Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1644
Short CommunicationOpen Access
Skin disorder in pregnancy Volume 2 - Issue 4
Myat San Yi1*, Mi Mi Khaing1 and Mon Mon Yee2
- 1University of Malaysia, Malaysia
- 2Newcastle University, Malaysia
Received: July 22, 2019; Published: July 30, 2019
Corresponding author: Myat San Yi, University of Malaysia, Sarawak, Malaysia
DOI: 10.32474/OAJRSD.2019.02.000143
Abstract
Pregnancy is a turning point in women’s life. There are so many physiological changes preparing the mother to adapt to the fetus. The change in the woman’s immune system, with a shift from a predominantly T helper 1 lymphocyte profile to a T helper 2 profile, may underlie a woman’s susceptibility to skin disease [1]. There are other factors like endocrine, metabolic, mechanical, and vascular changes which influence on skin changes [2].
Skin is a barrier and a front-line defense against the invasion of microorganisms. Its integrity provides the physical barrier as it contains the important bioactive molecules such as defensins and Cathelicidins. The presence of the skin microbiota made up of microorganisms such as Staphylococcusepidermidis, Propionibacteria,Corynebacteria and negative Coagulase staphylococci play their role to prevent the invasion from various organisms[3].Still, the skin changes or diseases in pregnancy will challenge the medical professionals in primary care. It may be due to limited teaching in medical school over this specific area. Most practitioners including,we feel unprepared or unconfident once addressed to these cases.This short communication is intended to cover the physiological skin changes in pregnancy and to tackle the case with systematic history taking and competent clinical examination. These factors, together with appropriate laboratory tests, can help the clinician achieve the correct diagnosis, and point towards the identification of the underlying causative agent.
Literature Review
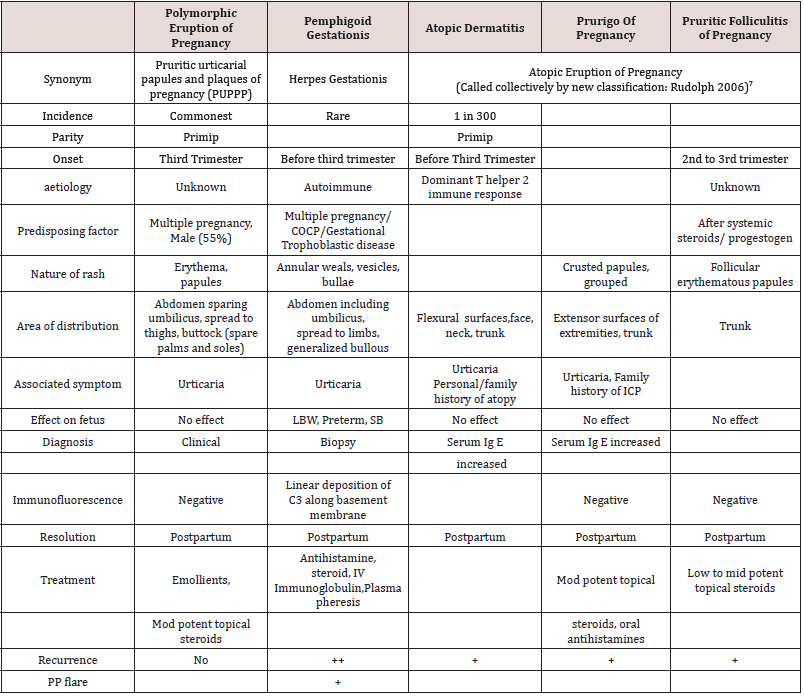
They are categorized into three types in general: normal physiological changes or benign skin conditions, exacerbations of preexisting conditions triggered by pregnancy, and specific dermatoses of pregnancy [4,5].The normal physiological changes are hyperpigmentation, hair changes, nail changes and pruritus gravidarum (common in the first and second trimester) and some glandular changes like increased activity in sweat glands and sebaceous glands. These changes are caused by increased secretion of pituitary Melanocyte- Stimulating hormone, steroids and pregnancy hormones such as estrogens and progesterone. The preexisting conditions like psoriasis improves in most of the cases. Eczema and atopy are commonly exacerbated by pregnancy. There are other skin conditions like acne vulgaris, scabies and fungal infection which may exacerbate during the pregnancy. The dermatoses of pregnancy are assumed to be developed from changes in immunologic, hormonal and metabolic system [6]. Their characteristics are summarized in the following (Table 1).
Practical Approach
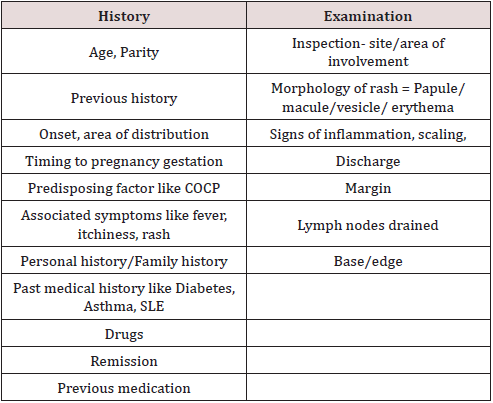
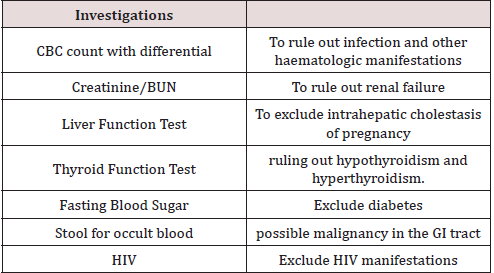
Tables 2 & 3) Dermatologists input is very important and helpful as skin biopsy for histopathological examination and immunofluorescence test to exclude specific skin disease. Treatment consists of simple measures like avoiding the irritants, applying emollients and symptomatic treatment like antihistamines. Steroids play an important role in the management. There are concerns over the safety of steroids usage in pregnancy. Recent evidence showed that there was no association between maternal use of topical steroids and orofacial cleft, preterm delivery or fetal death. There was a significant association between fetal growth restriction and maternal use of potent and ultra-potent topical steroids. Therefore, the recommendation is to use topical corticosteroids at the lowest potency possible to control the condition being treated. The risk of adverse effects increases with potency and the amount and length of time used [8-15].
Conclusion
In conclusion, interdisciplinary approach with involvement of obstetricians, paediatricians, dermatologists and physicians will lead to achieve the best outcome in their management. Early recognition, timely referral and adequate, effective treatment will reduce the short-term and long-term morbidity in both mother and foetus.
References
- Vaughan S, Ambrosrudolph C (2014)Skin disease in pregnancy.BMJ348:3489.
- DavisM,Brost B (2010)Skin diseases in pregnancy EBSCO eBook Collection EBSCOhost De Swiets. Medical disorder in pregnancy.
- RuoccoE, Donnarumma G, BaroniA, Tufano M A (2019) Bacterial and Viral Skin Diseases.Dermatologic Clinics 25(4): 663-676.
- WangwA R,KroumpouzosG (2019) Obstetrics: Normal and Problem Pregnancies (7thedn).Skin Disease and Pregnancy.
- RapiniR P (2019) Creasy and Resnik’s Maternal-Fetal Medicine: Principles and Practice (8thedn). The Skin and Pregnancy.
- MTunzi,GR Gray (2007) Common skin infections in pregnancy.American Family Physician 75(2): 211-218.
- C M AmbrosRudolph, RR Müllegger, SAVaughanJones, HKerl, MMBlack (2006)The specific dermatoses of pregnancy revisited and reclassified: results of a retrospective two- center study on 505 pregnant patients. Journal of the American Academy of Dermatology54(3): 395-404.
- JonesSV, AmbrosrudolphC, Nelsonpiercy, C (2014). Skin disease in pregnancy.BMJ 348:3489.
- Chi CC, Kirtschig G, Aberer W, Gabbud JP, Lipozencic J,etal. (2011)Evidence- based guideline on topical steroids in pregnancy. Br J Dermatol 165(5): 943-952.
- Sävervall C, Sand F L, ThomsenSF (2015) Dermatological Diseases Associated with Pregnancy: Pemphigoid Gestationis, Polymorphic Eruption of Pregnancy, Intrahepatic Cholestasis of Pregnancy and Atopic Eruption of Pregnancy. Dermatol Res Pract, pp. 1-8.
- Bremmer M, Driscoll M S, Colgan R (2010)skin disorders of pregnancy: A management guide. OBG Manag 22(6):24-33.
- Morgan M (2017)Challenging infections in pregnancy: a multiparametric approach. Obstetrics Gynaecology and Reproductive Medicine27(9): 266-276.
- AlabdulrazzaqF(2012)Mother risk Update Topical corticosteroid use during pregnancy. Can Fam Physician 58(6):643-644.
- Oakley A (2009)Topical steroids treatment for skin conditions. Best Practice Journal (23): 8-13.
- Ambrosrudolph, C M (2011)Dermatoses of Pregnancy - Clues to Diagnosis, Fetal Risk and Therapy. Ann Dermatol 23(3): 265-275.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...