Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1644
Review ArticleOpen Access
Experience with Sentinel Lymph Node Biopsy in Cervical Cancer Patients in Miguel Servet University Hospital Volume 2 - Issue 4
Yasmina José Gutiérreza*, Laura Baquedano Mainara, Marta Lamarca Ballesteroa, Silvia Ortega Marcillaa, Amparo Borque Ibañeza and Miguel Ángel Ruiz Condea
- A Department of Gynecology, Miguel Servet University Hospital, College of Medicine Zaragoza, Spain
Received: June 06, 2019; Published: June 20, 2019
Corresponding author: Yasmina José Gutiérrez, Department of Gynecology, Miguel Servet University Hospital, College of Medicine Zaragoza, Spain
DOI: 10.32474/OAJRSD.2019.02.000141
Introduction
The current standard of care for women who will be diagnosed with cervical cancer includes radical hysterectomy or trachelectomy and bilateral pelvic lymphadenectomy. For women with earlystage cervical cancer, lymph node status is the most important prognosticator of survival. However, the majority of these patients will not have lymph node metastases. For women with cervical cancer, ideally we would optimize the identification of positive lymph node spread in the minority of patients while limiting the morbidity of lymph node dissection for the majority of women who will ultimately have negative nodes. For that reason, there is significant interest in validating lymphatic mapping and sentinel node biopsy for women with this disease. The sentinel lymph node is the first node that receives drainage from the primary tumor. Therefore, if the sentinel lymph node is negative for metastasis, the remaining lymph nodes in the nodal basin should also be free of tumor. The use of lymphatic mapping and sentinel lymph node biopsy was first described by Cabanas in 1977. In an effort to decrease complications associated with lymphadenectomy, improve detection of micro metastatic disease, and fine tune our lymphadenectomy anatomic templates, sentinel lymph node (SLN) techniques have been developed and extensively studied in many oncologic fields. As a result, SLN technique is now part of the standard treatment guidelines for the management of breast cancer, melanoma, and more recently, it is being recognized as a safe and reasonable approach in select cases of vulvar cancer. The objective of our study is Introduce sentinel lymph node detection in patients with cervical cancer in our center and participle in the validation of the technique in a multicentric way [1].
Material and Methods
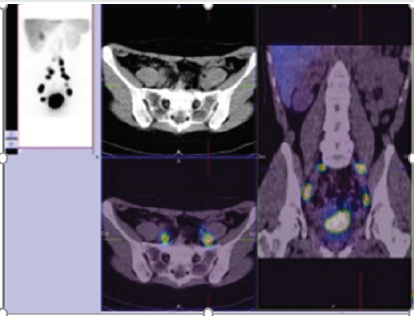
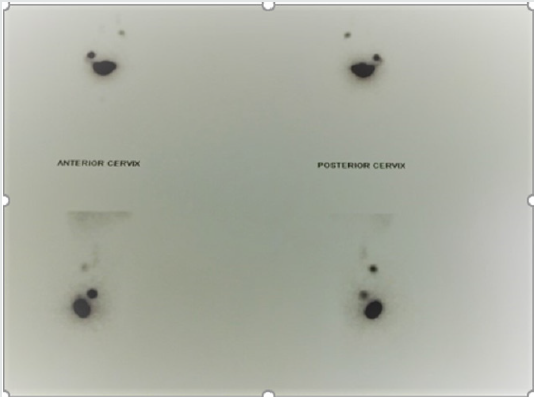
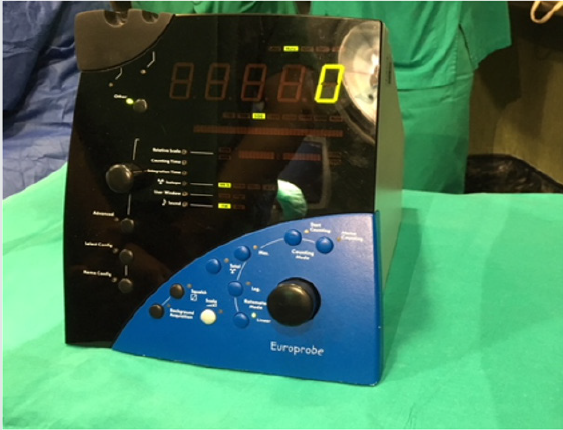
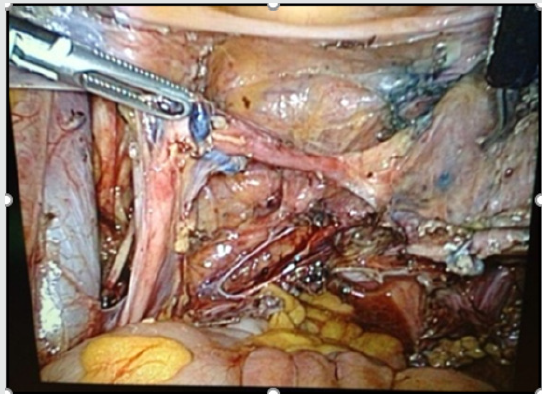
Retrospective descriptive study of the cases of SLN in patients with cervical cancer operated in our center from December 2013 to December 2018. We describe the procedure in our hospital, University Hospital Miguel Sevet from Zaragoza, Spain. Our center is reference center of gynecological oncology of Aragon, Spain. The day before surgery 1mCi/0,5ml nanocoll Technetium 99m was applied into the cervix at 300, 600, 900, and 1200. (Figures 1-2). Blue dye injection (Patentblue) occurred intraoperatively into the cervix at the same locations. We use it only in cases where it is anticipated that the location of the node can be difficult. (Figure 3). Detector gamma probe for laparoscopy is used to perform intraoperative detection of sentynel lymph nodes. (Figures 4-5). All the information about the patients and their datum were transcribed to an information base computerize. We used Statistic Process Social Sciences (SPSS) 20.0 for Windows (Copyright© SPSS Inc., 2006. Licencia Universidad de Zaragoza) to statistical analyses during the study period [2,3].
Results
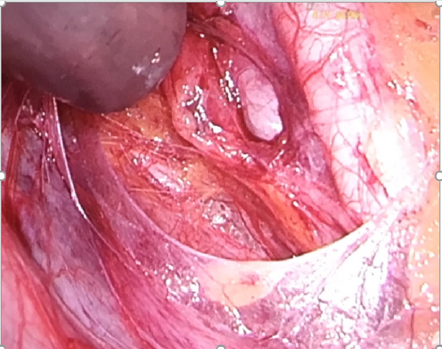
Between December 2013 and December 2018, 19 patients with cervical cancer FIGO stage I, II and II underwent SLN detection during primary operation (radical laparoscopic hysterectomy) or in patients with non-surgical stages to determine the condition of the nodes before radiotherapy. (Figures 6-8) show the process of detection of lymph node during surgery with or without the application of patent blue. In all cases a lymphadenectomy was also performed in the same surgical act because it was an unvalidated technique. The detection rate of SLN was 100%. The false-positive rate was 0 %. After the combined injection, the detection rate, specificity, and positive predictive values were 100%. The sensitivity was 95%. There were only two false negatives discovered. However, in one of these patients the positive node was found in a hemipelvis that did not map. A mean of 2.7 pelvic SLNs were detected. (Figure 9) shows anatomopathological study of sentinel lymph node [4-6].
Figure 9: Anatomopathological study of sentinel lymph node.

Discussion
Multiple single institution studies have reported their experience with sentinel lymph node biopsy in cervical cancer patients. Though the type of tracer used in each of these studies is widely variable, almost all of them describe excellent negative predictive values, ranging from 88% – 100%. However, sensitivity appears to be more inconsistent [7]. The SENTICOL study is the largest multiinstitutional trial of sentinel lymph node biopsy limited to women with early stage cervical cancer. In this study, 139 women with stage IA1 or IB1 cervical cancer underwent intracervical injection with radiocolloid and blue dye followed by sentinel node dissection and pelvic lymphadenectomy. The authors reported a detection rate of 97.8% and a sensitivity of 92%. There were only two false negatives discovered. The study concluded that sentinel node mapping is a sensitive method for detecting lymph node metastasis for women with early-stage cervical cancer. However, opponents have voiced concern that some nodal metastases may be missed if only the sentinel lymph nodes are removed. A high sensitivity of sentinel lymph nodes (SLN) for pelvic lymph node staging has been repeatedly shown in patients with cervical cancer. However, since only SLN are evaluated by pathologic ultra-staging, the risk of small metastases, including small macro metastases and micro metastases, in non-SLN is unknown. This can be a critical limitation for the oncological safety of abandoning a pelvic lymphadenectomy. Mapping sentinel lymph nodes is popular among gynecologistoncologists, which lead to having fewer side effects in patients who suffer from cervical cancer. Thus, more researches are required to confirm the total removal of lymph nodes in patients with sentinel lymph nodes positive. The presence of an effective team (composed of an expert gynecologist- oncologist and nuclear medicine team) is an important factor to have a successful surgery with an acceptable diagnostic power, less invasive operations, and better clinical management [8-10].
Conclusion
Sentinel lymph node detection in patients with cervical cancer is a multidisciplinary procedure involving gynecologists, pathologists and nuclear medicine. Until the validation of the technique, lymphadenectomy will be performed in the same surgical act to all patients in order to obtain data on the reliability of the procedure. According to the previous consensus, the defined validation parameters are at least 95% of the sentinel node identification rate and false-negative rate ≤5%. The validation of the technique will allow to avoid morbidity to patients with early stages and to select patients with affected lymph nodes candidates for radio chemotherapy without the need for radical pelvic surgery.
Acknowledgement
To the department of pathological anatomy of the Miguel Servet University Hospital for collaborating with us.
References
- Cibula D, Oonk MH, AbuRustum NR (2015)Sentinellymphnodebiopsy in themanagementofgynecologiccancer. Curr OpinObstetGynecol27(1):66-72.
- Casper T, Rovers MM, de Graaf C, Zusterzeel PLM, Bekkers RLM (2015)Thesentinelnodeprocedure in earlystage cervical cancer, takingthenext step; a diagnosticreview. Gynecol Oncol139(3):559-567.
- Bats AS, Buénerd A, Querleu D, Leblanc E, Daraï E, Morice P, et al. (2011)Diagnosticvalueofintraoperativeexaminationofsentinellymphnode in early cervical cancer. a prospective, multicenterstudyGynecol Oncol123(2):230-235.
- Darlin L. Darlin L, Persson J, Bossmar T, Lindahl B, Kannist P, et al. (2010)Thesentinelnode concept in early cervical cancerperformswell in tumorssmallerthan 2 cm. Gynecol Oncol117(2):266-269.
- El-Ghobashy AE, Saidi S (2009)A Sentinellymphnodesampling in gynaecologicalcancers: techniques and clinicalapplications.EUR J Surg Oncol: 35(7):675-685.
- Levenback CUpdateonsentinellymphnodebiopsy in gynecologiccancersGynecol Oncol111(2):42-S43.
- Euscher ED, Malpica A, Atkinson EN, Levenback CF, Frumovitz M, et al. (2008) Ultra stagingimprovesdetectionofmetastases in sentinellymphnodesofuterinecervixsquamouscell carcinoma. Am J SurgPathol32(9):1336-1343.
- Bats AS, Buénerd A, Querleu D, Leblanc E, DaraïE, et al (Nov 2011)Diagnosticvalueofintraoperativeexaminationofsentinellymphnode in early cervical cancera prospectivemulticenterstudyGynecol Oncol123(2):230-235.
- Genevieve K, LennoxaAllanCovens (2017) Can sentinellymphnodebiopsyreplacepelviclymphadenectomyforearly cervical cancer? GynecologicOncology 144:16-20.
- Kadkhodayan S, Hasanzadeh M, Treglia G, Azad A., Yousefi Z, et al. (2015)Sentinelnodebiopsyforlymph nodal stagingofuterinecervixcancer: a systematicreview and meta‐analysisofthepertinentliteratureEur. J. Surg Oncol 41:1-20.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...