasis [9].
The incidence of these lesions and their outcomes are still
largely unknown, although an increased incidence of NETs in
the last decade has been noticed worldwide. Review of the scant
relevant literature suggests a predominance of low-grade typical
carcinoids. Patients with atypical disease are three times more
likely to succumb from metastasis/locally advanced tumor at
presentation or recurrent disease following resection than patients
with typical disease [10].
Despite their malignant potential, complete conservative
resection prior to tumor spread is the treatment of choice for the
management of pediatric bronchial carcinoids. Bronchoscopic
removal of the tumor is not considered as first line treatment but it
has been reserved for cases in which surgical intervention carries an
unexceptably high risk [11,12] and remains an appealing approach
that needs further evaluation [13]. Relapses can be successfully
surgically treated and can occur even after many years, highlighting
the importance of long-term follow-up, probably for life [14].
In accordance with previous reports, our patients belonged
to adolescent age-group; therefore they were able to perform the
spirometric evaluation, which was characteristic of obstruction [15-
17]. The problem is difficult to solve when the patient is younger and
suffers recurrent episodes of wheezing and respiratory infections.
A high degree of suspicion is necessary in order to decide which
patient needs further evaluation.
References
- Al-Qahtani AR, Di Lorenzo M, Yazbeck S (2003) Endobronchial tumors in children: Institutional experience and literature review. J Pediatr Surg 38(5): 733-6.
- Yu DC, Grabowski MJ, Kozakewich HP, Perez-Atayde AR, Voss SD et al. (2010) Primary lung tumors in children and adolescents: a 90-year experience. J Pediatr Surg 45(6): 1090-5.
- Fauroux B, Avnie V, Larroquet M, Boccon-Gibod L, Ducou le Pointe H, et al. (2005) Carcinoid and mucoepidermoid bronchial tumours in children. Eur J Pediatr 164(12): 748-52.
- Machuca TN, Cardoso PF, Camargo SM, Signori L, Andrade CF, et al. (2010) Surgical treatment of bronchial carcinoid tumors: a single-center experience. Lung Cancer 70(2): 158-62.
- Rizzardi G, Marulli G, Calabrese F, Rugge M, Rebusso A, et al. (2009) Bronchial carcinoid tumors in children: surgical treatment and outcome in a single institution. Eur J Pediatr Surg 19(4): 228-231.
- Andersen JB, Mortensen J, Damqaard K, Skov M, Sparup J, et al. (2010) Fourteen-year-old girl with endobronchial carcinoid tumour presenting with asthma and lobar emphysema. Clin Respir J 4(2):120-124.
- Aydin E, Yazici U, Gulgosteren M, Agackiran Y, Kaya S, et al. (2011) Long-term outcomes and prognostic factors of patients with surgically treated pulmonary carcinoid: our institutional experience with 104 patients. Eur J Cardiothorac Surg 39(4): 549-554.
- Cogen JD, Swanson J, Ong T (2016) Endobronchial carcinoid and concurrent carcinoid syndrome in an Adolescent Female. Case Reports in Pediatrics.
- Moraes TJ, Langer JC, Forte V, Shayan K, Sweezey N (2003) Pediatric pulmonary carcinoid: a case report and review of the literature. Pediatr Pulmonol 35(4): 318-322.
- Cakir M, Grossman A (2011) The molecular pathogenesis and management of bronchial carcinoids. Expert Opin Ther Targets 15(4): 457-491.
- Cardillo G, Sera F, Di Martino M, Graziano P, Giunti R, et al. (2004) Bronchial carcinoid tumors: nodal status and long-term survival after resection. Ann Thorac Surg 77(5): 1781-1785.
- Fiala P, Petrásková K, Cernohorský S, Kinkor Z, Krepela E, et al. (2003) Bronchial carcinoid tumors: longterm outcome after surgery. Neoplasma 50(1): 60-65.
- Caplin ME, Baudin E, Ferolla P, Filosso P, Garcia-Yuste M, et al. (2015) Pulmonary neuroendocrine (carcinoid) tumors. European Neuroendocrine Tumor Society expert consensus and recommendations for best practice for typical and atypical pulmonary carcinoids. Ann Onc 26(8): 1604-1620.
- Naalsund A, Rostad H, Strøm EH, Lund MB, Strand TE (2011) Carcinoid lung tumors-incidence, treatment and outcomes: a population-based study. Eur J Cardiothorac Surg 39(4): 565-56
- Cogen JD, Swanson J, Ong T (2016) Endobronchial Carcinoid and Concurrent Carcinoid Syndrome in an Adolescent Female. Case Reports in Pediatrics.
- Guerreiro C, Ornelas P, Pereira L, Abecasis N, Almodovar MT (2017) Atelectasis in pediatrics: a case of carcinoid tumor. Rare Tumors 9(3):7049.
- Madafferi S, Catania VD, Accinni A, Boldrini R, Inserra A(2015) Endobronchial tumor in children: Unusual finding in recurrent pneumonia, report of three cases. World J Clin Pediatr 4(2): 30-34.