Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1644
Review ArticleOpen Access
Mondor Phlebitis (Mondor’s disease) of the Penis: A Review and Update of the Literature Volume 2 - Issue 5
Anthony Venyo*
- North Manchester General Hospital, Department of Urology, Manchester, United Kingdom
Received: February 25, 2020; Published: March 12, 2020
Corresponding author: Anthony Venyo North Manchester General Hospital, Department of Urology, Manchester, M8 5RB, United Kingdom
DOI: 10.32474/OAJRSD.2020.02.000147
Abstract
Mondor’s disease of the penis (MDP) is an uncommon disease which tends to affect sexually active males whose ages have tended to range between 18 years and 70 years, but it could manifest in younger and older males. MDP may present with a throbbing and aching painful dorsal induration that had involved the penis, a painful swelling of the penis which had ensued a laborious coital activity, The finding of a firm, sub-cutaneous cord-like structure or structures, that tend most often to be parallel to the coronal sulcus, The dorsal midline of the shaft of the penis as well as the foreskin could be affected by the disease which has produced firm cord-like structures, Tenderness and pain within the penis could occur in few cases especially during erection, painful lumps within the penis that may be present for a period of short time to few years in chronic cases. Isolated MDP may mimic Peyronies’s disease, laceration of corpus cavernosum and polyarteritis nodosa. Similar penile lesions of the penis could be on rare occasions be seen in associated with deep vein thrombosis, or a palpable cord-like lesion on the dorsum of the penis that has arisen within 24 hours to 48 hours of prolonged coital activity but the duration could be longer. Some of the possible aetiological factors of MDP include:
a) Trauma due to prolonged or vigorous coital activity, trauma to the penis, fracture of the penis, prolonged abstinence
from coital activity, utilization of vacuum device for coitus.
(b) Infection due to syphilis, Candida infection of the penis, sexually transmitted infection, Behcet’s disease.
(c) Pursuant to surgical operation including repair of inguinal hernia, orchidopexy, varicocelectomy;
oncological causes related to malignancy.
(d) Other causes including intracavernosal injection of drugs and tendency to thrombosis.
Diagnosis of MDP tends to be based upon the history and clinical examination findings and the diagnosis can be confirmed by utilization of ultrasound scan of the penis that shows upon Doppler scan no evidence of blood flow through the superficial dorsal vein and the ultrasound scan also shows thrombus within the superficial dorsal vein of penis. Treatment of MDP does involve expectant / non-surgical treatment with utilization of anti-inflammatory medicaments / topical heparin and majority cases do resolve within 4 to 8 weeks spontaneously. The medicaments would tend to ameliorate the symptoms, but they tend not to affect or influence the rate of resolution of MDP. Surgical intervention in the form of thrombectomy or resection of the thrombosed dorsal vein of penis does lead to be undertaken in cases of persistent symptoms and non-resolution after 6 weeks of conservative treatment as well as for cases of chronic disease and resolution of the MDP does ensue the surgical treatment. Clinicians need to carefully differentiate MDP from Peyronie’s disease, fracture of the penis and sclerosing lymphadenitis of the penis and thrombosis of the vein of the penis associated with generalized thrombosis including deep vein thrombosis, and malignancy. MDPs that are associated with treatable inflammatory conditions that may occur would also need to be treated additionally for the associated conditions.
Keywords: Mondor’s disease of penis; Superficial dorsal vein of penis; Thrombosis; Non-steroidal anti-inflammatory drugs; Topical heparin; Thrombectomy; Vein resection, Superficial thrombophlebitis of penis, Non-venereal sclerosing lymphangitis of penist
Introduction
Mondor phlebitis of the penis is a terminology that is utilized for an uncommon and most often transient condition that manifests as a cord-like lesion of the penis [1]. It has been stated that the incidence of Mondor’s disease of the penis (MDP) could be greater than that reported in view of the embarrassing nature of the complaint and the often-frequent spontaneous resolution of the disease [2]. The largest reported series of MDP to be reported in the literature contained 25 cases of MDP [2, 3]. MDP has been stated to tend to occur in men who are sexually active of any age, but the ages of the patients have tended to range between 18 years and 70 years [2-5]. MDP can mimic other diseases and considering that only few cases of MDP have been reported in the literature, there is the possibility that difficulties could may arise with regard the diagnosis of some cases of MDP that are encountered by clinicians who have never seen a case of MDP before. The ensuing review and update of the literature on MDP is divided into two parts (A) Overview and (B) Miscellaneous narrations and discussions from some case reports, case series and studies related to Mondor’s disease of the penis (MDP).
Aim
To review and update the literature on Mondor’s Disease of the penis.
Method
Internet data bases were searched including: Yahoo, Google; Google Scholar; and PUBMED. The search words that were used included: Mondor’s Disease of Penis, superficial thrombophlebitis of penis, non-venereal sclerosing lymphangitis of penis, penile Mondor’s disease. Thirty one references were identified which were used to write the review and update of the literature of the disease in two parts (A) Overview and (B) Miscellaneous narrations and discussions related to some case reports, case series and studies related to Mondor’s disease of the penis.
Review and Update of the Literature
Overview
Definition / General comment: Mondor phlebitis of the penis is a terminology that refers to a rare and most often transient condition that manifests as a cord-like lesion of the penis [1].
Terminology: Some of the terminologies that have been utilized for Mondor phlebitis include [1]:
a) Superficial thrombophlebitis of the penis.
b) Mondor disease
c) Non-venereal sclerosing lymphangitis (an incorrect
terminology).
Epidemiology
a) Mondor phlebitis is said to most often affect young men as well as middle-aged men who are sexually active [1].
b) It has been iterated that the incidence of Mondor phlebitis of 1% has been documented in patients who have been seen in sexually transmitted diseases (STD) clinic [1-6].
Sites: It has been documented that Mondor phlebitis of the penis does tend to afflict the superficial dorsal vein of the penis [1].
Aetiology
a) It has been iterated that as a sequel of massive thrombosis
of the superficial venous plexus of the penis there tends to be
the formation of a firm, subcutaneous cord-like structure or
structures along the shaft of the penis or around the coronal
sulcus [1].
b) With regard to the causation of Mondor phlebitis the
ensuing causations have been documented [1]:
i. Neoplasm.
ii. Mechanical trauma to the penis during vigorous /
strenuous coital activity following sexual abstinence.
iii. Sickle cell disease [7]. This was a report of a sickle cell
episode that had manifested with superficial thrombophlebitis
of the penis in a patient who received an anti-inflammatory
medicament and who was reassured that the disease was
benign. The lesion resolved within 6 weeks.
iv. Long period of airline flight [8]. This case report involved a
patient who developed Mondor’s disease of the penis 24 hours
ensuing a 15-hour flight. The patient also did report having
developed superficial thrombophlebitis (STP) of his left lower
limb varicose veins that ensued a similar flight three years
earlier. In the absence of any other predisposing factor it was
promulgated that long-haul flight is an important contributing
factor for the emanation of thrombosis of the superficial dorsal
vein of the penis.
v. A complication of Varicose vein surgery [9].
vi. Herpes simplex infection [2].
vii. Trauma to the penis [2].
viii. Fracture of the penis [2].
ix. Utilization of vacuum device for coitus [2].
x. Infection due to syphilis, Candida infection of the penis,
sexually transmitted infection, Behcet’s disease [2].
xi. Pursuant to surgical operation including repair of inguinal
hernia, orchidopexy, varicocelectomy [2].
xii. Oncological causes related to malignancy [2].
xiii. Other causes including intracavernosal injection of drugs
and tendency to thrombosis [2].
Clinical manifestations
a) Some of the documented manifestations of Mondor phlebitis include [1]:
i. The finding of a firm, sub-cutaneous cord-like structure
or structures, that tend most often to be parallel to the coronal
sulcus.
ii. The dorsal midline of the shaft of the penis as well as the
foreskin could be affected by the disease producing the firm
cord-like structures.
iii. Tenderness and pain within the penis could occur in few
cases especially during erection.
iv. Mondor phlebitis has been stated to be almost invariably
self-limiting with an associated spontaneous regression within
4 weeks to 8 weeks; nevertheless, the disease tends to be
associated with a lot of psychological stress.
Laboratory examination findings
a) Urine
Urinalysis, urine microscopy, culture and sensitivity are general tests that tend to be undertaken in the general assessment of patients who have MDP and the results would tend to be normal but if there is any infection this would be appropriately treated to improve upon the general condition of the patient but the results would not be diagnostic of MDP.
Laboratory blood tests
a) Haematology
i. Full blood count and coagulation screen are general tests that tend to be undertaken in the general assessment of patients who have MDP and the results would tend to be normal but if there is any impairment in the results this would be investigated and appropriately treated to improve upon the general condition of the patient but the results would not be diagnostic of MDP.
ii. It has been stated that blood tests for the investigation for an increased tendency for the formation of thrombosis tends to be rarely required [2-10].
b) Biochemistry
i. Serum urea, electrolytes, blood glucose and liver function tests are general tests that tend to be undertaken in the general assessment of patients who have MDP and the results would tend to be normal but if there is any impairment in the results this would be investigated and appropriately treated to improve upon the general condition of the patient but the results would not be diagnostic of MDP.
c) Radiology imaging
iii. It has been stated Colour Doppler ultrasound scan of
the penis is the key investigation that tends to be used to
differentiate MDP from non-venereal sclerosing lymphangitis
[2].
iv. With regard to cases of MDP, it has been iterated that
ultrasound scan of the penis would tend to show signs of
venous thrombosis including no evidence of colour filling or
flow within the lumen of the superficial dorsal vein which tends
to be associated with a low-speed, high-resistance flow pattern
within the cavernous arteries [11].
d) Diagnosis
i. Diagnosis of MDP tends to be based upon a good clinical
history and clinical examination finding in which the patients
do tend to manifest with a palpable cord-like lesion, which
almost invariably tends to be upon the dorsum of the penis
which most often would be noted to have arisen 24 hours to
48 hours pursuant to vigorous or prolonged coital activity
[2]. It has also been stated that clinical examination could
demonstrate a lesion which could be tender as well as cause an
episodic pain that tends to be worsened during erection [2]. It
has been documented that one case of MDP has been reported
to be asymptomatic [2,6].
ii. It has been documented that clinical examination of the
penis in cases of MDP would tend to show a lesion upon the
dorsum of the penis that tends to measure between 2 cm and
10 cm in length [2-10].
iii. It has also been stated that the overlying penile skin in
cases of MDP tends to be tethered and at times erythematous
and that the cord-like penile lesion could run longitudinally or
transversely as well as distal penile lesions of MDP could often
give the appearance of a double coronal sulcus [2-6].
e) Treatment
i. It has also been iterated that the treatment of MDP generally tends to be entirely symptomatic and that patients who have MDP could be managed expectantly [2]
ii. Additionally, patients who have MDP often to require explanation related to the fact that MDP is a benign disease which must be properly and adequately explained to them to reassure them [2].
iii. With regard to reported cases of MDP in the literature, the
reported patients have been frequently provided non-steroidal
anti-inflammatory medicaments which have been illustrated
to be effective for the therapy of the acute penile discomfort; however, the anti-inflammatory medicaments have tended not
to have any effect on the rate of the resolution of the disease
[2,12].
iv. Topical heparin creams have been utilized which had
not illustrated any significant improvement upon the rate of
resolution of the MDP [3].
v. With regard to refractory cases of MDP, surgical
intervention had been undertaken. Thrombectomy or resection
of the dorsal vein of the penis could be undertaken and these
surgical treatment options quite often tend to be offered
to patients who have been symptomatic whose symptoms
have failed to improve pursuant to 6 weeks of non-operative
management [3].
f) Macroscopic features: It has been iterated that upon gross visual and palpation examination of the penis of individuals who have Mondor phlebitis, there tends to be found a firm, subcutaneous cord-like structures along the dorsal aspect of the shaft of the penis or around the coronal sulcus [1].
g) Microscopic histopathology examination features
1. The microscopy pathology examination features of the
lesion in Mondor phlebitis does include the ensuing [1]:
a. The finding of prominent vessels that contain plump
endothelial cells as well as thickened (sclerotic) blood vessel
walls which mainly tend to be veins with the occasional vessel
that exhibit complete occlusion of its lumen,
b. The finding of perivascular inflammatory infiltrate, which
is comprised of lymphocytes, histiocytes, as well as plasma
cells.
c. There tends to be no evidence of lymphatic involvement
of the disease process.
2. It has also been iterated that pathology examination of the resected thrombosed veins would tend to show an increased amount of connective tissue within wall of the vein together with swelling of the endothelial cells, and intraluminal thrombus, and within the perivascular region an infiltration of lymphocytes, histiocytes as well as plasma cells could be visualised. [2,10]
h) Differential diagnosis
1. The differential diagnoses of Mondor phlebitis include:
a. Cutaneous polyarteritis nodosa. It has been stated that
with regard to polyarteritis nodosa involving the penis, microscopy
pathology examination of a specimen of the penile lesion would
tend to reveal vasculitis that has involved small and medium sized
arteries of the dermis as well as the subcutaneous tissue. [1]
b. Peyronies disease.
c. Fracture of the penis.
Outcome
With regard to outcome of MDP the ensuing iterations have
been made:
i. MDP tends to be a self-limiting disease and majority of
cases tend to resolve spontaneously within 4 weeks to 8 weeks.
[2, 6, 12]
ii. Episodes of recurrence of MDP have been reported that
have been associated with sexual intercourse. [6, 12]
Miscellaneous narrations from some case reports, case series, and studies related to Mondor phlebitis of the penis
Kumar et al. [6] reviewed documentations related to all patients who had attended their sexually transmitted diseases clinic between 1991 and 2003 that were examined for evidence of Mondor’s disease of the penis. They stated that detailed history as well as the clinical findings of the patients were recorded in a specially designed proforma as well as histopathology examination and immunohistochemistry staining studies with utilization of monoclonal antibodies for CD 31 and CD 34 were undertaken with regard to 11 patients. With regard to the results, Kumar et al. [6] reported that 18 out of 1296 patients who had attended their sexually transmitted diseases (STD) clinic during the period were diagnosed as having Mondor’s disease of the penis which had given an incidence of 1.39%. Seventeen of the patients did have a history of one or more than one episode of sexually transmitted diseases (STDs). Microscopy histopathology examination of the specimen did illustrate prominent vessels that had plump endothelial cells as well as thickened blood vessel walls. The pathology examination also showed an occasional vessel that was associated with complete occlusion of its lumen. Kumar et al. [6] made the ensuing conclusions:
1) With regard to their study, they did not find any evidence
of lymphatic involvement.
2) Non-lymphatic vessels, mainly veins, had been most
predominantly involved.
3) In their opinion Mondor’s phlebitis of the penis or
Mondor’s disease of the penis are better terminologies to
describe the disease instead of non-venereal sclerosing
lymphangitis.
Nazir and Khan [13] reported an 18-year-old male who had manifested with a history of a throbbing and aching painful dorsal induration that had involved the proximal one third of his penis over the preceding one week. He was asymptomatic otherwise. He stated that he had a recent non-traumatic masturbation. He had not had a sexually transmitted disease. His general and systematic examinations were normal. A thin ropy cord lesion was palpated superficially on the dorsal aspect of his penis. The palpable cord had included a dilated portion that measured about 0.6cm in diameter. The indurated cord could be followed up superiorly and it had extended into his pubic hair region by 2 to 3cm. Upon palpation, the cord was tender and the overlying skin was completely intact with no evidence of erythema. There was no evidence of lymph node enlargement or hernia within his groins. A clinical diagnosis of superficial thrombophlebitis of the dorsal vein of his penis was made. He had doppler ultrasound scan of his penis see Figure 1 showed a dorsal induration which corresponded to segmental thrombosis of the superficial dorsal vein of the penis and the rest of the trajectory did remain permeable. He received supportive care which had included Diclofenac 50 mg orally twice daily, oral enteric coated aspirin 325 mg daily for anticoagulation, ofloxacin 200 mg orally twice daily for prophylaxis, as well as heparin cream for local application for 4 weeks. The pain subsided and the induration disappeared. He was advised to refrain from coital activity until his induration and symptoms had subsided.
Figure1: Ultrasound of the superficial vein of the penis demonstrating thrombosis. Reproduced from: Nazir SS, Khan M [13]. Thrombosis of the dorsal vein of the penis (Mondor’s Disease): A case report and review of the literature. Indian Journal of Urology 2010 Jul-Sep; 26(3): 431–433. DOI: 10.4103/0970-1591.70588 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2978449/ Under copyright © Indian Journal of Urology This is an open-access article, distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited. Accessed 2020 Feb 04 Bird et al. [14] in 1997, reported an uncommon case of traumatic thrombophlebitis of the superficial dorsal vein of the penis (TSDVP) in a taxi driver which followed repeated injury to his penis by a coin-filled pouch.
Rodríguez Faba et al. [15] reported a 41-year-old man who had manifested with pain as well as induration of the dorsal aspect of his penis. Based upon his clinical examination findings and upon echo-doppler scan features of his penis a diagnosis of Mondor’s disease was made. His treatment included utilization of nonsteroidal anti-inflammatory agent, and antibiotics. Rodríguez Faba et al. [15] made the ensuing conclusions:
1) Dorsal vein thrombosis of the penis is a very uncommon
disease that is associated with pain and induration of the dorsal
vein of the penis.
2) The aetiology of Mondor’s disease of the penis does
include traumatic origin, neoplastic origin, excessive sexual
activity, and abstinence from sexual activity.
3) Sclerosing lymphangitis of the penis is a differential
diagnosis of Mondor’s disease of the penis.
4) Doppler ultrasound scan of the penis is useful with regard
to the confirmation of the diagnosis of Mondor’s disease of the
penis.
5) The treatment Mondor’s disease of the penis depends
upon utilization of non-steroidal anti-inflammatory agents,
and antibiotics for infection. Local application of heparin could
be useful and the undertaking of surgery with thrombectomy
resection tends to be reserved for persistent disease.
Sasso et al. [16] reported 10 patients who during the preceding 3 years were treated for superficial penile vein thrombosis. The ages of the patients had 20 years and 57 years and their mean age was 35 years. They reported that the main aetiology factors of the disease had included prolonged and excessive sexual intercourse, operations for inguinal hernia, and deep vein thrombosis. All of the patients had reported that they had noticed sudden and almost painless cord-like induration on the dorsal aspect of the penis. Doppler ultrasound scan of the penis was useful with regard to the diagnosis of the disease as well as in the follow-up assessment of the patients. Eight of the patients were treated by means of nonsteroidal anti-inflammatory drugs (NSAIDs) and anti-platelet drugs. With regard to the results, Sasso et al. [16] reported that the mean interval to the resolution of symptoms was 3 weeks. Two of the patients who did not respond to drug treatment did undergo surgery which had involved resection of dorsal vein of penis. Sasso et al. [16] concluded that medical treatment, and when required, resection of vein are successful and effective with regard to the treatment of Mondor’s disease of the penis.
Swierzewski et al. [12] reported superficial dorsal vein thrombosis 8 times that had occurred in 7 patients whose mean age was 27 years and whose ages had ranged between 19 years and 40 years. They stated that all of the patients had related the onset of thrombosis of the dorsal vein of penis to vigorous sexual intercourse. No other aetiological factors were found in the assessment of the patients. Three of the patients did receive acute treatment with anti-inflammatory medicaments and four of the patients were treated expectantly. They reported that the mean interval to resolution of the disease was 7 weeks. The mean followup of the patients was 11 months and the follow-up had ranged between 3 months and 30 months at which time all of the patients had reported normal erectile function. Only 1 of the patients did develop recurrent thrombosis 3 months pursuant to his initial episode of thrombosis of the dorsal vein of penis, which again was related to sexual intercourse. Swierzewski et al. [12] made the following conclusions:
a) Mondor’s phlebitis is a benign self-limited condition.
b) Anti-inflammatory medicaments are useful for the
treatment of acute discomfort, but they do not affect the rate of
resolution of the disease.
Singla et al. [17] reported a 37-year-old man who had manifested with a painful dorsal induration of his penis over the preceding 4 days. He described his penile pain as throbbing in nature. He was asymptomatic otherwise. He did not report any history of recent trauma, vigorous coital activity, or utilization of penile constricting devices. His general and systematic examinations were normal. There was evidence of a tender, cord-like swelling upon the dorsal surface of his penis that had extended from his glans penis to his supra-pubic region. There was no evidence of groin lymph node enlargement. The results of his routine blood biochemistry and haematology tests including his coagulation screen were normal. He had Doppler ultrasound scan of his penis which demonstrated a non-compressible, superficial dorsal vein, and lack of venous flow signals. Based upon the features of the penile lesion a provisional diagnosis of thrombosis of the superficial dorsal vein of the penis was rendered and conservative management was adopted with utilization of heparin ointment and non-steroidal anti-inflammatory medication that comprised of aceclofenac. He was advised to refrain from coital activity and to attend for review assessment in 1 month. During his assessment at his 1-month follow-up his clinical examination did demonstrate complete resolution of the swelling. He had a repeat Doppler ultrasound scan of his penis which illustrated restoration of normal blood flow within his dorsal vein of penis. Some of the iterations made by Singla et al. [17] included the ensuing:
1. In 1939, Henri Mondor described a case of sclerosing
thrombophlebitis of the subcutaneous veins of the anterior
thoracic wall, and in 1955, Braun-Falco did report phlebitis of
the dorsal veins of the penis within the context of generalized
phlebitis. [18, 19]
2. Isolated Mondor’s disease of the penis was first
documented in 1958 by Helm and Hodge [20].
3. Various causative factors for the development of Mondor’s
disease of the penis include: trauma of the penis, excessive
sexual activity, prolonged abstinence from sex, infection, pelvic
tumours, utilization of constrictive devices during certain types
of sexual practices. Out of the aforementioned factors, trauma
that is caused by sexual intercourse does appear to be the main
aetiology factor. This could be due to the stretching as well as
torsion of the veins of the penis that cause denudation of the
endothelium and the subsequent release of thromboplastic
substances which could activate the coagulation cascade [21].
4. Additionally, Mondor’s disease of the penis had been
documented pursuant to long-haul flights [8], as well as a rare
presentation of metastatic adenocarcinoma of the pancreas, as
well as an idiopathic entity.
5. The diagnosis of Mondor’s disease of the penis tends to
be mainly based upon the clinical examination finding and the
diagnosis based upon clinical examination can be supported
/ confirmed by utilization of Doppler ultrasound scan of the
penis [22].
6. Treatment of Mondor’s disease of the penis tends to be
mainly the conservative treatment option and many conservative
treatment options have been proposed for the disease. It is
important to note that anticoagulation with utilization of
aspirin, heparin, or other anti-platelet medicaments would
not expedite the process of healing and these would tend not to be necessary with regard to the prevention of additional
development of thrombosis. Antibiotics could be utilized as
prophylactic treatment to avoid infection. Non-steroidal antiinflammatory
medicaments (NSAIDs) could be utilized to
relieve pain, and for their anti-inflammatory action. Patients
who develop Mondor’s disease of the penis should be advised
to avoid sexual intercourse as well as masturbation.
7. With regard to majority of cases of Mondor’s disease of
the penis, the symptoms tend to resolve completely within 6
weeks to 8 weeks. With regard to Mondor’s disease of the penis
that do not resolve despite conservative management option,
it has been recommended that excision of the thrombus, or
excision of the vein should be undertaken [21]. Such surgical
procedures could relieve pain as well as diminish induration of
the skin, and they would tend to produce aesthetically pleasing
results.
8. The differential diagnoses of Mondor’s disease of the
penis does include sclerosing lymphangitis, Peyronie’s disease,
and fractured penis [13].
Ouattara et al. [23] reported a 34-year-old married man with four women, who was a healthy trader who was admitted as an emergency following a painful swelling of his penis which had ensued a laborious coital activity. His symptoms began 9 days later with progressive painful swelling at his balanopreputial ring after sexual intercourse. He had received treatment in a private clinic without improvement in his symptoms and he was admitted because of generalized involvement of his entire penis with painful oedema. He did not have any significant symptoms but stated he was married with four wives and had been having vigorous sexual intercourse activities. His clinical examination demonstrated an indurated subcutaneous filiform and painful cord, which was palpable at the dorsal root of his penis and a soft swelling of his entire penis see Figure 2. Examination of his genitourinary tract was normal.
Figure 3: Doppler coupled with USS showing an intraluminal thrombosis (weight arrow) of the dorsal vein of the penis.
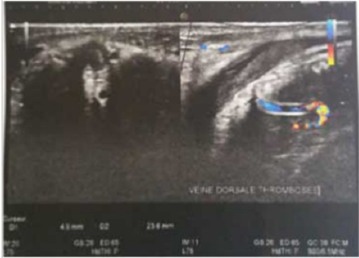
Figure 2 Generalized swelling of the penis. Reproduced from: [23] Ouattara A, Paré A K, Kaboré A F, Yaméogo C, Botcho G, Ky D, Ouédraogo AA, Bako A, Kiba R, Nikiéma Z, Kambou T. Subcutaneous Dorsal Penile Vein Thrombosis or Penile Mondor’s Disease: A Case Report and Literature Review. Case Reports in Urology Volume 2019; Article ID 1297048: 3 pages. https:// doi.org/10.1155/2019/1297048 https://www.hindawi.com/ journals/criu/2019/1297048/ under copyright © 2019 Adama Ouattara et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. The results of his urinalysis, urine microscopy and culture, routine blood haematology and biochemistry tests were all normal. A provisional diagnosis of fracture of the penis was considered, nevertheless, the patient did not experience a popping sound or hear a cracking sound or experience loss of erection during his coital activities. Based upon this a secondary diagnosis of thrombosis of the dorsal vein of the penis was made. He underwent Doppler ultrasound scan of his penis which demonstrated thrombosis of the superficial dorsal vein of his penis and presence of intravascular blood clot thrombosis (Figure3).
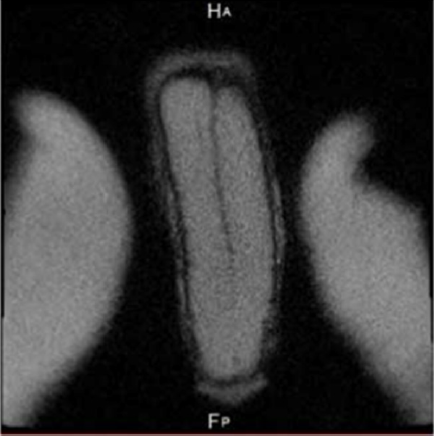
Figure 3 Doppler coupled with USS showing an intraluminal thrombosis (weight arrow) of the dorsal vein of the penis. Reproduced from: Reproduced from: [23] Ouattara A, Paré A K, Kaboré A F, Yaméogo C, Botcho G, Ky D, Ouédraogo AA, Bako A, Kiba R, Nikiéma Z, Kambou T. Subcutaneous Dorsal Penile Vein Thrombosis or Penile Mondor’s Disease: A Case Report and Literature Review. Case Reports in Urology Volume 2019; ArticleID1297048:3pages. https://doi.org/10.1155/2019/1297048 https://www.hindawi. com/journals/criu/2019/1297048/ under copyright © 2019 Adama Ouattara et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. In order to exclude the possibility of an associated fracture of the penis (laceration of the corpus cavernosum), a magnetic resonance imaging (MRI) scan of the penis was undertaken which did not demonstrate any traumatic lesion of the corpus cavernosum or corpus spongiosum (Figure 4).
He received conservative treatment which consisted of nonsteroidal anti-inflammatory medications (NSAID) and acetyl salicylic acid 100 mg per day with the aim of preventing thrombosis by coagulation and inhibition of platelet aggregation. He was advised to refrain from coital activities until his symptoms had completely resolved. His penile pain disappeared in 8 weeks as well as the swelling had reduced, and complete and total recovery of the penis was noted. At his 6-months follow-up he was well without any development of recurrence of his disease. A lesson that can be learnt from this case report is that Doppler ultrasound scan of the penis is useful for the confirmation of the diagnosis of Mondor’s disease of the penis but when a clinician is not absolutely sure whether or not there is an associated injury to the corpus cavernosum or corpus spongiosum then MRI scan of the penis or CT scan of the penis can be undertaken to exclude injury to the corpora whilst these images would also confirm thrombosis of the superficial dorsal vein of the penis. Ouattara et al. [23] iterated that antibiotics tends to be used in cases of Mondor’s disease of the penis associated with cellulitis or sexually transmitted diseases (STDs) until there is remission of symptoms. Nazir and Khan [13] had found that utilization of local anaesthesia infiltration of bupivacaine 0.5% around the thrombosed area considerably relieved pain.
Figure 4 MRI of penis showing the integrity of the cavernous bodies. Reproduced from: Reproduced from: [23] Ouattara A, Paré A K, Kaboré A F, Yaméogo C, Botcho G, Ky D, Ouédraogo A A, Bako A, Kiba R, Nikiéma Z, Kambou T. Subcutaneous Dorsal Penile Vein Thrombosis or Penile Mondor’s Disease: A Case Report and Literature Review. Case Reports in Urology Volume 2019; Article ID 1297048: 3 pages. https://doi.org/10.1155/2019/1297048 https://www.hindawi.com/journals/criu/2019/1297048/ under copyright © 2019 Adama Ouattara et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Pittaka et al. [24] reported a 62-year-old man who had a cT4 anal cancer (infiltration of corpora spongiosa and penile bulb), that was associated with extensive loco-regional lymph node enlargement, who had developed painful lumps within the midline of his anterior penile surface when he was receiving radical chemotherapy and radiotherapy. His clinical examination demonstrated two palpable cord-like swellings that were located 2 cm from his pubic symphysis. He had Colour Doppler ultrasound scan of his penis which confirmed the diagnosis of Mondor’s disease. He was successfully treated with non-steroidal anti-inflammatory medicaments. The causative factors for the development of the Mondor’s disease were malignancy of a pelvis organ and radiotherapy. The diagnosis of Mondor’s disease of the penis did prove challenging to the authors in view of the fact that Mondor’s disease of the penis is an uncommon disease and the fact that the differential diagnosis of the lesion did include progression of the malignant anal disease. Pittaka et al. [24] iterated that their reported case was the first case of Mondor’s disease of the penis to be reported in a patient with carcinoma of the anus who has been undergoing chemotherapy.
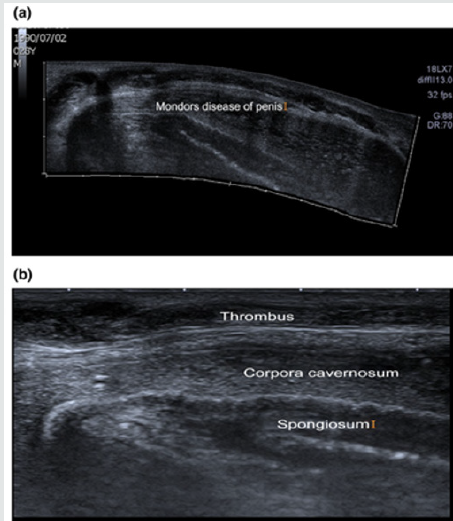
Mukendi and Mahlobo [25] reported a 29-year-old man who had manifested with a 1-week history of painful penis which did worsen with morning erections. He did report vigorous sexual intercourse 2 days preceding the onset of his symptoms. Examination of his penis demonstrated an 8 cm hard cord-like as well as mildly tender structure upon the dorsal surface of his penis that had extended from the base of his penis to the corona of his penis (Figure 5). He had Doppler ultrasound scan of his penis (CDU) which showed a thrombosed superficial dorsal vein of penis with a thrombus visualised from the base of the penis to the junction of the shaft of the penis and the glans of the penis. There was no venous flow detected upon Doppler scanning (Figure 6A & 6B) in keeping with Mondor’s disease of the penis. He received anti-inflammatory medicament of indomethacin 50 mg orally three times per day and topical heparin gel application twice daily. At his 2-week follow-up he did report resolution of his pain he defaulted further followup. Mukendi and Mahlobo [25] iterated that surgical management tends to be offered to patients who have Mondor’s disease with regard to cases that have proven to be refractory to medical treatment which tends to be defined as persistent symptoms and no evidence of venous flow upon Colour Doppler ultrasound (CDU) scan of the penis following six weeks of medical treatment and the surgical treatment does consist of thrombectomy and resection of the superficial vein of the penis [10].
Figure 5 Penile image showing a dilated and tortuous superficial dorsal vein of penis. Reproduced from: [25] Mukendi A M, Mahlobo F. Penile Mondor’s disease: Clinical and sonographic images. Clinical Case Reports. 2019 Nov; 7(11): 2283-2284. https://doi.org/10.1002/ccr3.2469. https://onlinelibrary.wiley. com/doi/full/10.1002/ccr3.2469 Accessed 2020 Feb 05. Under copyright © 2019 The Authors Clinical Case Reports published by John Wiley & Sons Ltd. This is an open access article under the terms of the Creative Commons Attribution License, which permits use, distribution, and reproduction in any medium, provided the original work is properly cited.
Figure 6A, A panoramic ultrasound view showing the extensive thrombus from the base of the penis to the corona. B, Sonographic image of the penis showing the thrombus, corpora cavernosum, and the spongiosum. Reproduced from: [25] Mukendi A M, Mahlobo F. Penile Mondor’s disease: Clinical and sonographic images. Clinical Case Reports. 2019 Nov; 7(11): 2283-2284. https://doi. org/10.1002/ccr3.2469. https://onlinelibrary.wiley.com/doi/ full/10.1002/ccr3.2469 Accessed 2020 Feb 05. Under copyright © 2019 The Authors Clinical Case Reports published by John Wiley & Sons Ltd. This is an open access article under the terms of the Creative Commons Attribution License, which permits use, distribution, and reproduction in any medium, provided the original work is properly cited. Hamilton et al. [4] reported a 36-year-old man who had manifested with lumps in his penis and he described two firm, raised areas upon the dorsum of his penis that had been present for one week. He did not have any penile pain at rest or upon palpation, but he did have discomfort in his penis upon erection. He was asymptomatic otherwise and he denied any trauma. His clinical examination did reveal 2 palpable, firm cords wrapping around the dorsum of his penis just proximal to his glans penis. The affected area of the penis was not tender and did not have any swelling, erythema, or warmth. The skin was intact without any evidence of lesions or signs of trauma. The rest of his clinical examination was normal. He had ultrasound scan of his penis which showed 2 short areas of non-compressibility which was adjudged to be consistent with the diagnosis of superficial penile vein thrombosis. He was treated with non-steroidal anti-inflammatory medicament with warm compresses. When he was called 2 days after his presentation, he did respond that his symptoms had almost completely resolved. Nawaz et al. [26] reported 3 cases of thrombosis of the dorsal vein of the penis as follows:
Figure 6A: A panoramic ultrasound view showing the extensive thrombus from the base of the penis to the corona. Figure 6B: Sonographic image of the penis showing the thrombus, corpora cavernosum, and the spongiosum.
Case 1
A 22-year-old man had presented with red swollen and painful penis of 4 days duration pursuant to vigorous intercourse. His clinical examination did reveal that his superficial dorsal vein of penis was linear, cord-like, as well as painful. He had Doppler ultrasound scan of his penis which showed obstruction of his superficial dorsal vein of penis. The results of his routine haematology and biochemistry blood tests were within normal range. He was treated by means of Ibuprofen 400 mg three times per day for four weeks. There was resolution of the thrombus as well as restoration of the penile dorsal vein blood flow that occurred normally.
Case 2
A 16-year-old male did manifest with pain within his penis as well as swelling of his penis pursuant to masturbation over the preceding 18 hours. He also presented with fever and shivering. His clinical examination demonstrated redness of the dorsal surface of his penis which was painful. A cord-like superficial dorsal vein of his penis was palpated which was painful. He had Doppler ultrasound scan of his penis which demonstrated no evidence of flow within the dorsal vein of his penis. His full blood count result did indicate a total leucocyte count of 13000/cu mm. The results of his routine blood biochemistry tests were within normal range. He received a one-week treatment of Ibuprofen 400 mg orally three times per day and Amoxycillin 500 mg three times daily. His fever subsided but his penile swelling and tenderness persisted. The thrombus from the dorsal vein of his penis was removed under General anaesthesia which demonstrated the obstructed dorsal vein of penis. He was discharged home on the same day and his post-operative recovery was normal.
Case 3
An 18-year-old male had developed a sudden painless, cordlike induration upon the dorsal surface of his penis pursuant to undergoing high-ligation of his left varicocele. A cord-like superficial dorsal vein of his penis was palpated which was slightly painful. He had Doppler ultrasound scan of his penis which demonstrated obstruction of the superficial dorsal vein of his penis. The results of his routine haematology and biochemistry blood tests were within normal range. He received Ibuprofen 400 mg orally three times per day and following 4 weeks of commencement of his treatment, there was complete resolution of the thrombus and Colour Doppler ultrasound scan of his penis had demonstrated free flow of blood.
Ozkan et al. [27] investigated the treatment outcomes among patients who had been diagnosed as having Mondor’s disease of the penis in order to evaluate the effect of the disease on erectile function. They reported that a total of 30 patients who had been diagnosed as having Mondor’s disease were enrolled in their study. All of the patients had undergone clinical examination and Doppler ultrasound scan of the penis and they had filled in the International Index of Erectile Function (IIEF-5) questionnaire at regular intervals.Pharmacotherapy was commenced when Mondor’s disease of the penis was diagnosed. After the data had been confirmed to be normally distributed with utilization of Kolmogorov-Smirnov test, the differences between the 3, IIEF-5 scores were evaluated with utilization of repeated measures analyses of variance as well as post-hoc Bonferroni tests. Ozkan et al. [27] summated the results as follows:
1. The ages of the patients had ranged between 25 years and
48 years and the mean age was 34.3 years.
2. Ten patients did have prolonged coital activity, 4 had
recent long-haul flights, 1 patient had sickle cell anaemia, and
2 patients had trauma of the penis which was caused by sexual
intercourse. Nine patients were considered to be idiopathic.
3. The mean IIEF-5 scores at the baseline, and at 1-monthfollow-
up and 2-month follow-ups were 20.87, 20.07, and
20.97 respectively. Even though no significant difference was
ascertained between the baseline and the 2-month follow-up
IIEF-5 scores, significant differences between the baseline and
the 1-month (P = 0.004) and the 1-month and the 2-month
follow-up IIEF-5 scores (p = 0.0001) were detected.
Ozkan et al. [27] made the ensuing conclusions:
1) Mondor’s disease of the penis is an uncommon
complication which could be successfully treated with
utilization of medical treatment and conservative approach.
2) Their series did show that Mondor’s disease of the penis
does not lead to permanent deformation of the penis or erectile
dysfunction.
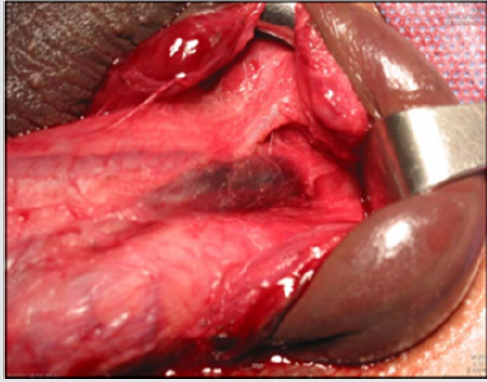
Jung and Ryu [28] reported a 44-year-old man who had manifested with painful swelling of his penis. He did develop spontaneous painful swelling of his penis which was not accompanied by rapid detumescence during masturbation one day preceding his presentation. He did deny a history of acute bending of his penis during masturbation and he did not report the “snappop” sound which is typically associated with fracture of the penis. His clinical examination revealed a markedly swollen ecchymotic and deviated circumcised penis with no evidence of blood at the external urethral meatus see Figure 7. His genitourinary examination as well as the results of his routine haematology and biochemistry blood tests were normal. Despite the non-typical history suggestive of fracture of the penis, a strong suspicion of fracture of the penis was considered as the diagnosis therefore, an operative management was decided upon without undertaking any radiology imaging. During the operation, a sub-coronal circumcision incision was undertaken, and the penis was degloved entirely pursuant to urethral catheterization. No defect was found on either side of the corpus cavernosum and corpus spongiosum. However, upon further dissection, thrombosis of the superficial dorsal vein of the penis was visualised at the proximal part of the penis and this was completely excised and the affected vein was ligated see Figure 8. The sub-coronal incision was repaired with utilization of simple interrupted sutures. The urethral catheter was removed on the first post-operative day and the patient was discharged without any complication. He did achieve satisfactory painless erections without any evidence of curvature of his penis or any erectile dysfunction at his 2-year follow-up. Lessons learnt from this case report include the fact that a differential diagnosis of Mondor’s disease of the penis is fracture of the penis and on rare occasions Mondor’s disease may be misdiagnosed as fracture of the penis. Nevertheless, experience gained from the case report has illustrated that if an acute case of Mondor’s disease of the penis is explored and the thrombosed vein is surgically excised or the thrombus removed this can also lead to good recovery of erectile function as well as it can lead to resolution of the symptoms.
Figure 7: Photograph showed a markedly swollen, ecchymotic, and deviated circumcised penis without blood at the meatus.

Figure 7 Photograph showed a markedly swollen, ecchymotic, and deviated circumcised penis without blood at the meatus. Reproduced from: [28] Jung Y H, Ryu D S. Mondor’s Disease of the Penis Mistaken for Penile Fracture. Urogenit Tract Infect 2016 Apr; 11(1): 39 – 41. http://dx.org/10.14777/uti.2016.11.1.39 https:// synapse.koreamed.org/Synapse/Data/PDFData/1216UTI/ uti-11-39.pdf ] copyright © 2016. The Korean Association of Urogenital Tract Infection and Inflammation All Rights Reserved. This is an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http:// creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Figure 8 Surgical approach reveals superficial thrombophlebitis of the dorsal vein of the penis. Reproduced from: [28] Jung Y H, Ryu D S. Mondor’s Disease of the Penis Mistaken for Penile Fracture. Urogenit Tract Infect 2016 Apr; 11(1): 39 – 41. http:// dx.org/10.14777/uti.2016.11.1.39 https://synapse.koreamed. org/Synapse/Data/PDFData/1216UTI/uti-11-39.pdf] copyright © 2016. The Korean Association of Urogenital Tract Infection and Inflammation All Rights Reserved. This is an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License ( http://creativecommons.org/licenses/ by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Al-Amiri et al. [29] reported 3 patients who were aged 36 years, 44 years, and 28 years, and who had presented with swollen superficial dorsal vein of penis the penis in a sub-acute fashion. All of the 3 patients did have Ultrasound scan of the penis which had shown superficial dorsal vein thrombosis. The three patients were managed conservatively with reassurance and utilization on nonsteroidal anti-inflammatory medications (NSAIDs) on an as may be required basis with instructions to avoid sexual activity during the symptomatic phase of the disease. None of the 3 patients did require to undergo surgical treatment. During the 4-week followup assessment, all the signs and symptoms had subsided without any negative sequelae with regard to 2 patients and 1 patient did have mild residual hardening of his vein which did resolve during his subsequent follow-up assessments. Al-Amiri et al. [29] made the following conclusions:
1. Mondor’s disease of the penis is a benign condition of the
penis.
2. Even though Mondor’s disease of the penis is not common,
Urologists need to be aware of its nature and they should
consider the disease with regard to the differential diagnosis of
the acutely swollen penis.
3. Mondor’s disease of the penis usually tends to be managed
conservatively.
Jakhal et al. [30] reported a 37-year-old man who had manifested with redness and oedema of his penis that had emanated pursuant to sexual intercourse 3 years earlier. The evolution of his disease was marked by persistence of a sclerotic cord upon the dorsal aspect of his penis as well as penile pain. A clinical diagnosis of chronic-stage Mondor’s disease of the penis was made. Stripping of the superficial penile vein was undertaken. Histopathology examination of the specimen did show a focal intimal thickening of the venous wall without obstruction of the vascular light, and an absence of thrombus. A lesson learnt from this case report is that on very rare occasions a case of chromic-stage Mondor’s disease of the penis could be encountered and that surgical treatment would be required which would tend to confirm the diagnosis based upon histopathology examination of the specimen as well as surgical treatment would be an effective treatment for such cases.
Jain et al. [31] reported a 26-year-old single man who had manifested with difficulties in voiding as well as oedema of his penis which was at provisionally diagnosed as well as treated as Mondor’s disease of the penis. He had Doppler ultrasound scan of his penis which demonstrated thrombus within his dorsal vein of penis without any detectable blood flow within the vein, but the scan showed normal blood flow within his dorsal penile artery. He also had ultrasound scan of his lower abdomen which was normal. The results of his routine haematology and biochemistry blood tests were within normal range except for his total leucocyte count that was mildly raised. His symptoms did not improve upon conservative management. He subsequently had a biopsy of the glans of his penis and histopathology examination of the specimen showed features that confirmed the diagnosis of moderately differentiated squamous cell carcinoma (SCC) of the penis. He underwent partial amputation of penis. At his 4-month post-operative follow-up he was well.
A lesson learnt from this case report include:
(a) Squamous cell carcinoma of the penis could mimic
Mondor’s disease clinically as well as upon ultrasound scanning
of the penis therefore clinicians should carefully assess
patients who present with symptoms that are suggestive of
Mondor’s disease of the penis and they should carefully followup
the patients and carefully examine them to confirm if the
provisionally clinically diagnosed Mondor’s disease has settled
completely or not.
(b) With regard to cases of clinically diagnosed Mondor’s
disease of the penis that do not resolve completely, careful
re-examination and biopsy of the residual / persistent penile
lesion would be required in order to confirm a definite diagnosis
so as to enable the most appropriate effective treatment of the
patients.
Conclusion
1. Mondor’s disease of the penis (MDP) is an uncommon
disease of the penis which does mimic more common diseases
of the penis including fracture of the penis, Peyronie’s disease
and sclerosing lymphadenitis of the penis.
2. MDP can be diagnosed through careful history taking and
typical clinical examination features of the disease and when in
doubt the diagnosis can be confirmed through ultrasound scan
examination of the penis including Doppler ultrasound scan.
3. MDP is a self-limiting benign disease and most cases
tend to resolve spontaneously within 4 to 6 weeks following
expectant and conservative management, reassurance of the
patients but many patients would tend to be treated by means
of anti-inflammatory medicaments which help reduce the acute pain but this does not influence the rate of spontaneous
recovery. Topical heparin does help as treatment in the acute
phase of the disease with regard to improvement of symptoms,
but it does not influence the rate of spontaneous resolution of
the disease by. Cases of MDP that persist beyond 6 weeks as
well as chronic MDPs are treated with good results by means of
thrombectomy from the thrombosed dorsal vein of the penis or
resection of the thrombosed superficial dorsal vein of the penis.
4. Patients who have MDP are advised to refrain from coital
activities during the acute painful stage of the disease.
Conflict of Interest
None.
Acknowledgements
Acknowledgements to:
1. The Korean Association of Urogenital Tract Infection
and Inflammation for granting permission to reproduce
figures and contents of their journal article under copyright
This is an open access article distributed under the terms of
the Creative Commons Attribution Non-Commercial License
(http://creativecommons.org/licenses/by-nc/4.0) which
permits unrestricted non-commercial use, distribution, and
reproduction in any medium, provided the original work is
properly cited.
2. Clinical Case Reports. And John Wiley & Sons for granting
permission to reproduce figures and contents of their Journal
article under copyright © 2019 The Authors Clinical Case
Reports published by John Wiley & Sons Ltd. This is an open
access article under the terms of the Creative Commons
Attribution License, which permits use, distribution, and
reproduction in any medium, provided the original work is
properly cited.
3. Case Reports in Urology and Hindawi Journals Ltd for
granting permission for reproduction of figures and contents of
their Journal article under copyright © 2019 Adama Ouattara et
al. This is an open access article distributed under the Creative
Commons Attribution License, which permits unrestricted use,
distribution, and reproduction in any medium, provided the
original work is properly cited.
4. Indian Journal of Urology for granting permission for
reproduction of figures and contents of their journal article
under copyright © Indian Journal of Urology This is an openaccess
article, distributed under the terms of the Creative
Commons Attribution License, which permits unrestricted use,
distribution, and reproduction in any medium provided the
original work is properly cited.
References
- Chaux A, Cubilla AL (2010) Penis and scrotum Inflammatory lesions Mondor Phlebitis.
- https://www.urologynews.uk.com/features/synopsis/post/penile-mondor-s-disease.
- Al-Mwalad M, Loertzer H, Wicht A, Fornara P (2006) Subcutaneous penile vein thrombosis (Penile Mondor’s Disease): pathogenesis, diagnosis, and therapy. Urology 67(3): 586-588.
- Hamilton J, Mossanen M, Strote J (2013) Mondor’s disease the penis. West J Emerg Med14(2): 1-180.
- Nagarsheth KH, Rosh AJ, Rowe VL (2019) Superficial Thrombophlebitis Medscape eMedicine.
- Kumar B, Narang T, Radotra BD, Gupta S (2005) Mondor’s disease of the penis: a forgotten disease. BMJ Journals Sexual Transmitted Infections. 81(6): 480-482.
- Nachmann MM, Jaffe JS, Ginsberg PC, Horrow MM, Harkaway RC (2003) Sickle cell episode manifesting as superficial thrombophlebitis of the penis. Am J Osteopath Assoc 103(2): 102-104.
- Day S, Binghmam JS (2005)Mondor’s disease of the penis following a long-haul flight. Int J STD Aids 16(7): 510-511.
- McLaren AJ, Riazuddin N, Northeast AD(2001) Mondor meets Trendelenberg: penile vein thrombosis after varicose vein surgery. J R Soc Med94(6): 292-293.
- Öztürk H (2014) Penile Mondor’s disease. Basic Clin Androl 3: 24-25.
- Han HY, Chung DJ, Kim KW, Hwang CM,Korean J (2008) Pulsed and color doppler sonographic findings of penile Mondor’s diseaseRadiol9(2): 179-181.
- Swierzewski SJ 3rd DenilJ, Ohl DAThe management of penile Mondor’s phlebitis: superficial dorsal vein thrombosis. J Urol 150(1): 77-78.
- Nazir SS, Khan M(2010) hrombosis of the dorsal vein of the penis (Mondor’s Disease): A case report and review of the literature. Indian Journal of Urology 26(3): 431-433.
- Bird V, Krasnokutsky S, Zhou HS, Jarrahy R, Khan SA(1997) Traumatic thrombophlebitis of the superficial dorsal vein of the penis: an occupational hazard. Am J Emerg Med 15(1): 67-69.
- Rodríguez Faba O, Parra Muntaner L, Gómez Cisneros SC, Martin Benito JL, Escaf Bermadah S (2006) Thrombosis of the dorsal penis vein (of Mondor’s phlebitis). Presentation of a new case. ActasUrolEsp 30(1): 80-82.
- SassoF, GulinoG, Basar M, Carbone A, Torricelli P, et al. (1996) Penile Mondor’s disease: an underestimated pathology. Br JUrol 77(5): 729-732.
- Singla K, Sharma AK, Viswaroop SB, Gopalakrishnan G, Kandasami SV(2012) Mondor’s Disease of the Penis: A Forgotten Entity. URO Today Int J 5(1): art 87.
- Mondor H (1939) Tronculite SonsCutanee de la parvi thoracique antero-lateral. Mem AcadChir65: 1275-1278.
- Braun-Falco O(1955) Clinical manifestations, histology and pathogenesis of the cordlike superficial phlebitis forms. Derm W Schr132(27): 705-715.
- Helm JD Jr, Hodge IG (1958)Thrombophlebitis of a dorsal vein of the penis: report of a case treated by phenylbutazone (Butazolidin). J Urol79(2): 306-307.
- Kraus S, Ludecke G, Weidner W(2000) Mondor’s disease of the penis. Urol Int 64(2): 99-100.
- Yanik B, Conkbayir I, Oner O, Hekimoglu B (2003) Imaging findings in Mondor’s disease. J Clin Ultrasound 31(2): 103-107.
- Ouattara A, Paré AK, Kaboré AF, Yaméogo C, Botcho G, et al. (2019) Subcutaneous Dorsal Penile Vein Thrombosis or Penile Mondor’s Disease: A Case Report and Literature Review. Case Reports in Urology Volume; Article ID 1297048: 3 pages.
- Pittaka M, Fotiou E, Dionysiou M, Polyviou P, Eracleous E, et al. (2017) Penile Mondor’s disease in a patient treated with radical chemoradiation for anal cancer. Oxford Medical Case Reports 2017(8).
- MukendiAM, Mahlobo F(2019) Penile Mondor’s disease: Clinical and sonographic images. Clinical Case Reports 7(11): 2283-2284.
- Nawaz H, Khan S, Ahmed S, Khan M, Pervaiz A, et al.(2003) Mondor’s. Disease of the Penis. Journal of Pakistan Medical Association 53(6).
- Ozkan B, Coskuner ER, TurkA, Akkus E, Yalçin V(2015) Penile Mondor Disease and its Effects on Erectile Function: Results of 30 Patients. Urology Male Sexual Dysfunction 85(1): 113-117.
- JungYH, Ryu DS (2016)Mondor’s Disease of the Penis Mistaken for Penile Fracture. Urogenit Tract Infect 11(1): 39-41.
- Al-Amiri A, Al-Terki A, Al-Shaiji T(2015) Mondor’s Disease of the Penis. Research.
- Jakhal N, Touzani A, Lasri A, Karmouni T, El Khader K, et al. (2017) Penile Mondor’s Disease.Case Report and Literature Review. Global Journal of Reproductive Medicine 2(5): 1-3.
- Jain P, Sarkar D, Pal DK(2018) Penile Carcinoma in Young Age Masquerading as Mondor’s Disease. Journal of Clinical and Diagnostic Research 12(1): 9-10.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...