Lupine Publishers Group
Lupine Publishers
Research Article(ISSN: 2644-1306) 
Attachment Styles in Relation to Patient Diagnosis in Psychodermatology Volume 1 - Issue 5
Tanyo Tanev*
- Department of Psychology, University of Roehampton, UK
Received:December 13, 2022 Published: February 08, 2023
*Corresponding author:Tanyo Tanev, Department of Psychology, University of Roehampton, London, UK
DOI: 10.32474/TRSD.2023.01.000122
Abstract
Introduction:Despite the availability of research in attachment and psychodermatology, topics regarding the effects of attachment style and its relation to patient diagnosis remain unexplored.
Objectives:The primary objective of this study was to investigate the possible relationships between patient attachment styles and diagnosis.
Methods:Patient diagnosis and demographic information were collected from a clinician-maintained database at a psychodermatology clinic. Participants were randomly selected and placed into one of three diagnostic groups based on their diagnosis. Participants were contacted by telephone and asked to complete the Revised Adult Attachment Scale. Control group responses were obtained by administering an online survey via the social media platforms Facebook and Twitter.
Results:A total of 120 participants took part in the study. There was a statistically significant difference in attachment style between groups as determined by one-way ANOVA. A Tukey post hoc test revealed that the mean attachment style score was statistically significantly lower for patients with the primary dermatological condition, and the Control Group compared to patients suffering from a combination of dermatological and psychiatric conditions.
Conclusion:Statistically significant differences between diagnostic groups and patient attachment styles were noted in this study. Future longitudinal multi-center studies can focus on exploring the effects of life histories, lifestyle choices, and quality of relationships on patients’ diagnoses.
Keywords:Adult attachment; Psychodermatology; Psychology; Psychiatry; Dermatology
Introduction
Relationships are an integral part of human life and have a measurable effect on health [1]. The state of a relationship can be influenced by an individual’s skin conditions [2]. The aspects of adult attachment within the context of skin disease have been investigated for specific conditions, such as the effects of psychosomatic factors on psoriasis [3] and skin barrier recovery [4]. The established relationships point to attachment playing a significant part in such dermatological conditions and general skin health. The increasing popularity of the field of psychodermatology has created a heightened demand for scientifically sound research that examines the interactions of diseases from the fields of psychology, psychiatry, and dermatology [5]. The field’s multidisciplinary core places a unique challenge when it comes to classifying and treating complex disorders. The published studies to date have looked at the effect of attachment on individual skin conditions such as psoriasis [6]. The role of attachment in general dermatology is explored in the study by Szabo [7]. However, studies that specifically look at the entire psychodermatology population are lacking. Several challenges to further research come in the form of financial needs, multi-disciplinary team requirements, and longer-than-usual appointment times [8]. Additionally, there are challenges in obtaining informed consent for randomization and the lack of specialized sites [5]. Recent research into the cost of clinical trials in the UK has revealed median economic costs to be £769,637 [9], which might be difficult to secure in a small and highly specialized field such as psychodermatology. One way to overcome such challenges is for psychodermatology to explore possible patterns of interest within various psychodermatological diseases via smaller pilot studies and then, based on the findings, conduct more detailed research and possibly clinical trials.
The present research aims to investigate the existence of patterns between the attachment styles of psychodermatology patients and their diagnoses. Based on previously found correlations between specific psychodermatological conditions and attachment styles [6,10] the present hypothesis is that clusters of psychodermatological conditions will significantly be associated with attachment styles in adults. For example, earlier studies found that plague psoriasis worsened in patients with attachment-related avoidance and patients with atopic dermatitis showed a higher frequency of insecure attachment than the general population [10]. Interest to this study is any existing relationship between attachment style and general clusters of psychodermatological conditions. The identification of such significant associations or lack thereof will prove useful in several ways. First, it will give more insight into the internal processes involved in psychodermatological conditions as a whole and their relationship to the attachment styles of individuals. Second, it will provide clarity regarding the inclusion of therapeutic methodologies that directly focus on a patient’s attachment style when it comes down to treating psychodermatological conditions.
The additional benefit of researching such associations is the inclusion of psychotherapeutic protocols in the treatment of psychodermatological conditions. Dermatology has already implemented the use of psychotherapies when treating certain disorders such as psoriasis [11]. A favoured treatment methodology is Cognitive-Behavioral Therapy which has spread to the field of psychodermatology and finds use in the treatment of conditions such as psoriasis [12]. The results from the present study will be useful to clinicians by informing them of the various significant associations found between attachment patterns and different psychodermatological disorders which in turn can be used to determine the best treatment for each client. To fill in the gap in the existing literature on the possible connections between attachment style and psychodermatological diagnosis the following research question formed the base for this work: Discussion about the various functions of the skin traces its origin as early as ancient Greece where the Philosopher Aristotle (384-322 BC) was one of the first people to suggest a connection between body and mind, which until then was discrete systems [13]. Fast forward to the present day and research has revealed that both the nervous system and skin develop from the same primary germ layer of an embryo, the ectoderm [14]. Today, the human skin is considered the largest organ of the human body and plays an essential role in protecting it from environmental hazards [15]. The cells of the skin can produce neurotransmitters and neuropeptides, hormones, and their corresponding functional receptors [16]. Earlier research has indicated connections between the immune, and neuroendocrine systems, and the skin [17] therefore placing the skin as a critical median between the environment and the internal organs of the body, allowing it to transmit signals from external stimuli directly to vital organs. This ability of the skin allows it to resist physical stress, toxins, and pathogens and therefore defines it as an immune organ. Findings like this are some of the reasons behind the emergence of the field of psychodermatology, a blend of the fields of psychology, psychiatry, and dermatology [18]. This relatively new area of study concerns itself with matters relating to the interactions between skin and mind and the health conditions related to both those areas.
Currently, there is no widely accepted uniform classification of psychodermatological conditions, and different authors might use designations that slightly differ. One such grouping splits psychodermatological conditions into four main categories [5]. The first category includes psychophysiological disorders or skin diseases that are caused or worsened by psychological stress. With those types of disorders, patients can make a clear association between the times they are stressed and the worsening of their symptoms. Examples of psychophysiological disorders are acne, psoriasis, and seborrheic dermatitis. The second category of conditions is psychiatric disorders with dermatological symptoms which are typically characterized by self-inflicted injury with an underlying psychological condition. Examples of such disorders are delusional parasitosis, body dysmorphic disorder, and an eating disorder. The third category is dermatological disorders with psychiatric symptoms. In such disorders, the emotional impact of a dermatological condition is causing the patient, significant psychological stress. Examples of such disorders are alopecia areata, chronic eczema, and psoriasis. The final category dubbed “Miscellaneous” contains conditions caused or exacerbated by medications or other disorders that do not fit in the previously mentioned groups, such an example being Cutaneous Sensory Syndrome. In a different classification [19] present conditions in the three categories of psychophysiological disorders, primary psychiatric disorders, and secondary psychiatric disorders. Disorders are not limited to a particular category within either of the classifications discussed above, and certain disorders might be found in more than one of the categories.
One example of such overlap is between the psychophysiological category and dermatological disorders with psychiatric symptoms category in one classification [5] for example, psoriasis can be triggered and exacerbated by the stress [20,21] but can also cause significant stress to an individual [22]. This overlap is indicative of the complex nature of psychodermatological conditions, which poses a challenge when treating patients with such conditions [23]. These challenges can be addressed by engaging in scientific research which looks for significant relationships between various aspects of psychodermatological disorders. Since psychodermatology is a field that combines multiple disciplines, it is normal to draw on various theoretical perspectives when solving the main hypothesis of this study. The behavioural neuroscientist Stephen [24] proposed polyvagal theory, the theory states that when people experience stress their sympathetic system is activated. Following this activation, people attempt to activate their social engagement system to relieve stress. That system lets them look for other close individuals who can provide support and protection. This notion overlaps with what we already know about attachment. If findings security in another individual does not work the person prepares to act, also known as the fight or flight response. Finally, if fighting fails and running is not possible the person freezes. The initial response phase is particularly important for this study as it considers the assumptions surrounding adult attachment.
From another perspective, neurodevelopmental studies have shown that inadequate parental care can result in long-term adverse effects on the hypothalamus-pituitary-adrenal (HPA) system regulation in humans [25-27]. Elevated levels of cortisol, a steroid hormone produced by the adrenal gland, were related to slower rates of skin barrier recovery [4]. Attachment-based interventions were found to be beneficial to children, especially regarding the biological regulation of cortisol, thus making their responses appear in line which children who had undergone less difficult childhoods [28]. Research in the medical field has found a significant association between psychopathological symptoms and insecure attachment style, and a negative relationship between quality of life and insecure attachment style [29]. A study looking into dermatology populations similarly found that patients who were found to have a secure attachment style reported greater satisfaction with their visits to a dermatologist [7]. Additionally, patients with secure attachments reported less stressful situations in the past period of six months compared to insecure patients. Walker and Papadopoulos have classified insecure attachment as a vulnerability factor in such patient populations. Research has also investigated the association between attachment style and discrete conditions such as alexithymia, a state where an individual has difficulty identifying and describing feelings [30]. Studies linking alexithymia to insecure attachment with caregivers present further data to be considered [31]. Another psychodermatology condition, plaque psoriasis, was found to worsen in patients with attachmentrelated avoidance [10]. The same study also looked at patients with atopic dermatitis and found a high frequency of insecure attachment.
Those findings suggest that insecure attachment is related to at least some of the conditions in psychodermatology. Currently, studies of the relationship between attachment and illness behaviour and increased vulnerability to stress are limited [32]. Some research findings indicate that individuals who score high on an avoidant attachment or high on anxious attachment have poor adjustment and coping and might find psychological interventions focusing on the attachment style of an individual to be beneficial [33]. The same researchers found that individuals with attachment anxiety used defeatism coping which further perpetuated their distress. The theory proposed by [24] integrates well with [34] attachment theory specifically regarding the need for an individual to seek proximity and protection from other attachment figures. Taking insecure attachment into consideration, the above studies solidify the mind-body connection discussed earlier. The mental internalizations made by people can prevent them from having secure attachment by becoming engrained in the nervous system which leaves them vulnerable to prolonged flight, flight or freeze states or stress. To transfer all that knowledge to psychodermatology, the stressful situations individuals experience in their daily life need to be taken into consideration with the added factor of the psychodermatological condition. Particularly noteworthy is that the standard levels of stress will be higher in insecurely attached individuals due to their impaired ability to cope and reduced ability to access the support of other individuals. Additionally, considering [34] train track idea, a securely attached individual might deviate further from the secure style when exposed to such pressure. To gain a better understanding of the connection between the diagnoses of psycho-dermatology patients and their attachment styles such relationships need to be investigated in more global studies, encompassing the entirety of psychodermatology.
Most of the currently existing literature on the relationship between adult attachment styles and psychodermatological conditions is limited to studies focusing on specific conditions such as atopic dermatitis [35] female alopecia [36] or more general concepts such as chronic skin disease [37] affective touch [38] alexithymia [39] as well as the general role of adult attachment on patients with skin disease [33]. A more recent study has provided a broader examination of the attachment styles in patients in dermatology [7]. The current study aimed to provide an examination of relationships between the attachment styles and diagnosis of patients in psychodermatology. Now, the author is not aware of the existence of other studies that have conducted the same type of examination with similar or different clusters of the psychodermatological population. To examine the entire spectrum of psychodermatological disorders and examine associations with patient attachment style, conditions were grouped into three major clusters based on the review of the previous classifications of psychodermatology discussed earlier. This grouping does not attempt to provide a standard for the classification of psychodermatology conditions. Instead, it aims to create the most encompassing classification for this study by including the entirety of the patient population. The current research explored the existence of any relationships between adult attachment style and the above-mentioned clusters of conditions.
Materials and Methods
A total of 120 participants took part in this study. The sample size was determined based on calculations by G*Power (a commonly used software program for determining statistical power) to obtain an α error of .05. Participants for the diagnostic groups were recruited from The Royal London Hospital in London, UK (TRLH; n = 90) via a specialized psychodermatology clinic. A control group was recruited from the general population via the social media platforms of Facebook and Twitter (n = 30). Participants in the diagnostic groups were sampled to satisfy three primary criteria. First, participants had to be over the age of 18, as this was the required age of providing consent. Second, participants in the diagnostic groups were attending the psychodermatology clinic for treatment of a psychodermatology-related condition. Third, participants were required to have the capacity to provide consent. The participants who were found to not have capacity due to their health or otherwise were excluded. Patient capacity was determined by a consultant liaison psychiatrist and consultant dermatologist operating as part of the multi-disciplinary team at the psychodermatology clinic. The Mental Capacity Act is designed to protect people who may lack the capacity to make decisions about their care and treatment [40]. Patients were assessed on the presence of an impairment that would make them unable to make specific decisions regarding participation in scientific research. Capacity was determined on the bases of file information and previous knowledge of the selected participants. Participants in the control group had only to satisfy the criteria of being over the age of 18 and provide their consent. There was no compensation offered to participants for taking part in this study (Appendix A).
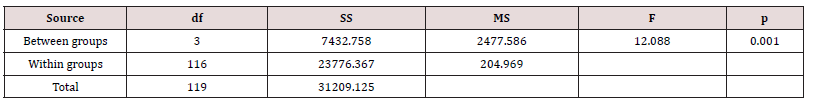
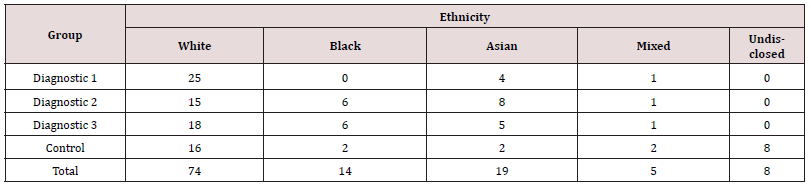
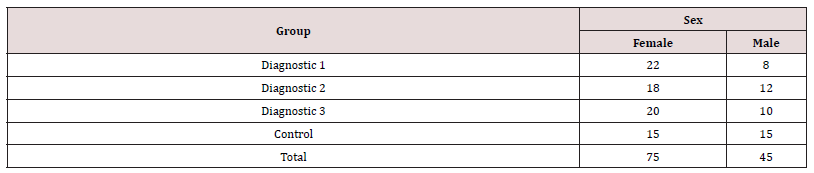
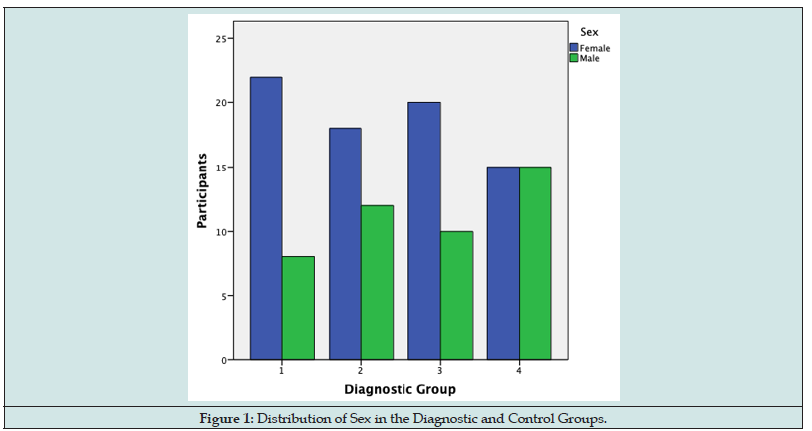
The mean age of participants was 46.13 (sd = 16.19, range = 18 to 93). The sample was mostly female (62.5%), and primarily identified as White (61.7%), Asian (15.8%), Black (11.7%), and mixed race (4.2%). One participant declined to disclose their sex and seven participants declined to disclose information on their ethnicity. Differences in demographic information between the three diagnostic groups and the control group were examined. A one-way between-subjects ANOVA was conducted to examine demographic differences between groups (Table 1). There was a significant effect of age on the Diagnostic Group at the p<.05 level for the four groups (F (3,119) = 12.088, p = .001). A Tukey post hoc test revealed that the control group differed from the diagnostic groups in age, in that they were significantly younger (-11.23 ± -30.50 min, p = .001; -5.83 ±-25.10 min, p = .001; -6.66 ± -25.94 min, p = .001; control group in comparison to Diagnostic Groups 1 (DG1) through 3, respectively). No other statistically significant demographic differences between groups were found. This research project formally commenced following its successful application to the Clinical Effectiveness Unit from The Royal London Hospital (TRLH; ID:9732). A comprehensive database from the psycho-dermatology clinic in TRLH was used in the random selection of participants in the diagnostic groups. The database was created and kept up to date by the clinicians working at TRLH’s psycho-dermatology clinic. Initially, the database contained 1264 entries which were reduced to 1204 after duplicate and incomplete entries were removed.
Following this, numbers from the sequence were assigned at random to one of three diagnostic groups (Appendix B) based on a criterion of patient diagnosis which was included in the database provided by the psychodermatology clinic. The participants assigned to DG1 all met the criteria of having a primary psychiatric condition with secondary dermatological symptoms. Such patients tend to suffer from psychiatric disorders such as body dysmorphic disorder, delusions of parasitosis, and neurotic excoriations which can result in self-inflicted skin injury [5]. Diagnostic Group 2 (DG2) participants met the criteria of having a primary dermatological condition with secondary psychiatric symptoms. Patients in this group present with dermatological conditions that can be exacerbated by stress such as acne [41] or cause stress with their presence such as vitiligo [42]. Diagnostic Group 3 (DG3) included participants with multiple conditions that did not meet the criteria of either group one or group two. DG3 also included a portion of patients that are suffering from chronic lifelong problems such as depression which they have alongside the psychodermatological condition that they bring to the clinic [42] Numbers were selected continuously from the random sequence until each group had 45 participants. Since each group only required 30 participants an extra 15 were added considering potential complications in obtaining data such as the inability to contact some participants or refusal to participate. The sampling method outlined above was done to ensure that all participants had an equal opportunity to participate in this research and to account for potential participants who may decline consent.
The patient diagnosis was determined by the consultant dermatologist and consultant psychiatrist at the TRLH clinic and was included in the patient database. As various diagnoses can be found in the clinic, an information table is included with the conditions that the sampled patient had with a brief explanation of those conditions as well as the frequency of the condition occurring in the sample (Appendix C). Demographic data of the sex, age, and ethnicity of the randomized participants were extracted from the patient database along with the telephone numbers of participants. The randomly selected participants were contacted via telephone by the researcher. Out of respect to the participants in this study, calls were restricted to weekdays between 9 am and 5 pm and no calls were made during weekends or holidays. Each participant was contacted by telephone and given information about the study. Participants who expressed interest in the study but were unable to complete it at the time of the first call were given the option to schedule a different time to complete it. Upon giving verbal consent, the researcher presented participants with the 18 items of the Revised Adult Attachment Scale (RAAS) [43]. Each item was rated on a 5-point Likert scale where 1 stood for “not at all characteristic of me” and 5 stood for “very characteristic of me”. Following the completion of the items participants were debriefed with more information about the study and its future implications, participants were also given time to ask additional questions. A total of 100 potential participants were contacted with ten declining consents (7 in DG1; 3 in DG3).
Control group participants were recruited via a link on social media sites, Facebook, and Twitter. The link contained the 18 items of the RAAS with the addition of 3 demographic questions on sex, age, and ethnicity. The survey questions were administered via SurveyMonkey, an online survey development cloud-based software. When accessing the study online, participants were first presented with information about the study followed by the options to give their consent and take the study or self-select. A total of 35 participants accessed the survey, though 5 participants declined consent and were directed to a thank-you page, thanking them for their time and consideration. Males (n = 15) and Females (n = 15) were equally represented in the control group. Participants primarily identified as White (n = 16), Asian (n = 2), Black (n = 2), and Mixed Race (n = 2). Eight participants decided not to provide information on their ethnicity. Data for the control was recorded and stored in the same way as for the participants contacted by telephone.
Participants in the diagnostic groups were not asked demographic questions. Instead, data on age, gender, and ethnicity were obtained from the database provided by the psychodermatology clinic at TRLH. Detailed demographic information is part of a patient file, and it is assumed that this information is accurate due to the comprehensive requirements placed on hospital administrative procedures. Participants in the control group answered three short questions about the demographic categories: age, gender, and ethnicity. Unlike the diagnostic groups, where demographic information was collected, controls had the option not to provide an answer to some or all the demographic questions, if they so choose.
The Revised Adult Attachment Scale (RAAS) is a standardized tool used for testing an individual’s attachment style. The tool is an 18-item scale based on Hazan and Shaver’s [44] categorical measure. Criticism of the initial measure suggested that the three attachment styles included were mutually exclusive [45- 47] However, [45] developed the Adult Attachment Scale (AAS), a dimensional measure that establishes three scales through factor analysis, in response to the previous criticism. First, the scale measures the extent to which an individual is comfortable with closeness and intimacy (e.g., “I find it relatively easy to get close to others”). Second, the belief of an individual about how dependable others can be (e.g., “I am comfortable depending on others.”). The final dimension is how anxious the individual feels about the possibility of being abandoned or unloved (e.g., “I find that others are reluctant to get as close as I would like.”). AAS is a Likert- type scale and collects quantitative data. The respondents can select a number from 1 to 5 where 1 is “not at all characteristics of me” and 5 is “very characteristic of me”. Collins & Read reported Cronbach’s alpha coefficients of α = .69 for Close, α = .75 for Depend, and α = .72 for Anxiety. Test-retest correlations for 2 months were α = .68 for Close, α = .71 for Depend, and α = .52 for Anxiety. The AAS was further modified in the RAAS by slightly rewording the items to apply to close relationships instead of romantic relationships [45]. This scale is therefore particularly useful for the current study as it looks at attachment in a broader scope, which is important as the study considers the broader scope of social support in close relationships.
Participants were presented with the scale, and the researcher marked their responses next to the 18 items. Each item was marked with a number between 1 and 5. When all data was collected, seven items are recorded in reverse order (Appendix F; AT8R, AT13R, AT17R, AT2R, AT7R, AT16R, AT18R) as directed by the author of the scale [45]. Following this, three attachment dimensions were computed and labelled: CLOSE, DEPEND, and ANXIETY. The CLOSE and DEPEND dimensions can further be combined into the CLOSEDEP dimension. Those computed dimensions can be used to compute the attachment style of participants by using cut-off scores on each of those dimensions. For example, if a participant’s score is greater than 3 on the CLOSEDEP dimension and less than 3 on the ANXIETY dimension, then the participant is assigned the secure attachment style. The validity and reliability of the RAAS have been additionally tested and found to be significant by a detailed metaanalytical study of all attachment instruments produced in the last 25 years [48]. The study reviewed the validity and reliability of 29 different instruments and provided a detailed review of 11 scales that were deemed to have strong psychometric properties, extensive use, or use in psychosomatic research. The RAAS was included in this selection, highlighting its reliability and validity in various settings. The reviewers caution that the use of each scale needs to carry considerations of the study it is being used for, which is the case for the present research.
Another reason for selecting the RAAS for this study was its ease of use in a telephone interview, due to its relatively short length compared to other instruments such as the 40-item Attachment Style Questionnaire [49] and the 36-item Close Relationships Scale [46]. The Avoidant Attachment Questionnaire for Adults was a similar tool that was also considered [50] however, it was dismissed due to validity and reliability concerns from previous findings. Other scales measuring attachment, such as the Current Relationship Interview [51-53] Secure Base Scoring System and Couple Attachment Interview focus on attachment concerning one partner or spouse, which is not the focus of this research. Accordingly, they were not selected for use in the current study. A limitation of this study was the use of a phone interview. Previous studies suggest that participant responses could vary over the phone to make themselves appear different than they are [54] however, those findings have been disputed [55]. Due to the time limitation, data collection in psychodermatology clinics was inadequate because of the relatively limited number of clinics during the data collection period, and the inability to conduct a truly random study. This is a particularly important constraint in psychodermatology, as patients often have high rates of missed appointments [56].
The limitations can be addressed in future longitudinal studies that provide written questionnaires to participants and allow them to complete them anonymously. Additional restrictions have been presented in the face of using the Revised Adult Attachment Scale (RAAS). Due to the lack of a single defining scale that measures attachment and the different schools of thought on the role of attachment, the scale used will continue to present a challenge. Replications of the current study with the same and different scales will provide relevant information about the reliability and validity of those instruments in a psychodermatology population. Another constraint was the exclusion of participants under the age of 18, due to the study being conducted in a predominantly adult clinic. The existence of specific pediatric psychodermatology clinics is rare and even a more significant challenge to research and collect data from than adult clinics. Future studies that employ a longitudinal model and potentially could pool data from multiple clinics would be able to look into this. Such studies will need to have the attachment scales they use adjusted for pediatric populations.
Finally, the quantitative nature of data collection presents a limitation to the study. Future studies could use instruments such as the 20-item Adult Attachment Interview [57] or create an entirely new instrument specifically for the psychodermatology population. Such instruments were impractical for the current research, mostly due to time limits. Additionally, it is not known how psychodermatology patients would respond to such forms of questioning, which tend to take significantly more time than a short quantitative scale to complete. The above analysis focused on answering the research hypothesis that a possible relationship exists between certain groups of psychodermatological conditions and attachment styles. The RAAS was found to be an appropriate scale to measure attachment style regarding the sample of participants while taking into consideration that the study focused on the extended range of close personal relationships and not just romantic once. Participants (n = 90) were selected from a large pool (n = 1204) that included various diagnoses found in psychodermatology. Controls (n = 30) were gathered via a survey online. Data collection of the RAAS was conducted over the phone. Obtained data were scored by the recommendations given by the author of the scale [47]. Based on the scoring participants were assigned one of four attachment styles.
Results
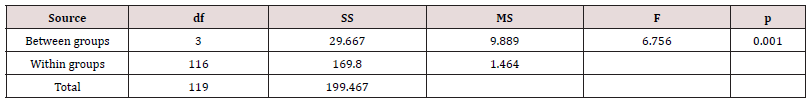
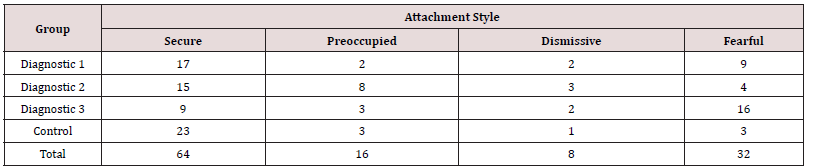
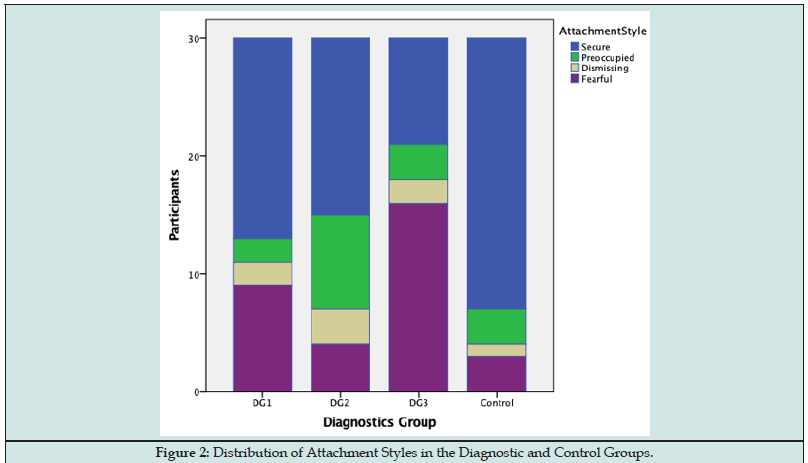
The current research aimed to examine if differences exist between the patient diagnostic group and participant attachment style in psychodermatology. There was a statistically significant difference in attachment scores of the diagnostic plus control groups as determined by one-way ANOVA (F (3,116) = 6.756, p = .001). A Tukey post hoc test revealed that the mean attachment style score was statistically significantly lower for Diagnostic Group 2 (DG2; 1.87 ± 1.07, p = .013) and the Control Group (CG; 1.47 ± .97, p = .000) compared to Diagnostic Group 3 (DG3; 2.83 ± 1.37) [58]. There was no statistically significant difference between Diagnostic Group 1 (DG1) and the CG (p = .184), DG2 (p = .878), and DG3 (p = .093). Taken together, these results suggest that people from the general population as well as those suffering from dermatological conditions with psychological impact have a smaller attachment style score than patients who have multiple psychological and dermatological conditions. Specifically, the results suggest that a difference exists between patient attachment style and diagnostic groups (Figure 1). Additionally, differences in demographics between the three diagnostic groups and the control group were examined. A one-way between-subjects ANOVA was conducted to examine Demographic differences between groups (Table 1). There was a significant effect of Age on the Diagnostic Group at the p<.05 level for the four groups (F (3,119) = 12.088, p = .001) (Table 2). A Tukey post hoc test revealed that the control group differed from the diagnostic groups in age, in that they were significantly younger (-11.23 ± -30.50 min, p = .001; -5.83 ± -25.10 min, p = .001; -6.66 ± -25.94 min, p = .001; control group in comparison to diagnostic groups 1 through 3, respectively). No statistically significant variations in participant ethnicity or sex were found. Frequencies of those two demographic dimensions can be found in (Table 3) and (Table 4) below. It is important to note the prevalence of participants who identified as white (n = 74, 61.67%). Also, the number of participants identified as female (n = 75, 62.5%). (Figure 2) shows the trend of having more female participants in diagnostic groups compared to the control.
The following four sections of this chapter examine the prevalence of the four attachment styles (secure, preoccupied, dismissing, and fearful) in each of the diagnostic groups and the control group. Each section begins with a description of the discussed attachment style [59]. Earlier research on attachment is reviewed in a top-down manner by looking at studies of the general population, then moving to studies on attachment in dermatology and finally to specialized subpopulations. Each subsection concludes with an examination and discussion of the present finding by making evaluations about the prevalence of attachment styles in each diagnostic group. The impact of the limiting factors in this research on the outcomes is taken into consideration and discussed. Additionally, suggestions are made about future research or clinical improvements that can be made based on the findings of the present study. The final sections of this chapter discuss the general implications of the findings of this study within dermatology and psychodermatology [60]. Additionally, the overlaying limitations are discussed in consideration of future studies. Suggestions about the direction research can take following the obtained results in this study are also given with regard and focus on the field of psychodermatology and the inclusion of interventions based on the results from this study.
Participants with secure attachment style.
[52] summarize four prototypic attachment styles derived from the dimensions of anxiety and avoidance. Individuals with a secure attachment style are those who are low in both anxiety and avoidance. Such individuals feel respected by others and have a positive predisposition towards their attachment figures; they are comfortable getting close to others and depending on them [61]. Earlier research shows that between 55% [43], 56% [24], and 59% of the general population exhibit a secure attachment style(Table 5). Within a population of dermatology patients, a sizeable multi-nation study found that 68.7% had a secure attachment style [7]. In the current study, a total of 64 (53.33%) securely attached individuals were found in the sample with most located in the control (n = 23) and the least found in DG3 (n = 9). A visual representation of the distribution of styles per group can be seen in (Figure 1) where securely attached individuals are presented in blue. The rate of securely attached respondents in the current study is below average among both the general and dermatological populations; this is not surprising, however, considering the conditions included in each group and the effects they have on participants. The lower rate of securely attached individuals could be related to the prevalence of chronic illness in individuals which an earlier study found to be 36% [37]. Interpretation of the results, particularly for securely attached individuals, needs to be done carefully due to the tendency of psychodermatology patients to dismiss any psychological factors to their conditions and instead insist the conditions are caused entirely by physiological or external factors [19].
Therefore patients, particularly in DG1 and DG3, could potentially dismiss any factors linked to their mental health and account for psychological issues by attributing them to environmental or physiological causes. The dismissiveness can be due to the long time spent going from clinic to clinic and trying to manage and treat their condition, which may have resulted in general mistrust in clinicians [62,63]. This is most applicable to DG1, which primarily included participants suffering from delusional parasitosis (n = 17) and dermatitis artefacta (n = 4). Both conditions include a strong belief of external factors are the reason for the condition and a refusal to accept other explanations. Admittance of relationship difficulties could be seen as psychological disturbance by the patient, as it is something that has been implied or directly said to them by healthcare providers in the past. In such a scenario it is not unlikely for the patient to augment their responses to be more in line with their distorted self-image [64]. Therefore, when considering previous studies on psychodermatological conditions, it is possible that secure attachment style representation in DG1 and DG3 could be exaggerated. Future studies can address this by examining the participant attachment style with more nuanced scales, to circumvent the possibility of patients responding desirably. This potentially calls for the development of an attachment scale that targets populations whose delusional beliefs can affect the genuineness of their responses, as well as the general population, to reduce response bias.
Participants with preoccupied attachment style
Individuals with a preoccupied attachment style are those who score high on anxiety but low on avoidance. Individuals look to the opinion of others for their self-esteem, they seek closeness and intimacy but are not confident that others will adequately respond to their needs and fear rejection and abandonment [52]. Earlier research on a large sample of the general population has shown that 11% had an anxious attachment. Those findings need to be considered with caution; however, since the application of various models of attachment and their respective testing instruments could potentially result in errors due to their inability to overlap entirely. Still, [46] comment that the preoccupied attachment style is like Hazan and Shaver’s anxious-ambivalent category which found 19% of the population to have that attachment style [44]. Within a population of dermatology patients, it has been found that 9% had a preoccupied attachment style [7]. The current study found 16 (13.33%) participants to have a preoccupied attachment style with half of them located in Diagnostic Group 2 (DG2) and the rest spread evenly between the other groups and control. Participants in this group had primary dermatological conditions with secondary psychiatric symptoms such as anxiety and depression based on their dermatology conditions.
The preoccupied participants are visually represented in (Figure 1) with the colour green. The more extensive representation of individuals with a preoccupied attachment style contrasts with the other three groups, which appear to have a similar distribution. It is also interesting that DG2 contains individuals with primary dermatological conditions. It is unclear if the chronic dermatological conditions have a direct impact on the anxiety dimension of the RAAS or if preoccupied individuals who are already high on anxiety are more vulnerable to such chronic dermatological conditions. A causal relationship cannot be drawn; however, this leaves the question open for future studies to answer. Limitations to obtaining exact values could have been presented in the phone interview, where participants would answer more in line with their distorted image of reality [64]. [52] Note this can also be characteristic of preoccupied individuals since they value themselves less than others and could potentially augment their responses to appear more competent than they are. Since DG2 can easily be generalized to general dermatology, further studies need to explore the potential relationship between preoccupied attachment style and skin health. One recommendation this study can make is the utilization of more attachment-based treatment of patients in general dermatology, specifically those who have a preoccupied attachment style.
Participants with a dismissing-avoidant attachment style
Dismissing-avoidant individuals are characterized by being low in anxiety but high in avoidance [52]. They tend to be confident and feel that they cannot be affected by negative feelings. They perceive attachment figures as unreliable and unresponsive. Dismissing participants were evenly represented amongst groups. Since most studies look at avoidance as one dimension, data on how many people in the general population have this particular attachment style was not found, however, in the dermatology population 15.3% of patients have been found to have that particular attachment style [7]. Dismissing-avoidant individuals were the least represented in the sample (n = 8; 6.67%) and are defined, coloured in tan, in (Figure 1). Due to the individuals being low in anxiety it can be assumed that such individuals will not be as concerned about their dermatological issues in the same way participants in the other diagnostic group will.
Additionally, their high avoidance could make them less likely to trust professionals such as psycho-dermatologist which in turn results in a small sample [65]. One possibility to consider is that such individuals might be avoiding seeing a specialist and this could result in them being under-represented. One way to address this is to launch a psycho-dermato-educational program for the general public informed about various skin conditions and how specialty clinics are established to help with them, perhaps giving them the option to self-refer after having read about the types of treatment offered instead of being “given” a diagnosis and being sent to a specialist could result in higher representation. It also needs to be considered that the group could be small relative to the rest and is accurately represented.
Participants with a fearful-avoidant attachment style
Fearful-avoidant individuals are characterized by being high in both anxiety and avoidance [52]. Such individuals have a strong sense of distrust which goes alongside expectations of being rejected. They are uncomfortable with intimacy and avoid close and intimate relationships. In a large dermatology patient population, fearful-avoidant attachment individuals consisted of 6.9% [7]. Participants with fearful-avoidant attachment style accounted for the second largest group after secure attachment style in the study (n = 32; 26.67%), second to individuals with secure attachment style. They were mostly found in DG 3 (n = 16) and DG 1 (n = 9). Interestingly, the second most prevalent style in the study was fearful-avoidant. First, its prevalence is several times higher than in the general dermatology population. Second, the description of fearful-avoidant individuals can easily be transferred to the majority of psychodermatology patients [66].
Psychodermatology patients are also described to be highly anxious about their condition and to be particularly reluctant to any psychological treatment [19], offered by the psychodermatology team or their social support. In the present study, such individuals were also mostly found in groups that included primary psychiatric conditions (DG1 and DG3) even though this does not present causation between such conditions it opens the door for future studies that can examine it. These findings confirm the personality patterns that previous research has found in psychodermatology patients with primary psychiatric conditions. More surprising is the high prevalence of this attachment style in DG3 where participants had mixed conditions. A potential conclusion from this is that long-term conditions in psychodermatology that are associated with psychiatric symptoms are also related to fearful-avoidant attachment style
General implications of the findings.
Psycho-dermatology deals with a wide range of conditions. This study alone included individuals suffering from over 25 different conditions. The significant association found between different diagnostic groups should be enough to stimulate two kinds of action. First, it should allow for future studies to build upon and expand on the findings of the current research. More specifically such research can continue to explore the relationship between various diagnostic groups and patient attachment styles. Second, it should enable health professionals to provide better services by presenting them with further knowledge of participants’ interpersonal coping mechanisms or their lack thereof. The findings of this study can also help supplement attachment theory by expanding it to the specific patient subpopulation. They can also be tested against future studies which use different measuring instruments of attachment.
Limitations to findings and alternative interpretation of results
The current data is specific to a single center of psychodermatology in the United Kingdom. This has undoubtfully created some limitations and the general ecological validity of the findings. Thus, the results are mostly applicable in large urban centers within the United Kingdom and can be generalized to demographically similar centers in Western Countries. [62] Found that within Canada, those likely to be in a lower socioeconomic group were significantly less likely to visit a dermatologist for a specialist consultation. This reduced representation of socioeconomic groups and overrepresentation of others could affect the outcomes of studies in Canada, and possibly other Western countries [67]. To overcome this limitation, a multi-national study needs to be carried out in various countries that also account for cultural differences. Additionally, consideration needs to be made about the effects of patient conditions on their responses, particularly in the groups containing primary psychiatric conditions. Patients could be answering in a way closer to their perception of self that could significantly differ from reality [64]. This can be addressed by contrasting the obtained results with data from previous medical examinations [65], or using behavioural observations whenever possible [12]..
Discussion
This study shows that the mixed-diagnosis group of psychodermatological disorders had significantly different attachment styles in comparison to the other diagnostic groups and the control group. The findings add to previous dermatological studies examining the aspects of attachment patterns within the context of discrete conditions such as psoriasis [6,3], skin barrier recovery [4], and atopic dermatitis by looking at the entire spectrum of psychodermatological conditions. The current study also confirms the previously established relationships between psychodermatological conditions and insecure attachment [6]. by showing that different diagnostic clusters are associated with insecure attachment styles. The study also adds to more general research exploring attachment relationships in general dermatology [7] by focusing on the subfield of psychodermatology. Patient diagnosis and demographic information were retrieved from a database created and updated by the clinicians at the site. Participants were randomly selected and placed in one of three diagnostic groups based on their diagnosis. Participants were then contacted by telephone and asked questions from the Revised Adult Attachment Scale [47]. A control group was used by administering an online survey to the social media platforms Facebook and Twitter containing the same questions as the diagnostic groups. A total of 120 participants took part in this study.
There was a statistically significant difference in attachment scores of the diagnostic plus control groups as determined by oneway ANOVA (F (3,116) = 6.756, p = .001). A Tukey post hoc test revealed that the mean attachment style score was statistically significantly lower for Diagnostic Group 2 (1.87 ± 1.07, p = .013) and the Control Group (1.47 ± .97, p = .001) compared to Diagnostic Group 3 (2.83 ± 1.37). There was no statistically significant difference between Diagnostic Group 1 and the Control Group (p = .184), Diagnostic Group 2 (p = .878), and Diagnostic Group 3 (p = .093). Taken together, these results suggest that people from the general population as well as those suffering from dermatological conditions with psychological impact have a smaller attachment style score than patients who have multiple psychological and dermatological conditions. Specifically, the results suggest that a difference exists between patient attachment style and diagnostic groups. The identification of significant associations can prove useful in several ways. First, as an educational device to clinicians and researchers, about the patterns of attachment found in the psychodermatological population and the ability to relate that information to the psychodermatology population. Second, it can be used to guide future research that looks to further delve into the relationship between attachment style and psychodermatological diagnosis. Third, it provides an argument for or against the inclusion of specific attachment-based treatment patterns in the holistic treatment plan of psychodermatology patients.
The current use of psychotherapy in psychodermatology is considered to further extend the third point above. Psychodermatology has already implemented the use of psychotherapies when treating certain disorders such as psoriasis [11]. The results of the current research could prove useful in implementing psychotherapeutic protocols when treating psychodermatological conditions. Such can extend to the widely used and popular treatment methodologies of Cognitive-Behavioral therapy, which has already spread to the field of psychodermatology and is used for the treatment of several conditions including psoriasis. Additionally, treatment modalities can consider more general approaches that explain the interaction of perceived dangers and their effect on the nervous system [24]. and base new treatments particularly tailored for the psychodermatology population. Implementation of such protocols based on the findings of the present study will be useful in providing therapists and clinicians with further information on the interaction of various psychodermatological diseases which can be used in determining factor of the best therapy to be used for each client. This research will also enable psychodermatology to move to a more holistic treatment modality [68].
The present study comes with several limitations regarding the methodology that was used. First, the use of telephone interviews could be a limitation as participants could alter their responses to make themselves appear better than they are in reality [54] however those findings have been disputed [55]. Second, due to the existing time limitation on data collection attending psychodermatology clinics to administer the Revised Adult Attachment Scale was inadequate because of the few numbers of clinics available [58] and the reduced possibility of pure randomization of participants. Those limitations must be addressed in future longitudinal studies that provide written questionnaires to participants who can then complete them anonymously. Due to the lack of a single defining scale that measures attachment and the different schools of thought on the role of attachment the scale will continue to present a challenge [67]. Another constraint was the exclusion of participants below the age of 18. The existence of specific pediatric dermatology clinics is rarely making it a more significant challenge to research and collect data compared to adult clinics [60]. Future longitudinal multi-center studies can focus on exploring the effects of life histories, lifestyle choices, and quality of relationships on patients’ diagnoses.
Acknowledgments
I would like to express my sincere gratitude to Dr. Anthony Bewley and the psychodermatology team at The Royal London Hospital for providing the site and their expertise for this study. It was Dr. Bewley who sparked my interest in psychodermatological research, observing and learning from him has been one of the most significant educational milestones in my career.
References
- Uchino BN (2004) Social Support and Physical Health: Understanding the Health Consequences of Relationships.
- Bewley A (2017) The neglected psychological aspects of skin disease. BMJ: Clinical Research (Online) pp. 358.
- Janković S, Raznatović M, Marinković J, Maksimović N, Janković J, Djikanović B et al. (2009) Relevance of psychosomatic factors in psoriasis: a case-control study. Acta dermato-venereologica 89(4): 364-368.
- Robles T F, Brooks K P, Kane HS, Schetter CD (2013) Attachment, skin deep? Relationships between adult attachment and skin barrier recovery. International Journal of Psychophysiology 88(3): 241-252.
- Jafferany M, Franca K (2016) Psychodermatology: basics concepts. Acta dermato-venereologica 96(217): 35-37.
- Picardi A, Mazzotti E, Gaetano P, Cattaruzza MS, Baliva G, Melchi CF et al. (2005) Stress, social support, emotional regulation, and exacerbation of diffuse plaque psoriasis. Psychosomatics 46(6): 556-564.
- Szabó C, Altmayer A, Lien L, Poot F, Gieler U et al. (2017) Attachment styles of dermatological patients in Europe: a multi-centre study in 13 countries. Acta dermato-venereologica 97(6-7): 813-818.
- Marshall C, Taylor R, Bewley A (2016) Psychodermatology in clinical practice: main principles. Acta dermato-venereologica 96(217): 30-34.
- Hind D, Reeves B C, Bathers S, Bray C, Corkhill A, Hayward C, Tremain L (2017) Comparative costs and activity from a sample of UK clinical trials units Trials 18(1): 203.
- Rabung S, Ubbelohde A, Kiefer E , Schauenburg H (2004) Bindungssicherheit und Lebensqualität bei Neurodermitis. PPmP-Psychotherapie· Psychosomatik· Medizinische Psychologie 54(08): 330-338.
- Price ML, Mottahedin I, Mayo PR (1991) Can psychotherapy help patients with psoriasis? Clinical and Experimental dermatology 16(2): 114-117.
- Sambhi R, Lepping P (2010) Psychiatric treatments in dermatology: an update. Clinical and Experimental Dermatology: Experimental dermatology 35(2): 120-125.
- França K, Chacon A, Ledon J, Savas J, Nouri K (2013) Pyschodermatology: a trip through history. Anais brasileiros de dermatologia 88(5) : 842-843.
- Gilbert SF (2001) Ecological developmental biology: developmental biology meets the real world. Developmental biology 233(1): 1-12.
- Kanitakis J (2002) Anatomy, histology and immunohistochemistry of normal human skin. European journal of dermatology: EJD 12(4): 390-9.
- Slominski A (2005) Neuroendocrine system of the skin. Dermatology 211(3): 199-208.
- Salmon JK, Armstrong CA, Ansel JC (1994) The skin as an immune organ. Western journal of medicine 160(2): 146.
- Jafferany M (2007) Psychodermatology: a guide to understanding common psychocutaneous disorders. Primary care companion to the Journal of clinical psychiatry 9(3): 203.
- Koo J, Lebwohl A (2001) Psychodermatology: The Mind and Skin Connection. American family physician, 64(11):1873-1878.
- Basavaraj KH, Navya MA, Rashmi R (2011) Stress and quality of life in psoriasis: an update. International journal of dermatology 50(7): 783-792.
- Farber EM, Nall L (1993) Psoriasis: a stress-related disease. Cutis 51(5): 322-326.
- Kimball AB, Jacobson C, Weiss S, Vreeland MG, Wu Y (2005) The psychosocial burden of psoriasis. American journal of clinical dermatology 6(6): 383-392.
- Harth W, Gieler U, Tausk FA, Kusnir D (2009) The difficult or impossible-to-treat problem patient. Clinical Management in Psychodermatology 261-264.
- Porges SW (2011) The polyvagal theory: neurophysiological foundations of emotions, attachment, communication, and self-regulation. WW Norton, Company.
- Heim C, Nemeroff C B (1999) The impact of early adverse experiences on brain systems involved in the pathophysiology of anxiety and affective disorders. Biological Psychiatry 46(11): 1509-1522.
- Heim C, Newport DJ, Bonsall R, Miller AH, Nemeroff CB (2001) Altered pituitary-adrenal axis responses to provocative challenge tests in adult survivors of childhood abuse. The American Journal of Psychiatry, 158(4): 575-581.
- Buss C, Lord C, Wadiwalla M, Hellhammer D, Lupien et.al (2007) Maternal care modulates the relationship between prenatal risk and hippocampal volume. The Journal of Neuroscience 27(10): 2592-2595.
- Dozier M, Peloso E, Lewis E, Laurenceau JP, Levine S (2008) Effects of an attachment-based intervention on the cortisol production of infants and toddlers in foster care. Development and Psychopathology 20(3): 845-859.
- Barbosa F, Freitas J, Barbosa A (2011) Chronic idiopathic urticaria and anxiety symptoms. Journal of health psychology 16(7): 1038-1047.
- Taylor GJ (1984) Alexithymia: Concept, measurement, and implications for treatment. The American Journal of Psychiatry 141(6): 725-732.
- Picardi A, Pasquini P, Cattaruzza MS, Gaetano P, Baliva G, Melchi CF, Biondi M (2003) Only limited support for a role of psychosomatic factors in psoriasis: Results from a case-control study. Journal of psychosomatic research 55(3): 189-196.
- Kotler T, Buzwell S, Romeo Y, Bowland J (1994) Avoidant attachment as a risk factor for health. British Journal of Medical Psychology 67(3): 237-245.
- Krasuska M, Lavda AC, Thompson A R, Millings A (2018) The role of adult attachment orientation and coping in psychological adjustment to living with skin conditions. British Journal of Dermatology 178(6): 1396-1403.
- Bowlby J (1973) Attachment and loss:2. Separation: anxiety and anger.
- Dieris-Hirche J, Milch WE, Kupfer J, Leweke F, Gieler U (2012) Atopic Dermatitis, Attachment and Partnership: A Psychodermatological Case-control Study of Adult Patients. Acta dermato-venereologica 92(5): 462-466.
- Schmidt S (2003) Female alopecia: the mediating effect of attachment patterns on changes in subjective health indicators. British Journal of Dermatology 148(6): 1205-1211.
- Schmidt S, Nachtigall C, Wuethrich-Martone O, Strauss B (2002) Attachment and coping with chronic disease. Journal of Psychosomatic Research 53(3): 763-773.
- Krahé C, Drabek MM, Paloyelis Y, Fotopoulou A (2016) Affective touch and attachment style modulate pain: a laser-evoked potentials study. Philosophical Transactions of the Royal Society B: Biological Sciences 371(1708): 20160009.
- Ozuguz P, Kacar SD, Alpaslan AH, Celep B, Uzel H (2016) Evaluation of Alexithymia in Patients Admitted to the Dermatology Clinic. International Neuropsychiatric Desease Journal 5(3): 1-8.
- Jones RM, Piffaretti E (2005) Mental capacity act manual. Sweet, Maxwell, USA.
- Polenghi MM, Zizak S, Molinari E (2002) Emotions and acne. Dermatology and Psychosomatics/Dermatologie und Psychosomatik 3(1): 20-25.
- Salman A, Kurt E, Topcuoglu V, Demircay Z (2016) Social anxiety and quality of life in vitiligo and acne patients with facial involvement: a cross-sectional controlled study. American journal of clinical dermatology 17(3): 305-311.
- Tohid H, Aleem D, Jackson, C (2016) Major depression and psoriasis: a Psychodermatological Phenomenon. Skin pharmacology and physiology 29(4): 220-230.
- Hazan C, Shaver P (1987) Romantic love is conceptualized as an attachment process. Journal of personality and social psychology 52(3): 511-524.
- Collins N L, Read SJ (1990) Adult attachment, working models, and relationship quality in dating couples. Journal of personality and social psychology 58(4): 644-663.
- Brennan L, Clark C, Shaver P (1998) Self-report measurement of adult attachment. In J. A. Simpson, WS Rholes (Eds.) Attachment Theory and Close Relationships.
- Collins N L (1996) Working models of attachment: Implications for explanation, emotion, and behaviour. Journal of Personality and Social Psychology 71(4): 810-832
- Ravitz P, Maunder R, Hunter J, Sthankiya B, Lancee W (2010) Adult attachment measures: A 25-year review. Journal of psychosomatic research 69(4): 419-432.
- Feeney J A, Noller P, Hanrahan M (1994) Assessing adult attachment: developments in the conceptualization of security and insecurity. In: Sperling MB, Berman WH, editors. Attachment to adults: theory, assessment, and treatment 128-152.
- West M, Sheldon-Kellor A E (1992) The assessment of dimensions relevant to adult reciprocal attachment. Canadian Journal of Psychiatry 37(9): 600-6.
- Crowell J, Owens, G (1996) Current Relationship Interview and scoring system. Unpublished manuscript
- Collins N L, Feeney BC (2004) Working models of attachment shape perceptions of social support: evidence from experimental and observational studies. Journal of personality and social psychology 87(3): 363-383.
- Cohn D A, Silver, D H (1992) Working models of childhood attachment and couple relationships. Journal of Family Issues 13(4): 432-49.
- Garbett R, McCormack B (2001) The experience of practice development: An exploratory telephone interview study. Journal of Clinical Nursing 10: 94-102.
- Opdenakker R (2006). Advantages and disadvantages of four interview techniques in qualitative research. In Forum Qualitative Sozialforschung/Forum: Qualitative Social Research 7(4).
- Orion E, Feldman B, Ronni W, Orit BA (2012) A Psychodermatology Clinic. American journal of clinical dermatology 13(2): 97-101.
- George C, Kaplan N, Main M (1996) Adult Attachment Interview. Unpublished manuscript.
- Aguilar‐Duran S, Ahmed A, Taylor R & Bewley A (2014) How to set up a psychodermatology clinic. Clinical and experimental dermatology 39(5): 577-582.
- Bewley A, Taylor RE, Reichenberg JS & Magid M (Eds.) (2014) Practical Psychodermatology.
- Burns EA, Finlay A, Barrett M, Baselga E, Basra MK et al (2012) Pediatric Psychodermatology: a clinical manual of child and adolescent psychocutaneous disorders. Walter de Gruyter.
- Galen L W (2012) Does religious belief promote prosociality? A critical examination. Psychological Reports, 138(5), 876-906.
- Haider A, Mamdani M, Shaw JC, Alter DA & Shear NH (2006) Socioeconomic status influences care of patients with acne in Ontario, Canada. Journal of the American Academy of Dermatology 54(2): 331-335.
- Harth W, Gieler U, Kusnir D & Tausk FA (2008) Clinical management in psychodermatology.
- Paulhus D L & Vazire S (2007) The self-report method. In R. W. Robins, R. C. Fraley (Eds.), Handbook of research methods in personality psychology 224-239.
- Podsakoff PM, MacKenzie SB, Lee JY & Podsakoff NP (2003) Common method biases in behavioral research: A critical review of the literature and recommended remedies. Journal of Applied Psychology 88(5): 879-903.
- Ranson KE & Urichuk LJ (2008) The effect of parent-child attachment relationships on child biopsychosocial outcomes: a review. Early Child Development and Care 178(2): 129-152.
- Roisman GI, Holland A, Fortuna K, Fraley RC, Clausell E & Clarke A (2007) The Adult Attachment Interview and self-reports of attachment style: An empirical rapprochement. Journal of personality and social psychology 92(4): 678-697.
- Taylor R E, Bewley A & Melidonis N (2006) Psychodermatology. Psychiatry 5(3): 81-84.