Lupine Publishers Group
Lupine Publishers
Case Report(ISSN: 2644-1306) 
Lichen Planus in Down Syndrome: Treatment with Systemic Retinoid - An Observation Volume 1 - Issue 3
Mohammad A Hye1* and Siddhartha Shankar Dutta2
- 1Department of Dermatology, Jalalabad Ragib-Rabeya Medical College, Bangladesh
- 2Department of Dermatology, Sylhet M.A.G Osmani Medical College, Bangladesh
Received: June 08, 2019 Published: June 18, 2019
*Corresponding author: Mohammad A Hye, Department of Dermatology, Jalalabad Ragib-Rabeya Medical College, Bangladesh
DOI: 10.32474/TRSD.2019.01.000113
Abstract
Down syndrome (DS) is the most common congenital abnormality affecting numerous organs and is associated with an increased incidence of many cutaneous diseases. DS is an extensively researched condition but its associated cutaneous diseases are not well studied. Only a small numbers of case reports on lichenoid diseases associated with DS are reported in literature. So far, we know, there is no report published on classical lichen planus with DS until now. We reported a case of lichen planus in an adult patient of Down syndrome. We treated the patient with systemic acitretin. Patient has been observed for last three years. A good result was observed without any complication or relapse.
Keywords: Lichen planus; Acitretin; Down syndrome
Introduction
Down syndrome (DS), also known as trisomy 21, is an
autosomal chromosomal disorder caused by the presence of all
or part of a third copy of chromosome 21. It is typically associated
with physical growth delays, characteristic facial features and mild
to moderate intellectual disability. Down syndrome is one of the
most common chromosome abnormalities in humans with a birth
incidence of approximately 1 in 1000 live birth [1]. The cutaneous
manifestations of DS are numerous [2-6]: common associated
condition are: xerosis, atopic dermatitis, seborrheic dermatitis,
cutaneous infections, alopecia areata, vitiligo, syringomas, elastosos
keratoderma palmaris et plantaris, pityriasis rubra pilaris.
We describe an adult patient with Down syndrome, associated
with lichen planus (LP). LP is an inflammatory muco-cutaneous
disease characterized by shiny, flat-topped papules and plaques.
It affects around 1% of the population. The disease is usually selflimiting
and benign in nature. However, some varieties of LP may
cause considerable discomfort and recalcitrant in nature. Owing to
advances in medical care and changes in attitude, the life expectancy
of the DS patients is improving. A good number of research
papers is published in medical literature regarding physical and
psychological aspects of this disease. But papers related to LP and
other cutaneous aspects of DS are not enough in number. Still, there
is no published report on LP associated with DS. But LP is a disease
which significantly affect quality of life of patient. The disease is
also associated with many immunologically altered condition [7].
DS is also a medical condition with altered immune function [4,8].
So, an appreciation and higher research of LP associated with DS is
very important for comprehensive medical care as well as quality of
life of these patients.
Case Report
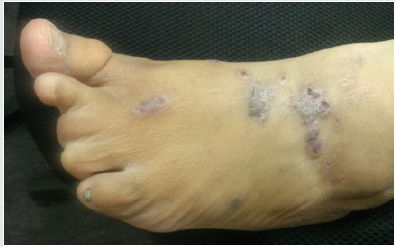
A 33 years old Bangladeshi female presented with flat topped, violaceous papules and plaques in flexor surface of wrist, trunk and foot for last 2 (two) years. Plaques in foot were polymorphic in shape, 1.5cm to 2cm in diameter with wickham’s striae in surface (Figure 1). The lesions were slightly hypertrophic and signs of scratching were seen. However, lesions in wrist (Figure 2) and trunk were smaller in size. She complained of severe itching. Her treatment history revealed that she was prescribed both topical and systemic steroid several times with partial outcomes and recurrences.
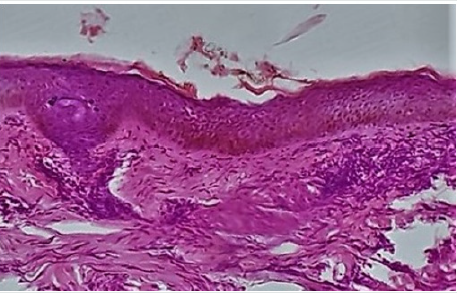
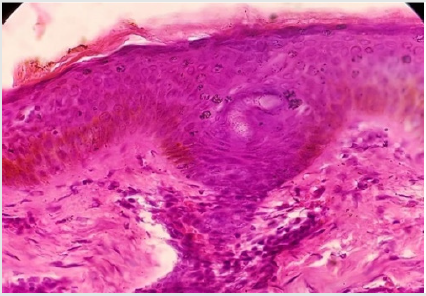
Her physical appearance was compatible with that of DS and following features were observed: epicanthic fold, brachicephaly, and depressed nasal bridge, upward angle of eyes, short broad neck and widened hands and foot and shortening of 4(four) lateral toes. Routine laboratory data were between normal ranges. Her liver and kidney function parameter were within normal range. Histopatholgical study revealed Hyperkertatosis, hypergranulosis, Vacuolar degeneration of basal layer of epidermis and inflammatory cell infiltrate in upper dermis (Figure 3 & 4). These findings are compatible with lichen planus. Her lipid profile was within normal limit. An interview with her family revealed that she had learning disability otherwise she was psychologically sound; She had only one brother and nobody of her family members had any relevant clinical conditions.
She was a diagnosed case of DS and received several therapies
in different institution by both internist and dermatologist. Her
past history revealed that she had frequent episodes of bacterial
and fungal infection since childhood. She revealed a treatment
history of several course of topical and systemic steroid since last 2
yrs without any satisfactory outcome.
After proper counseling we prescribed her systemic Acitretin
(25mg) daily for 1month. She was examined after 1 month and
we found her lesions were significantly cured with less intensity
of itching. She was prescribed again for Acitretin (25mg) for
consecutive 2 month after evaluation of her relevant laboratory
parameters. She attended after 1month with 90% clearance of
lesions. In her follow up visit after I month, she was found fully
cured. Patient did not complain of any significant side effects of the
drugs. There was no relapse within one year after discontinuation
of treatment.
Discussion
Few case reports on lichen nitidus with DS were reported in
literature but cutaneous LP associated with DS is not reported until
now. LP is one of the common disease in dermatology. The overall
prevalence of lichen planus in the general population is about 0.1–
4.0% [9]. It generally occurs more commonly in females, in a ratio
of 3:2, and most cases are diagnosed between the ages of 30 and 60,
but it can occur at any age [9].
Pathogenesis of LP is not fully understood. However, there is a
general consensus that LP is an immunologcally-mediated disease,
where basal cell damage occurs due to a complex interaction
between keratinocytes, Langerhan’s cells and T cells [7].
The LP with DS is no ta recognized association. However, it
is shown in different studies that cutaneous diseases are more
frequent in patients of DS than normal population. Morever, it is
reported that immune-mediated diseases like atopic dermatitis, psoriasis, seborrheic dermatitis etc are more frequent in patients
of DS [4] LP is usually a self-limiting benign disease some form of
the disease may persist for a long duration and may cause a range
of morbidity.
Without treatment, most lesions will spontaneously resolve
within 6–9 months for cutaneous lesions, and longer for mucosal
lesions [10]. More aggressive forms of treatment are needed for
the few recalcitrant variants of LP including hypertrophic type.
Standard therapy for LP includes topical and systemic steroids,
retinoids and PUVA. Acitretin has shown a relatively good efficacy
in the treatment of Hypertrophic LP [11-13].
In our case, patient was symptomatic, and she was treated with
systemic steroid without satisfactory outcome. So, patient had a
choice for systemic retinoid and we observed a very good result
with these drugs.
Discussion
In the medical literature, there is no research report on LP associated with DS. We presented the case to draw attention of the concerned health professional for more research in this arena. At present, the patients of Down syndrome are enjoying a longer life span than before; they deserve the best medical care and quality of life in this 21st century.
References
- Weijerman ME, de Winter JP (2010)The care of children with Down syndrome. European journal of pediatrics169(12): 1445–52.
- Carmelo Schepis, Concetta Barone, MaddaloneSirgnsa (2002) An Updated Survey in Skin Conditions in Down Syndrome. Dermatology 205(3):234-8.
- Dourmishev A,Mitev V, Pramatarov K, Schartz RA (2000) Cutaneous aspect of Down Sundrome. Cutis 66(6):420-4.
- Barankin B, Guenther L (2001) Dermatological manifestations of Down syndrome. J Cutan Med Surg5: 289-93.
- Brown AC, Olkowaski ZL, Mklaren JR, Kutner MH (1977) Alopecia areata and vitiligo associated with Down nsyndrome. Arch Dermatol 113(9):1296.
- Hazini AR, Rongioletti F, Rebora A (1988) Pityriasis rubra pilaris and vitiligo in Down syndrome. Clin Exp Dermatol 13(5): 334-335.
- Shiohara T,Mariya N, Tanaka Y, Arai Y, Hayakawa J, et al. (1988) Immunopathological study of lichenoid skin diseases. Correlation between HLA-DR positive keratinocytes or Langerhans cells and epidermotropic T cells. J Am Acad Dermatol18:67-74.
- MA Kuters,RH Verstegen, EFA Gemen, E de Vries (2009) Intrinsic defect of the immune system in children in Down syndrome: a review. Clin Exp Immunol(2):189-193.
- Le Cleach, Laurence Chosidow, Olivier (2013)"Lichen Planus". New EngJourof Med 366(8): 723–732.
- Scully C, El-KomM (1985)"Lichen planus: review and update on pathogenesis". Journal of Oral Pathology and Medicine 14(6): 431–458.
- Oliver GF,Winklemann RK (1993) Treatment of lichen planus. Drugs45:56-65.
- Alamri A, Alsenaid A, Ruzicka T, Wolf R (2016) Hypertrophic Lichen Planus- Successful treatment with acitretin. DematolTher 29(3): 173-176.
- Vazirnia A, Cohen P (2014) Acitretin for the management of genealized cutaneous lichen planus. Dermatol Online J 20(9):25244164.