Lupine Publishers Group
Lupine Publishers
Research Article(ISSN: 2637-4722) 
Systematic Developmental Interventions for Preterm Infants in the Neonatal Intensive Care Unit: An Occupational Therapy Perspective Volume 1 - Issue 5
Kendra Schnack¹, Katelynn Martin¹, Makenna Brown¹, Courtney Cahow¹, Shirley Blanchard*¹ and Lisa Bader²
- 1Department of Occupational Therapy, Nebraska
- 2Bergan Mercy Medical Center, Omaha, Nebraska
Received: November 01, 2018; Published: November 09, 2018
Corresponding author: Shirley Blanchard, Department of Occupational Therapy, Nebraska
DOI: 10.32474/PAPN.2018.01.000125
Abstract
Background: There is paucity of evidence supporting occupational therapy interventions and outcomes for premature infants in the neonatal intensive care unit (NICU). This study sought to determine the relationship between the type and frequency of occupational therapy interventions delivered in systematic developmental order with neuromotor and developmental outcomes for preterm infants and to examine the frequency of occupational therapy interventions in relation to an infant’s activity tolerance at baseline.
Methods: Thirty-nine infants born between 23 weeks and 28 weeks, six days gestation were included in a retrospective chart review using a data collection form developed by the authors. The data collection form was used to analyze type and frequency of systematic sensory-based interventions performed, level of initial activity tolerance, total visits to discharge and Test of Infant Motor Performance Version 5.1 (TIMP) scores prior to discharge to determine if there is a correlation.
Results: Results support a systematic delivery of interventions that follow the development of an infant’s sensory system. Analysis indicated that 53.8% of infants achieved scores in the average TIMP category prior to discharge from the NICU. The frequency of occupational therapy interventions increased with lower levels of activity tolerance at baseline.
Conclusion: This study demonstrated the vitality of occupational therapy’s presence in the NICU for delivery of developmentally appropriate services in accordance with activity tolerance and sensory system development. Further research is warranted to increase consistency in interventions and documentation among neonatal therapists to ensure quality and systems appropriate delivery.
Keywords: Neonatal Intensive Care Units; Occupational Therapy; Preterm Infants; Early Intervention
Abbrevations: NICU: Neonatal Intensive Care Unit; TIMP: Test of Infant Motor Performance; AAP: American Academy of Pediatrics; SDT: Synactive Development; CNS: Central Nervous System; HIPAA: Health Insurance Portability and Accountability Act; SPSS: Statistical Package for the Social Sciences
Introduction
Preterm birth is prevalent worldwide and impacts an estimated 9.6% of infants [1]. Preterm birth can be categorized into three subcategories: “extremely preterm (<28 weeks’ gestation), very preterm (28 to <32 weeks’ gestation), and moderate to late preterm (32 to <37 weeks’ gestation)” [1]. Infants born prematurely are at risk for developmental delays, compromised neurodevelopment, and health conditions such as cerebral palsy [2]. Problems associated with neurodevelopment often lead to intellectual disabilities, and visual and hearing impairments [3]. Occupational therapists provide early intervention based on the infant’s sensory system development and focus on prevention of abnormal sensory and motor responses that promote appropriate neurodevelopment. The American Academy of Pediatrics (AAP) now requires that a neonatal occupational or physical therapist be on staff for both Level III and IV neonatal intensive care units (NICU) [4]. According to the American Academy of Pediatrics, Level III NICUs are equipped to care for infants “<32 weeks’ gestation, weigh <1500 g at birth, or have medical or surgical conditions, regardless of gestational age” [5].
Similarly, Level IV NICUs are equipped to care for infants with the same level of medical complexity and may also perform specialized surgeries for these infants [5]. Because infants in the NICU present with complex medical and rehabilitative needs, therapists must possess advanced skills needed to optimize the development and outcomes for each infant [6]. It has been shown that infants do not receive enough early rehabilitative services while in the NICU [7]. Neurodevelopmental interventions are graded, bridge motor and cognitive development, and follow a developmental protocol that aids in reducing sequelae of preterm infants [1]. The synactive development (SDT) model may be used to observe preterm infant behavior, response to the environment, manage neurodevelopmental disorders and develop intervention plans [8]. The model infers that infant development is a hierarchal process consisting of five subsystems (1) neuro vegetative, (2) motor system, (3) behavioral system, (4) attention to interaction, and (5) self-regulation.
The function and stability of each system depends on the maturation of the next system. Infants reach behavioral goals through self-regulation and the interaction of the five subsystems. Occupational therapists must consider sensory/perceptual system development when providing interventions to premature infants due to the close link to neurodevelopment [7,9]. If sensory systems are stimulated prior to maturation, problems can arise with neuromotor and developmental outcomes [6]. Similar to the SDT model, the sensory/perceptual system develops in the following sequence: somatosensory (tactile and proprioceptive), vestibular, chemoreceptive (taste and smell), auditory, and visual [6]. Tactile stimulation is defined as “gentle, light, and systematic skin-to skin therapy that is cephalocaudal in nature” (p.85) [7].
Tactile interventions facilitate appropriate neurodevelopment and include containment holds, static proprioceptive input to the body, static/dynamic proprioceptive input to each extremity, passive range of motion, positive touch, static touch, deep pressure points, tactile desensitization, infant massage, colic massage, edema massage, and myofascial release based on each infant’s developmental status and needs [10]. Vestibular interventions are used for central nervous system (CNS) development such as gentle rocking, linear vestibular input (infant swings or vibrating infant seats) or graded multimodal inputs [11]. Oral motor treatment for preterm infants is important for the safe and efficient coordination of sucking, swallowing, and breathing [12]. Auditory interventions include music therapy or exposure to voice, music, and meaningful sounds which fine tune auditory development; this is also an important factor for supporting auditory/language recognition and development [13].
Mobiles hung over the crib serve as a visual intervention and stimulation for the visual system which is the last to mature [11]. Unimodal stimulation is the best for many preterm infants; however, as an infant’s sensory/perceptual system develops, the CNS is mature enough to tolerate multimodal stimulation or several sensory and motor treatment combinations [10]. Recent studies using multimodal stimulation have shown promise in high risk infants [14]. Poor tolerance is identified if the infant is physiologically unstable and exhibits finger splaying, change in color, arching, crying, hiccupping, or looking away [10]. The order of multimodal facilitation includes containment holds, static proprioceptive input, positive touch, proprioceptive input to each extremity, myofascial release, infant massage, gentle rocking, tummy time, therapeutic ball activities, feeding, soft music and human voice, toys with gentle sounds, utilizing the human face as the best toy, and mobile in crib for visual input [10].
Currently there are no standardized assessments for infants less than 34 weeks gestation due in part to the preterm infant’s inability to tolerate extensive sensory and motor contact. While an occupational therapist may attempt to assess other areas such as reflexes, tone, and quality of movement, the infant may not be able to tolerate these inputs. Thus, it is important to document observations of baseline activity tolerance to guide future therapy sessions. Previous research has not addressed the hierarchical order of occupational therapy interventions based on sensory system development of preterm infants’ neuromotor and developmental outcomes. This study sought to (1) describe the distribution of occupational therapy interventions delivered in the NICU based on sensory system development, (2) to evaluate the relationship between preterm infant neuromotor and developmental outcomes with type and frequency of OT sensory-based interventions, and (3) to examine the relationship between the frequency of occupational therapy interventions received and activity tolerance at baseline.
Methods
Participants
A convenience sample of de-identified medical charts from a Midwestern Level III NICU were utilized for data abstraction. The lead therapist selected 39 preterm infant charts that were extremely preterm or born between 23-28 weeks, six days gestation. Extremely premature infants who had serious medical conditions such as intraventricular hemorrhage grade III or IV, periventricular leukomalacia, trauma at delivery, or any serious genetic or neurological condition were excluded from the sample because of possible compromised sensory system development and significant comorbidities impacting the infant’s neurodevelopment. At this Level III NICU, infants with neurological conditions were typically seen 5-7x/week due to the advanced medical complexity whereas infants with a primary prematurity diagnosis were seen 3-5x/week. Infants who were born before 23 weeks gestation were excluded from the sample because few infants survive who are born prior to 23 weeks and rehabilitation services are typically not appropriate due to failure to thrive.
Infants born after 28 weeks and six days gestation were excluded from the sample because these infants would no longer be classified as extremely premature. Research suggests that extremely premature infants remain at high risk for death and disability with 30–50% mortality and at least 20–50% risk of morbidity for survivors [15]. The chances of survival between extreme premature infants when compared to other classified premature infants is much less due to length of gestation [16]. Information collected in this study was not disclosed to the study participants as participants did not take an active role.
Measures Instrument
A self-developed data collection form (Appendix A) was organized based on a review of literature related to preterm infant development. The form consisted of demographics, gender, Apgar scores, maternal and delivery complications, infant sensory and motor assessment in the NICU (such as movement, tone, and reflexes), activity tolerance, and parental presence during intervention. Type of sensory processing, type of intervention, and number of facilitations was obtained. The data collection form was pilot tested by the lead NICU occupational therapist on three infant charts. These charts were not included in the final data set to avoid biasing the data. Results of the pilot study were used to make final modifications to the data collection form. Additional information gathered included demographics, duration of total therapy minutes, frequency of total therapy visits, total number of specific occupational therapy interventions, and TIMP score and category at discharge.
To measure the infant’s neurodevelopmental status, the Test of Infant Motor Performance Version 5.1 (TIMP) was administered prior to discharge to determine the need for future services and/or recommendations for parents and caregivers. The TIMP assesses motor developmental delay from 34 weeks postconceptional age through four months post-term based on age standards developed from a sample of 990 U.S. infants (all races/ethnicities) [17]. Psychometrics indicate that test-retest reliability for 116 pairs of tests was r = .89 over three days. There was no significant difference between testers and significant predictability in motor function in years to come on related neuromotor tests [17,18]. Currently, no psychometrics exist using the TIMP for retrospective assessment and correlation with occupational therapy interventions. The infant’s TIMP percentile rank was based on the raw score and corrected gestational age. TIMP scores were categorized into far below average, below average, low average, and average categories [19].
Average is the highest category an infant can receive on the TIMP. Practitioner rated activity tolerance as good, fair, or poor based on the infant’s response throughout the initial evaluation. Adverse reactions which led to a fair or poor activity tolerance included: oxygen desaturation, significant changes in heart rate or blood pressure, and/or signs of physical distress which included stiff or tense body or limbs, finger splaying, limp posture, protection of infant’s own face with hands/arms, sticking their tongue out, or grimacing [16]. Additional behaviors that can indicate stress include color changes, level of arousal, agitated or frantic movements, hyperextension, gagging, spitting up, arching, and gaze aversion [20]. Activity tolerance is a sign of CNS development, if the infant is tolerating more inputs, the CNS is developing appropriately and will exhibit more stable vital signs, thermoregulation sucking, cuddling, trunk movement, and deep quiet sleep as the infant is progressing to self-regulation [8].
Procedure
To gain access and for continuity of chart review, all members of the research team completed a required on-boarding process including hospital electronic medical record orientation and a review of the Level III NICU with the lead occupational therapist. Charts meeting inclusion criteria were pre-selected and numbered for de-identification in order to protect privacy and maintain Health Insurance Portability and Accountability Act of 1996 (HIPAA) requirements. Medical charts were assigned to each of four researchers. This study was approved by the Institutional Review Board prior to data collection.
Study Design
This study used a self-developed data collection form for data abstraction. Quantitative methods using descriptive statistics were used to obtain frequency counts. Information was collected and transcribed onto the data collection form. The researchers peer reviewed each other’s chart reviews; missing and inconsistent data was discussed with the lead NICU occupational therapist. Member checking was used to resolve any discrepancies and achieve consensus. Information that was collected was saved in a secure private folder at the hospital. No infant charts were allowed to leave the premises. Per this hospital standard of care and protocol, the TIMP was administered just prior to discharge; TIMP scores for each infant were recorded on the data abstraction form.
Data analysis
Data were analyzed using Statistical Package for the Social Sciences version 25 (SPSS) and Stata 15. Descriptive statistics were used to summarize demographics and frequency counts for sensory system intervention delivery, parent education and presence, and TIMP scores were computed. Pearson’s Correlation coefficient was used to evaluate the relationship between interval and ratio level data: total number of occupational therapy treatments and total number of minutes spent in therapy. The relationship between activity tolerance and number of occupational therapy visits were analyzed via a one-way ANOVA with a Bonferroni post-hoc analysis.
Results
The characteristics of 39 preterm infants who were born between 23 weeks and 28 weeks, six days gestation were completed and 24 (61%) were male and 15 (35%) were female. Over 50% demonstrated poor to fair activity tolerance at baseline. A summary of infant demographics and characteristics can be found in Table 1.
Distribution of Interventions Delivered in the NICU
aResults from this study support a hierarchical systematic approach to facilitate sensory system development. Tactile/ proprioceptive and vestibular interventions were utilized most frequently and auditory and visual treatments less frequently. Table 2 summarizes the total mean frequency of sensory-based treatments as well as individual subtype treatments organized by sensory system development.
Neuromotor and Developmental Outcomes
Table 3 outlines the distribution of TIMP categories based on percentile rank of the infants (far below average, below average, low average, and average) by subject groups. The total number of occupational therapy treatments was not significant for predicting higher TIMP scores (t(8)=.044; p=0.795). From this sample, 33.3% of infants performed in the below average category and 53.8% of infants performed in the average category, the highest category achievable on the TIMP.
Activity Tolerance and Interventions
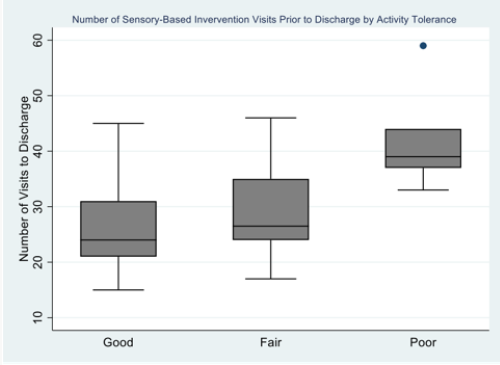
A one-way between-subjects ANOVA with a Bonferroni posthoc analysis was conducted to assess the relationship between activity tolerance upon initial evaluation and the mean number of occupational therapy visits to discharge. The mean number of occupational therapy visits varied significantly across activity tolerance categories such that infants with poor activity tolerance upon initial evaluation had a significantly higher number of occupational therapy visits to discharge compared to infants with good activity tolerance upon initial evaluation [F(2)= 6.176 p= .005; p<.05]. Figure 1 displays a box-plot of median frequency of visits delivered by occupational therapists and speech-language pathologists in relation to activity tolerance upon initial evaluation categorized by good, fair, and poor.
Discussion
Systematic Sensory-Based Interventions
Sensory system development occurs sequentially in the following order of maturation: tactile/proprioceptive, vestibular, gustatory/ olfactory, auditory, and visual [6]. Infants born prematurely do not have the ability to fully develop all these sensory systems prior to leaving the uterus. Therefore, these infants are at a high risk for developmental problems later in life which most commonly include sensory processing disorders, motor incoordination, cognitive dysfunction, learning disabilities, and mental health disorders [21]. Recent studies have found that premature infants are at increased risk of autism spectrum disorders, neurosensory impairment, cognitive impairment and delayed social-emotional engagement due in part to atypical sensory processing patterns [21]. It is imperative that the premature infant receive therapeutic intervention in the first two years of life, as this time period is crucial for neurodevelopmental plasticity and may have lifelong benefits for the infant’s health and well-being [21].
Consistent with the SDT model and NICU lead occupational therapist, early intervention for preterm infants follows a hierarchal order and aids in the infant achieving activity tolerance and self-regulation [8,10]. Available research is limited examining developmental sensory-based occupational therapy interventions in the NICU and their impact on neurodevelopmental outcomes. This study focused on describing the distribution of sensory-based interventions for premature infants and the effect these treatments had on the infants’ neuromotor and developmental outcomes. Upon initial evaluation, occupational therapists developed an individualized care plan based on the responsiveness of each infant’s competencies, emerging abilities, and vulnerabilities in relation to sensory and motor development, activity tolerance, and medically complex factors. Occupational therapy interventions began when the infant reached 30 weeks gestational age and were provided throughout the infant’s stay in the NICU per the infant’s activity tolerance.
Sensory-based interventions were delivered in order of sensory/perceptual system development as “out of sequence stimulation of one system interferes with development” (p. 10) [6,10]. The goal for each infant was to “achieve self-regulation, normal development, and normal sensory processing” (p. 14) [10]. A key finding in this study was that the frequency of treatments indicated a specific delivery method of interventions based on sensory system development. Results from this study indicated that treatments most commonly provided were tactile/proprioceptive interventions as this system develops first, and fewer visual treatments as infants were likely discharged before visual treatment was developmentally appropriate. Specific protocols including music therapy, cycled lighting, and positioning were implemented in this NICU as the infant could tolerate these levels of stimulation. Occupational therapists often provided education on protocols which were then carried out by nursing.
TIMP and Related Outcomes
The second main finding was that there was no relationship between the type and frequency of OT treatments and individual discharge TIMP scores. Although the correlation between TIMP categories and frequency of therapy services was not statistically significant in this study, the results were clinically significant. While 33.3% of infants in this high-risk group performed in the below average category, this correlated with other research studies that showed high-risk infants received below average TIMP scores when compared to low-risk infants who were more likely to receive TIMP scores in the average range [22,23]. In comparison, 64.1% of infants in this study achieved scores in the low average and average TIMP category range. This is clinically significant because these infants’ TIMP scores are comparable to infants’ TIMP scores born closer to full-term [23]. One reason for lower TIMP scores for higher risk infants may be that infants who were born more prematurely and/or exhibit lower birth weights had a higher frequency of developmental disorders [23].
Overall, infants born prematurely typically presented with lower scores on assessments when compared to infants born at term, even when the assessment was adjusted for prematurity due to medical complications associated with premature birth [24]. Past research has shown that referrals to therapy while in the NICU showed the highest correlation with changes in TIMP scores and that infants who received therapeutic services made greater changes on the TIMP when compared to infants who did not receive therapeutic services [25]. It is clinically relevant to note discharge factors and readmission rates for preterm infants whom were discharged from this Level III NICU. According to a recent study, unadjusted readmission rates for infants discharging from NICUs across various geographic regions ranged from 2.2-28.4% within 7-14 days of discharge and were noted to be between 2.7-34.4% within a year of discharge [26]. Infants in this study demonstrated with a 10.3% rate of readmission to the hospital, which was lower than average.
Additionally, 0% of infants from this study were discharged with a G-tube. This is significant because according to a recent study, one-third of infants who were discharged home from the NICU with a G-tube had at least one emergency department visit and 9% had multiple emergency department visits due to G-tube-related complications [27]. Finally, 7.7% of infants in this study were discharged home with oxygen indicating lower rate of bronchopulmonary dysplasia in infants at discharge. While various factors may contribute to an infant’s discharge status and potential for readmission, sensory-based occupational therapy treatments promote central nervous system neurodevelopment as demonstrated by the infant’s ability to tolerate treatment and serves as a contributing factor to an infant’s success in the NICU and beyond discharge.
Activity Tolerance
The third main finding of the study was that there was an association between activity tolerance and total number of sensory-based visits. Activity tolerance was examined and documented upon each infant’s initial evaluation. Due to a lack of available standardized assessments for premature infants at birth, this NICU utilized an informal assessment for each infant upon initial evaluation including assessing the infant’s quality of movement, muscle tone, and reflexes. An infant’s activity tolerance was continuously monitored throughout occupational therapy interventions. This study found that infants who exhibited poor activity tolerance upon initial evaluation received a higher frequency of sensory-based interventions when compared to infants who had fair or good activity tolerance upon evaluation to ameliorate neurodevelopment, as presented in Figure 1. This is clinically significant because infants who presented with poor initial activity tolerance tended to have longer lengths of stays within the NICU and received higher rates of sensory-based treatments prior to discharge from the NICU.
Collectively, these findings suggest that occupational therapists need be involved in the screening, assessment, and treatment of high-risk infants in the NICU for problems related to development and sensory processing. Sensory processing dysfunction has the potential to influence the development of play, social participation, education, and self-care occupations, all of which are considered to be within the scope of occupational therapy [28].
Implications for Practice and Directions for Future Research
Occupational therapy services continue to develop and emerge within Level III and IV NICUs. This research outlined specific sensory-based treatments that occupational therapists performed using advanced skills in the NICU. Occupational therapists may use this systematic delivery of services to plan intervention strategies for infants in other NICUs. Increased education and training on sensory system developmental will lead to an increase in consistency of care and documentation provided by occupational therapists in NICUs across the country and improve the rate of premature infants who achieve a pre-discharge average category score on the TIMP. Prior to a premature infant being discharged from the NICU, it is crucial for therapists to provide parent/caregiver education related to the infant’s sensory system development, progression, and appropriate stimulation techniques. This study provides a resource for specific entry-based interventions according to each sensory system that parents may include into their infant’s daily routine.
It is recommended that occupational therapists support parenting roles and relationships and provide appropriate engagement in the infant’s care [21]. While this study focused primarily on sensory-based occupational therapy treatments in the NICU, there are many other areas that occupational therapists address which aid in infant development. These areas are within occupational therapy’s scope of practice and include, but are not limited to, positioning, feeding, parent education and support, facilitating kangaroo care, and pain management. Parental education should focus on continued infant development following discharge from the NICU with referral for early intervention [21]. Future studies could expand upon the inclusion criteria to allow for larger a sample size. More research is needed to provide further insight on the longitudinal effects of occupational therapy interventions following discharge from the NICU. Future research could analyze the impact that occupational therapy intervention has on neurodevelopment and sensory system integration and the parent/caregiver role in providing these treatments beyond discharge from the NICU.
Limitations
This study has several limitations. First, the data collection process form was self-developed and has not undergone examination for psychometric properties. The small sample size was due to the high medical complexity and comorbidities presented from extremely premature birth, limiting generalizability to other NICUs. Therapists did not complete a scored standardized assessment upon admission but evaluated activity tolerance, quality of movement, muscle tone, and reflexes. Some interventions in this study may have presented with lower frequency due to methods of documentation and data collection protocols. Throughout the data collection process, discrepancies of documentation were noted among practitioners. While therapists within this NICU used the same systematic approach for developmentally appropriate interventions, some specific interventions may have been listed under varying names. This further supports the need for consistent documentation and clarification of treatments within the NICU.
Such discrepancies were resolved with the occupational therapist who was the primary provider for these infants. A lower frequency of containment holds was reported in this study due to data collection protocol of only accounting for the interventions when it was the sole treatment provided by the occupational therapist. Containment holds were typically performed at the start of each treatment session and throughout to facilitate the infant’s coping skills [10]. Finally, olfactory/gustatory interventions that were included within this study for sensory-based interventions were delivered by speech-language pathologists in this Level III NICU. Although the occupational therapist may have been present during treatment for facilitation of the infant’s coping skills, speech-language pathologists primarily performed the gustatory/ olfactory treatments at this NICU when the interventions were developmentally appropriate. Speech treatments typically occurred 3x/week and interventions were distributed following sensory system development in relation to speech-related items.
Speech treatments typically began with tactile arousal to the mouth, such as placing breast milk on the pacifier, and continued along the sensory system progression to gustatory/olfactory treatments when developmentally appropriate. However, delivery of gustatory/olfactory treatments can also be classified within occupational therapist’s scope of practice and could be performed by occupational therapists within other NICUs.
Conclusion
This study examined the sequence of occupational therapy interventions based on a sensory-system development approach in accordance with neuromotor and developmental milestones in NICU infants. Type and frequency of interventions were implemented based on system development and graded appropriately in accordance with activity tolerance. This study demonstrated the vitality of occupational therapy’s presence in the NICU promoting the need for consistency of interventions among neonatal therapists. Further inquiry with a larger sample size is warranted to explore the type, frequency, and systematic delivery of sensory-based occupational therapy interventions for preterm infants.
Conflicts of Interest
The authors declare no conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Hughes AJ, Redsell SA, Glazebrook C (2016) Motor development interventions for preterm infants: A systematic review and metaanalysis. Pediatrics 138(4): e20160147.
- Behrman RE, Butler AS (2007) Preterm birth: Causes, consequences, and prevention. National Academies Press, Washington DC, USA.
- Farin Soleimani, Farzaneh Zaheri, Fatemeh Abdi (2014) Long-term neurodevelopmental outcomes after preterm birth. Iran Red Crescent Med J 16(6): e17965.
- Riley LE, Stark AR, Kilpatrick SJ, Papile IA (2012) Guidelines for perinatal care (7th edn.) American Academy of Pediatrics. Illinois, USA.
- Wanda Denise Barfield (2012) Levels of neonatal care pediatrics. American Academy of Pediatrics. Pediatrics 130(3): 587-597.
- Blackburn S (2007) Sensory system development and capacities in preterm infants and implications for care. Presented at Developmental Interventions in Neonatal Care. Las Vegas, USA.
- Liaw J (2000) Tactile stimulation and preterm infants. Journal of Perinatal & Neonatal Nursing 14(1): 84-103.
- Agata Maltese, Beatrice Gallai, Rosa Marotta, Francesco Lavano, Serena Arianna Lavano, et al. (2017) The synactive theory of development: The keyword for neurodevelopmental disorders. Acta Medica Mediterranea 33(2): 1257-1263.
- Fucile S, Gisel E (2010) Sensorimotor interventions improve growth and motor function in preterm infants. Neonatal Network 29(6): 359-366.
- . Lisa Bader (2017) The ladder approach: A systematic approach to the delivery of therapy services in the NICU. Omaha, USA.
- Case Smith J, O Brien J (2014) Occupational Therapy for Children and Adolescents (7th edn.) Elsevier Mosby. St. Louis, USA.
- Fucile S, Gisel EG, Lau C (2005) Effect of an oral stimulation program on sucking skill maturation of preterm infants. Developmental Medicine and Child Neurology 47(3): 158-162.
- Stanley N Graven, Joy V Browne (2008) Auditory development in the fetus and infant. Newborn and Infant Nursing Reviews 8(4): 187-193.
- Jacqueline M McGrath, Sharon Cone, Haifa A Samra (2011) Neuroprotection in the preterm infant: Further understanding of the short- and long-term implications for brain development. Newborn and Infant Nursing Reviews 11(3): 109-112.
- Glass HC, Costarino AT, Stayer SA, Brett CM, Cladis F, et al. (2015) Outcomes for extremely premature infants. Anesthesia and analgesia 120(6): 1337-1351.
- Larocque K, Heon M, Aita M, Lacroix A (2015) Educational intervention on preterm infants’ behaviours for the promotion of parental confidence. Infant 11(5): 170-174.
- Gay Girolami (2015) Test of Infant Motor Performance.
- Campbell SK, Kolobe TH, Wright BD, Linacre JM (2002) Construct validity of the Test of Infant Motor Performance. Developmental Medicine and Child Neurology 44(4): 263-272.
- Campbell SK, Girolami GL, Thubi HA, Osten ET, Lenke MC (2001) Test of Infant Motor Performance Verson 5.1. Infant Motor Performance Scales, LLC. USA.
- Als H, Duffy FH, McAnulty GB, Rivkin MJ, Vajapeyam S, et al. (2004) Early experience alters brain function and structure. Pediatrics 113(4): 846- 857.
- . Royal College of Occupational Therapists (2017) Occupational therapy in neonatal services and early intervention: Practice guideline.
- Coker Bolt P, Woodbury ML, Perkel J, Moreau NG, Hope K, et al. (2014) Identifying premature infants at high and low risk for motor delays using motor performance testing and MRS. Journal of Pediatric Rehabilitation Medicine 7(3): 219-232.
- Giachetta L, Nicolau CM, Juliani RC, de Carvalho WB, Krebs VL (2016) Characterization of motor performance of newborns in a neonatal unit of tertiary level. Revista Da Associacao Medica Brasileira 62(6): 553- 560.
- Snider L, Majnemer A, Mazer B, Campbell S, Bos AF (2009) Prediction of motor and functional outcomes in infants born preterm assessed at term. Pediatric Physical Therapy 21(1): 2-11.
- Rose RU, Westcott SL (2005) Responsiveness of the Test of Infant Motor Performance (TIMP) in infants born preterm. Pediatric Physical Therapy 17(3): 219-224.
- Lorch S, Macheras M (2014) Hospital-level variation in readmission rates of neonatal intensive care (NICU) patients: A potential quality measure. Archives of Disease in Childhood 99(2): A1-A620.
- Khalil ST, Uhing MR, Duesing L, Visotcky A, Tarima S, et al. (2016) Outcomes of Infants with Home Tube Feeding: Comparing Nasogastric vs Gastrostomy Tubes. JPEN J parenter enteral nutr 41(8): 1380-1385.
- American Occupational Therapy Association (2015). The role of occupational therapy with children and youth.