Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1768
Research ArticleOpen Access
Expectations and Attitudes of Relatives and Parents of Children with Severe Central Nervous System Defect Volume 6 - Issue 5
Jerzy A Skuciński1, Kacper Grudzień1, Zuzanna Baliga1, Kamil Hapkiewicz1, Wojciech Grabowski1, Karolina Kwiatkowska2, Stanisław Kwiatkowski2 and Olga Milczarek2*
- 1Students’ Scientific Group at the Department of Pediatric Neurosurgery, Jagiellonian University Medical College, Poland
- 2Department of Children’s Neurosurgery, Jagiellonian University Medical College, Faculty of Medicine, Institute of Pediatrics, Poland
Received:October 18, 2022; Published:November 02, 2022
Corresponding author: Olga Milczarek, Department of Children’s Neurosurgery, Jagiellonian University Medical College, Faculty of Medicine, Institute of Pediatrics, Poland
DOI: 10.32474/SJPBS.2022.06.000248
Abstract
The advancement of medicine enables the maintenance of vital functions in patients born with lethal Central Nervous System (CNS) malformations. Patients can live long life with appropriate care and specialized pediatric treatment even with presumably very low quality of their and their relatives’ life. In this study we explore the realities of palliative care and quality of life of children with severe CNS malformations, focusing on extreme hydrocephalus, resulting in nervous tissue compression, which leads to irreversible brain damage and atrophy. The retrospective study was carried out on 13 children hospitalized in the Department of Pediatric Neurosurgery due to extreme congenital hydrocephalus between 1996 and 2017. Based on medical histories, we analyzed treatment strategies and outcomes. We decided to carry out a follow-up study based on a questionnaire interview with the parents and examination of the children. The questionnaire was focused on analyzing children’s disabilities, daily functioning, family dynamics as a result of the disease, socioeconomic problems and social perception of the child and family. The quality of life was analyzed with Pediatric Quality of Life Inventory (PedsQL) 4.0. Generic Core Scales.
CNS malformations result in extreme changes in their families’ daily life and routines. Patients require 24/7 palliative care and, sometimes, artificial life support and multiple medical interventions. Therefore, early prenatal detection which enables the parents to undergo psychological and medical counselling should be followed by a knowledgeable decision regarding keeping the pregnancy or its termination. When it comes to results of quality of life, its analysis reveals objectively surprisingly high scores for this type of severity which may be caused by parents’ lowered expectation towards their children’s performance related with naturally positive feeling of having offspring.
Keywords: Wodogłowie; Bezmózgowie; Jakość życia; Hydrocephalus; Anencephaly; Quality of life
Introduction
The definition of a congenital disorder is very broad and encompasses every anatomical abnormality present at birth. Congenital disorders are present in approximately 2-3% of neonates alive at birth, in up to 10% of those stillborn, while up to 50% of fetuses with severe malformations die in utero in the early weeks of pregnancy. The currently available literature lacks reliable data on the fates of children born with CNS malformations considered lethal. These patients are usually cared for by multiple physicians and healthcare providers, yet few of them focus on the qualities of lives of these affected by the disease [1]. CNS malformations often lead to a spectrum of neurological disorders, which have a significant impact on the quality of lives of these patients and their relatives.
The necessity of repeatedly performing surgical procedures, regular hospital admissions, rehabilitation and palliative care are only just a few of the problems the patients and their families face [2] (Attachment 1).
Aim of the Trial
This study was carried out with the intention of gauging the quality of lives and the outlooks of relatives and parents of children who have been neuro surgically treated because of the aforementioned pathologies.
Materials and Methods
Characteristics of the studied demographics
13 patients with severe hydrocephalus were qualified (7 girls and 6 boys). In all patients the diagnosis of severe hydrocephalus or anencephaly was made. The main differences pertained to the etiology of the main disorder, its severity and other accompanying malformations. In the examined population, hydrocephalus was recognized in 9 patients, including the following subtypes: idiopathic (1 boy), post-hemorrhagic (1 boy, 1 girl), with accompanying dysraphism (1 boy, 4 girls) and in a patient with Dandy-Walker syndrome (1 girl). One female patient was diagnosed with holoprosencephaly. Anencephaly was recognized in 3 boys. Dysraphism was recognized in 6 patients; in 5 cases multiple malformations coexisted (3 malformations in 3 girls and 1 boy, 2 malformations in 1 girl). In 1 boy the malformation was isolated. Neurogenic bladder as an isolated disorder secondary to dysraphism was diagnosed in 3 girls. In 3 cases cerebral midline malformations were found, specifically septum pellucidum agenesis (1 girl, 1 boy), partial corpus callosum agenesis (1 girl) and colpocephaly (1 girl, 1 boy). Epilepsy was diagnosed in 5 children (3 girls, 2 boys), including 1 West syndrome diagnosis in a boy. Lower extremity paresis was found in 3 patients (2 girls, 1 boy) and spastic tetraparesis in 1 boy.
Applied surgical treatment
The hydrocephalus found in 10 patients required surgical treatment. The treatment modality most frequently used were ventriculoperitoneal shunt implantation, Rickham reservoir implantation and third ventriculostomy (in 1 boy, as a causal treatment of hydrocephalus). 1 female patient experienced shunt system infection, which resulted in the girl’s death.
Quality of Life assessment
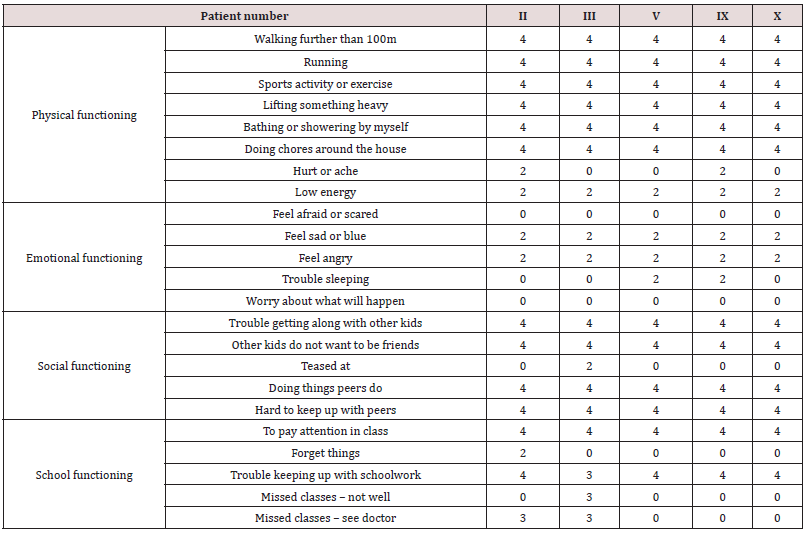
To assess the quality of life, the Pediatric Quality of Life Inventory (PedsQL) 4.0 Generic Core Scales was filled in by the parents of the affected children. The form was intended to gather the parents’ views on their children’s functioning in the physical, emotional, and social spheres, as well as in professional, school, or university settings (Table 1).
Results
The quality of life assessment was performed in 11 patients out of 13 qualified for the study. 1 of the patients had died, and for one of them an incomplete form was delivered. Physical functioning assessment in patients aged 2-4 allows to draw conclusion that their functioning deviated significantly from their peers. Additionally, the discomfort associated with pain and fatigue makes it difficult for the patients to function on every day leaving. Furthermore, the patients experience emotional problems. They do not display emotion with the same aptitude their peers do, and they have difficulty sleeping. The patients’ relationships with other children are abnormal, which is most likely the result of not being able to “keep up” with the pace at which fully healthy children play. The patients are impaired in their ability to establish new interpersonal relations, which can be attributed to the fact, that they do not attend nurseries or kindergartens. Their peers, however, do show interest in playing with them (Table 2).
Quality of life assessment in patients aged 5-7 points towards similar difficulties in functioning as in the previous group. The examined population does not experience the same spectrum of emotions as their peers, they do, however, show some improvement over the previous demographics. Similarly to the previous group, they also experience difficulty sleeping and keeping up with the pace at which their peers play, the reasons for which do not differ significantly from the previous paragraph. Focusing is troublesome for the examined children, yet their parents do not report any major problems with their performance in kindergartens or schools. The patients occasionally do not show up to some of their classes due to feeling unwell or hospitalizations (Table 3).
The degree of disability among examined children aged 8-12 is similar to that of the previous groups. These patients experience emotion to a bigger extent compared to the other demographics. Difficulty sleeping is also prevalent in this age group, yet to a lesser degree. Most of these children attend school, but just as their younger counterparts, have trouble establishing social contacts, maintaining close interpersonal relationships and fulfilling tasks in the same time as their peers (Table 4).
Despite living with a disability, the studied children are not shunned by their peers, nor are they subject to hostile interactions from them, which remarkably improves the patients’ quality of lives and sheds new light on the social implications of disability and its acceptance.
Discussion
According to the World Health Organization, quality of life is a person’s subjective assessment of their life situation, judged against the culture they live in, their value system, goals, expectations, personal interests [3]. Hydrocephalus in children treated with shunts affects their physical, socio-emotional and cognitive qualities of life [4]. A study, carried out by Eloqayli, et al. using the PedsQL 4.0 questionnaire, evidenced better physical functionality in children with hydrocephalus treated with a programmable shunt, which suggests their better quality of lives. What’s interesting, the authors noted a decrease in the children’s social abilities between the ages of 2 and 3, which was probably brought about by the parents’ overprotectiveness. In our study, the patients are also affected by other disorders, apart from hydrocephalus, which also significantly lower their quality of lives and their ability to thrive in different areas: physical, emotional and social. The development of these aspects is markedly delayed when compared with those of their peers. It’s noteworthy, that the patients in our study, also utilizing the PedsQL 4.0 form, also showed impairment in the emotional sphere; some of them weren’t able to experience fear, and almost none of them expressed concern about their futures.
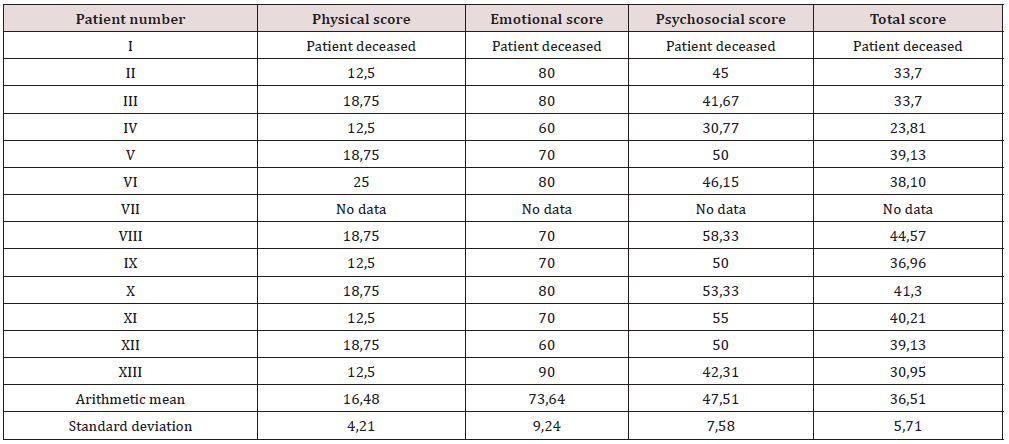
While examining the quality of lives in children with post-hemorrhagic hydrocephalus treated with programmable shunts, Gigi et al. evidenced a significant dip in Health-Related Quality of Life (HRQoL), measured with PedsQL form, in every aspect when compared with the control group. These results were driven by conditions adversely affecting the children’s development, i.e. nonprogressive encephalopathy, epilepsy, intellectual disability [3]. These results differ from these collected by our research team. Motor skills are shown to be significantly lower in our study (16.48 [SD 4.21] vs. 36 [SD 34.9]), and emotional functioning - to be better (73.63 [SD 9.24] vs. 59.8 [SD 26.7]) (Table 5). It’s worth mentioning, that the examined group encompasses a much wider scope of hydrocephalus patients, which also impacts their motor skills, including achieving respective developmental milestones. Thus, one can draw the conclusion that the coexistence of other congenital CNS malformations essentially impairs the quality of life, mainly in physical functioning, more so than hydrocephalus alone.
In a similar study performed by Sumpter, et al. which also utilized the PedsQL questionnaire, also pointed to the finding that the older a child with hydrocephalus, the lower their quality of life. The authors note that motor skills among affected teenagers are lower than in children with the same condition. Noticeably lower results were also achieved in the social sphere. This piece of research also emphasizes the need to consider the psychosocial needs of children and teenagers with hydrocephalus as a cornerstone of holistic treatment plan for these patients. The potential benefits of this approach may improve their academic achievements, decrease the occurrence of mental health problems throughout their whole lives and ease the stress of their caretaker and the rest of their immediate surroundings [5]. Our study did not enroll teenagers over the age of 12, therefore we did not have the opportunity to make comparisons involving older age groups. What we did capture was the noticeable difference in the psychosocial sphere between children aged 4-7 and 8-12 (54.44 vs. 48). It is plausible that this finding is reflective of possible future downward trend. According to the latest literature review, the quality of life assessment form utilized by us-the PedsQL-is one of the most oft-used questionnaires as a research tool. It can be adapted as an instrument to measure the quality of lives in children with hydrocephalus treated with a programmable shunt [6]. Our study has its limitations: the researched population is quite small when juxtaposed with the cited articles and the lack of patients aged 13-18 also affects the presented results.
Conclusion
The high ratings of different aspects of quality of lives act encouragingly to wager a discussion on the attitudes and expectations of parents regarding the levels at which their children should function. It is important to keep in mind, though, that the widely applied tools used to gauge the quality of life are highly subjective, and in the case of our patients carrying out a reliable analysis of their quality of lives is nigh impossible, as it is deviated by their parents’ low expectations as to their functioning. These low expectations are most likely resultant of the parents’ naturally occurring positively charged emotions towards their progeny. The lives of families of these patients require making many sacrifices and devoting more time and attention to their children, compared with taking care of fully healthy children. As such, we deem it vital to have access to appropriate perinatal testing and psychosocial assistance serves for the parents and their families starting in the pregnancy period, should the parents decide or are made to uphold the pregnancy.
References
- Glinianaia SV, Embleton ND, Rankin J (2012) A systematic review of studies of quality of life in children and adults with selected congenital anomalies. Birth Defects Res A Clin Mol Teratol 94(7): 511-520.
- Rocque BG, Bishop ER, Scogin MA, Hopson BD, Arynchyna AA, et al. (2015) Assessing health-related quality of life in children with spina bifida. Journal of Neurosurgery: Pediatrics 15(2): 144-149.
- WHO (1997) WHOQOL: Measuring Quality of Life. Division of mental health and prevention of substance abuse.
- Gigi M, Roth J, Eshel R, Constantini S, Bassan H (2019) Health‐related quality of life after post‐haemorrhagic hydrocephalus in children born preterm. Developmental Medicine & Child Neurology 61(3): 343-349.
- Sumpter R, Dorris L, Brannan G, Carachi R (2012) Quality of life and behavioural adjustment in childhood hydrocephalus. Scottish medical journal 57(1): 18-25.
- Lusiana D (2020) Evaluate on the quality of life of hydrocephalus children with shunt implants: literature review. IJDS: Indonesian Journal of Disability Studies 7(1): 124-129.
Attachment 1. Pediatric Quality of Life Inventory (PedsQL) 4.0. Generic Core
In order to assess the quality of life, the Pediatric Quality of Life Inventory (PedsQL) 4.0. Generic Core Scales form for parents was utilized. The parents of the examined children were asked questions regarding things which may be troublesome to their offspring. Taking into account all the events that had happened in the previous month, the parents were asked to describe how difficult it was for their child to perform each of the activities included in this form by assigning the appropriate number of points according to the following rules:
a) 0 if they never have difficulty doing it
b) 1 if they almost never have difficulty doing it
c) 2 if they sometimes have difficulty doing it
d) 3 if they often have difficulty doing it
e) 4 if they almost always have difficulty doing it
The activities in question were grouped into following categories: physical functioning, emotional functioning, social functioning, nursery/kindergarten/school functioning.
Physical functioning
a) Walking/walking further than 100m (depending on the age)
b) Running
c) Participating in active games, sports/exercise or exercise (depending on the age)
d) Lifting something heavy
e) Bathing/bathing or showering by himself (depending on the age)
f) Helping pick up the toys after playing/helping around the house, e.g. picking up the toys/doing chores around the house (depending on the age)
g) Feeling hurt or ache
h) Feeling low on energy
1. Emotional functioning
a) Feeling afraid or scared
b) Feeling sad or blue
c) Feeling angry
d) Trouble sleeping
e) Worrying/worrying about what will happen (depending on the age)
2. Social functioning
a) Trouble getting along with other kids
b) Other kids do want to be friends
c) Being teased at
d) Inability to do things peers do
e) Difficulty keeping up with other kids
3. Nursery/Kindergarten/School functioning
a) Paying attention in class (optional, depending on the age)
b) Forgetting things (optional, depending on the age)
c) Trouble keeping up with what peers do/schoolwork (depending on the age)
d) Missing classes due to feeling unwell
e) Missing classes due to an appointment with a doctor/hospitalization
The results are transformed into a scale of 0-100 in the following way: 0=100, 1=75, 2=50, 3=25, 4=0. The results can be divided into Physical score, Emotional score, Psychosocial score, and Total score. Physical score is an arithmetic mean of the transformed scores received in the questions regarding physical functioning. Emotional score is an arithmetic mean of the transformed scores received in the questions regarding emotional functioning. Psychocial score is an arithmetic mean of the transformed scores received in the questions regarding emotional, social, and school functioning. Total score is an arithmetic mean of all transformed scores assigned to all the categories.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...