Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1768
Review ArticleOpen Access
Race, Reality and the Road to Redemption: COVID-19‘s Precipitous Pandemic Problem among Black Lives that Matter Volume 4 - Issue 4
Eric Rogers*
- Profess or Psychology, physics educator, Chicago, Illinois, UK
Received: October 12, 2020; Published: October 23, 2020
Corresponding author:Eric Rogers, Profess or Psychology, physics educator, Chicago, Illinois, UK
DOI: 10.32474/SJPBS.2020.04.000191
Abstract
Race and ethnicity and socioeconomics are high and heinous risky punitive pawns in game of life and health care relative to underlying conditions that impact health. Long-standing systemic health and social inequities open the door and maintain a breeze of devastating consequences putting many people from racial and ethnic minority groups at increased risk of getting sick and dying from COVID-19. The term “racial and ethnic minority groups” includes people of color with a wide variety of backgrounds and experiences. Equally important, But some experiences are common to many people within these groups (heart disease, dementia, alzheimers, diabetes, stroke, etc.). Yet, specific social determining factors wreak havoc on individuals, particularly of color: Social determinants are simply are conditions in the places where people live, learn, work, and play that affect a wide range of health and quality-of life-risks and outcomes.
Introduction
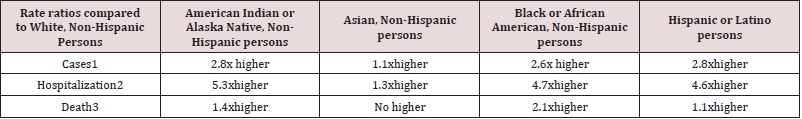
The bottom line is that social determinants of health have
historically prevented them from having fair opportunities for
economic, physical, and emotional health. Furthermore, there is
unequivocal evidence that some racial and ethnic minority groups
are being disproportionately affected by COVID-19. Factors that
contribute to increased risk include but not limited to : Ignorance
and Irresponsiblity: Individuals across the racial divide in America
often believe they are invincible and immune to the virus, etc. They
consciously choose not to wear mask nor keep their respective
distances 6 feet or further. Hygiene is not taken seriously nor
health efforts to minimize the spread and contagiousness of COVID
19. Far too many persons take solace in having house parties,
cookouts, barbecues, backyard fellowships and birthday partiesall
of course with either limited masking, distance or essentially
none at all. Discrimination: Unfortunately, discrimination exists
in systems meant to protect well-being or health. Discriminating
systems include health care, housing, education, criminal justice,
and finance. Make no mistake about it, discrimination in any form
which includes racism, can lead to chronic and toxic stress and
shapes social and economic factors that put some people from
racial and ethnic minority groups at increased risk for COVIDHealthcare
access and utilization: People of color and lower
income backgrounds are more likely to be uninsured than non-
Hispanic whites. An injury and insult is the reality of many other
factors, such as lack of transportation, child care, or ability to take
time off of work; communication and language barriers; cultural
differences between patients and providers; and historical and
current discrimination in healthcare systems. Many people of color
don’t trust the healthcare system and they shouldn’t. Why? Because
life is a cruel teacher: It gives you exam first, then the lesson (Table
1). The historical realities of exploitation, abuse, degradation and
death specifically targeted at people of color are a matte of public
and private records such as the Tuskegee Study of Untreated
Syphilis in the African American Male and sterilization without
people’s permission highlight this reality.
Occupation: People of color are grossly represented in work
settings such as healthcare facilities, farms, factories, grocery stores,
house keeping, cleaning, and public transportation. Some people
who work in these settings have more chances to be exposed to
the virus that causes COVID-19 due to several factors, such as close contact with the public or other workers, not being able to work
from home, and not having paid sick days. Educational, income, and
wealth gaps: Inequities in access to high-quality education for some
racial and ethnic minority groups can lead to lower high school
completion rates and barriers to college entrance. This may limit
future job options and lead to lower paying or less stable jobs [1].
People with limited job options likely have less flexibility to leave
jobs that may put them at a higher risk of exposure to the virus that
causes COVID-19. People in these situations often cannot afford to
miss work, even if they’re sick, because they do not have enough
money saved up for essential items like food and other important
living needs.
Housing: Some people from racial and ethnic minority groups
live in crowded conditions that make it more challenging to
follow prevention strategies. In some cultures, it is common for
family members of many generations to live in one household.
In addition, growing and disproportionate unemployment rates
for some racial and ethnic minority groups during the COVID-19
pandemic may lead to greater risk of eviction and homelessness
or sharing of housing. These factors and others are all associated
with more COVID-19 cases, hospitalizations, and deaths in areas
where racial and ethnic minority groups live, learn, work, play,
and worship. They have also contributed to higher rates of specific
medical illnesses and conditions that increase one’s risk of severe
illness from COVID-19. In addition, community strategies to slow
the spread of COVID-19 may cause unintentional harm, such as lost
wages, reduced access to services, and increased stress, for some
racial and ethnic minority groups [2-4].
s
Furthermore, neuro-cognitive implications are meticulously
decisive in their impact and impetus effects: Whether it is mental
fatigue and mild loss of concentration major neuro health issues
are frequently reported by people with COVID-19. More severe
cognitive impairment is reported in those with secondary illness
such as stroke, which has been reported even in younger COVID
patients and is believed to result from coagulopathy caused by
SARS-CoV-2. Encephalopathy is observed after extubating, possibly
due to lingering effects of sedation and possibly due to the effects
of mechanical ventilation. This often resolves over a period of days
but can sometimes persist for weeks or even months.
Conclusion
Encephalopathy can be further exacerbated by bacterial infection, which can develop during ventilation. So far there are relatively few reports of meningitis/encephalitis associated with SARS-CoV-2, although it is possible more reports of direct infection will emerge over time, similar to previous coronavirus outbreaks (e.g., the SARS-CoV-1 outbreak in 2003 and the Middle East Respiratory Syndrome outbreak in 2012) And the most recent medical and scientific reports showed that the most severe cases of COVID-19 were the most likely to develop neurological symptoms [4-8]. Risk factors for neurocognitive symptoms in those cases are similar to other populations with acute respiratory distress syndrome. Those risk factors include pre-existing diagnoses such as dementia, subarachnoid hemorrhage, and epilepsy. Increased risk of neurocognitive effects is also associated with pathophysiological events during acute care, such as hypoxemia, hypoperfusion and inflammatory response. Finally, further increase in risk is observed when management during acute care includes sedation, mechanical ventilation, and complications such as delirium. Consequently, we have been warned. Wear your mask. Wash your hands. Wedge the distance (whether its 6 feet or 6 steps)…because this virus…this vicious and vile venom of bio-chemical expression is coming soon to a place….a person and/or a predicament near you.
References
- Institute of Medicine (US) Committee on the Consequences of Uninsurance. Care Without Coverage: Too Little, Too Late. Washington (DC): National Academies Press (US).
- Institute of Medicine (2003) Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: The National Academies Press, USA.
- (2003) US National Library of Medicine. Native Voices: Timeline: Government admits forced sterilization of Indian Women.
- Novak NL, Lira N, O’Connor KE, Harlow SD, Kardia SLR, et al. (2018) Disproportionate Sterilization of Latinos Under California’s Eugenic Sterilization Program, 1920-1945. Am J Public Health 108(5): 611-613.
- Stern AM (2005) Sterilized in the name of public health: race, immigration, and reproductive control in modern California. Am J Public Health 95(7): 1128-1138.
- Prather C, Fuller TR, Jeffries WL (2018) Racism, African American Women, and Their Sexual and Reproductive Health: A Review of Historical and Contemporary Evidence and Implications for Health Equity. Health Equity 2(1): 249-259.
- US Bureau of Labor Statistics. Labor force characteristics by race and ethnicity.
- Economic Policy Institute. Black workers face two of the most lethal preexisting conditions for coronavirus-racism and economic inequality.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...