Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Case Report(ISSN: 2690-5752) 
Zenker Diverticulum: Pathophysiology, Clinical Presentation, and Therapeutic Management Volume 9 - Issue 5
Niema Benkhraba1,3, Mohamed Ali Gliti1,3*, Moncef Delouane1, Razika Bencheikh2,3, Mohamed Anas Benbouzid2,3, Abdelilah Oujilal2,3 and Leila Essakalli Houssyni2,3
- 1Resident physician in otolaryngology, Department of Otolaryngology, Head and Neck Surgery, Ibn Sina University Hospital, Rabat, Morocco
- 2Professor of otolaryngology, Department of Otolaryngology, Head and Neck Surgery, Ibn Sina University Hospital, Rabat, Morocco
- 3Faculty of Medicine and Pharmacy of Rabat, Mohamed V University, Rabat, Morocco
Received: April 14, 2023; Published: April 27, 2023
Corresponding author: Mohamed Ali Gliti, ENT Department, Rabat Specially Hospital, Ibn Sina University Hospital, Hafiane cherkaoui Avenue, 10100 Rabat, Morocco
DOI: 10.32474/JAAS.2023.09.000328
Abstract
Zenker diverticulum (ZD) is attributed to a poorly compliant cricopharyngeus muscle, and the mainstay of treatment is a cricopharyngeal myotomy. We report the case of a patient of 78 years, diagnosed with Zenker diverticulum and we report diagnostic and therapeutic modalities.
Keywords: Zenker diverticulum; Myotomy; Diverticulectomy; Endoscopy
Introduction
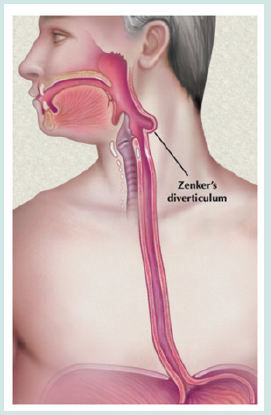
Zenker diverticulum (ZD) is a pulsion diverticulum that occurs in a natural weakness: the triangular shaped area of the posterior wall of the hypopharynx, which is bordered by oblique muscle fibers of the inferior pharyngeal constrictor and the horizontal muscle fibers of the cricopharyngeal muscle and is called Killian triangle. The cricopharyngeus marks the beginning of the esophagus and is a part of the upper esophageal sphincter (UES) [1–3]. The wall of the pseudo-diverticulum consists of mucosa and submucosa that bulge as a result of increased intraluminal pressure caused by incoordination between these muscles, and as a consequence of incomplete relaxation of the cricopharyngeus and the UES in a swallowing reflex. Cricopharyngeal myotomy remains a key element of surgical treatment of Zenker diverticulum (ZD) [2,4]. Although there is a lack of randomized clinical trials, surgeons favor minimally invasive endoscopic techniques – stapling or laser diverticulostomy – be cause they are believed to cause fewer complications and produce similar outcomes to classic trans-cervical repair [5–8].
Case Report
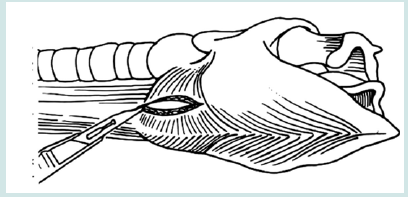
Patient of 78 years who had a progressive aggravation of swallowing disorders with weight loss estimated at more than 5kg (Figure 1). Oesogastroduodenal transit showed evidence of a Zenker Diverticulum developed at the expense of the upper third of the esophagus, on the posterior hypopharyngeal wall, remaining 45mm below the upper esophageal sphincter. This diverticulum measures 15*23*23. The patient was referred to our surgical team for management. We investigated her by performing a barium swallow which demonstrated a pharyngeal pouch (Zenker diverticulum). Treatment involves surgery with an external or endoscopic approach to eliminate the diverticular pouch. We started with oesophagoscopy which showed a large diverticulum, without food stasis. Due to the size of the diverticulum, we continue with an external cervical approach. The treatment consists on diverticulectomy with cricopharyngeal myotomy (Figures 2 & 3). Nasogastric tube has been inserted. The post-operative follow-up was simple. Barium swallow study was realized after one week, was normal (Figure 4). The patient resumes the oral diet. The evolution was favorable. The histological study shows an esophageal diverticulum.
Discussion
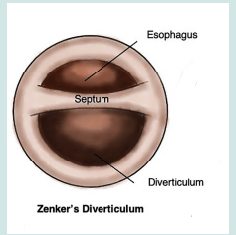
Zenker diverticulum (ZD) was first described by Ludlow in 1769 [1]. However, it was Friedrich Von Zenker who recognized ZD results from increased intrapharyngeal pressure [2]. ZD, also termed cricopharyngeal diverticulum and pharyngoesophageal diverticulum, is located proximal to the upper esophageal sphincter (UES) usually on the posterior hypopharyngeal wall [3]. A tissue bridge composed of mucosa, submucosa, connective tissue, and muscle between the lumen of esophagus and diverticulum is present. Inadequate relaxation of the cricopharyngeal muscle leads to outflow obstruction creating a zone of high pressure in the hypopharynx. Fibrosis of muscle fibers and progressive tension over the esophageal wall results in formation of a diverticulum [4]. Zenker diverticulum usually occurs between the seventh and eighth decades of life, and rarely before the age of 40 years [5]. It occurs predominately in men. The prevalence of ZD among the general population is believed to be between 0.01% and 0.11% [6]. However, the true incidence of ZD is difficult to establish since the number of asymptomatic patients is unknown. Although several symptoms may be present, 80– 90% of patients complain of dysphagia. Regurgitation of undigested foods, halitosis, and hoarseness can also occur. Cervical borborygmi is almost pathognomonic of ZD [7].
As the pouch enlarges, symptoms become more severe with resultant weight loss and malnutrition. As many as 30–40% of patients describe chronic cough and repeated episodes of aspiration, some with aspiration pneumonia. Symptoms may be present for weeks to several years. A sudden increase in the severity of dysphagia and regurgitation and/or development of alarm symptoms such as local pain and hemoptysis or hematemesis may signal the presence of squamous cell carcinoma within the ZD which has an incidence of 0.4–1.5% [7]. Other pathologies associated with ZD include laryngocoele, leiomyoma, polymyositis, cervical esophageal web, carotid body tumor, anterior cervical fusion, stenosis of upper esophagus, hiatus hernia, and gastroesophageal reflux. These coexisting pathologies are not directly associated with or caused by ZD but can be additional causes of dysphagia in patients with ZD. Gastroesophageal reflux (GER) has been implicated in the genesis of ZD. Physical examination findings are few and are usually seen in more severe cases. They include findings of malnutrition, voice changes, neck mass, cervical borborygmi and crepitus. In most cases, the diagnosis of ZD is suspected based on clinical symptoms and confirmed by esophageal studies. Complications of untreated ZD include retained foreign body, tracheal fistula, vocal cord paralysis, fistula to the prevertebral ligament with cervical osteomyelitis, peptic ulceration, and hemorrhage [7].
Surgical treatment of ZD can be categorized as either external or endoscopic. Traditionally, an open transcervical resection of ZD was the treatment of choice [7]. However, as the underlying contribution of the cricopharyngeus to the pathophysiology of ZD was appreciated, a CP myotomy, with or without diverticulopexy or diverticulectomy, gained favor as a significant component of the surgical therapy. Once the diverticulum is exposed through an external approach, there remain several options to manage the diverticulum including diverticulectomy followed by hand sewn closure or applying a staple-assisted device to complete both the resection and closure of the esophagotomy. These open techniques must be accompanied by a myotomy to address the underlying pathophysiology and prevent recurrence. Earlier on in the evolution of managing ZD, to avoid the concern of post-diverticulectomy dehiscence and leaking, the techniques of diverticulopexy and diverticular imbrication were designed to negate an esophagotomy. Diverticulopexy involves suturing the base of the diverticulum to the prevertebral fascia or pharyngeal constrictors, whereas diverticular imbrication involves tying a purse string around the diverticulum followed by inversion into the lumen [8,9]. However, diverticulopexy is asso ciated with a higher recurrence rate, and inversion is likely only beneficial for a small diverticulum. Furthermore, with careful attention to sewing techniques, particularly the canal stitch, as well as the reliability of the gastrointestinal anastomotic stapler, leaking postdiverticulectomy has become much less of a concern. Although the risks of diverticulectomy are low, they must be considered and discussed with the patients. These include mediastinitis, recurrent laryngeal nerve injury, pneumonia, hematoma, and infection.
Separating the sternocleidomastoid muscle and the strap muscles is incised and the carotid sheath is gently retracted laterally. Blunt dissection is carried down onto the esophagus and posterolaterally to the prevertebral fascia exposing the diverticulum. The diverticulum is grasped with a Babcock and suspended superolaterally to allow for the diverticulectomy to be performed. When available, an endostapler is used to simultaneously perform the diverticulectomy and pharyngeal repair. Alternatively, a diverticulectomy can be performed with a scissor or scalpel, and a 3–0 Vicryl on a tapered needle is used to perform vertical canal stitches in an interrupted fashion. Inferior to the diverticulum the dysfunctional cricopharyngeus is exposed and a myotomy is performed using a fresh scalpel. A nasogastric tube is inserted, and the patient is kept NPO for 48 hours, after which a barium swallow study is performed before resumption of an oral diet. When only a small diverticulum is present, or in the case of a symptomatic cricopharyngeal bar, a myotomy alone is performed. The cricopharyngeus is exposed as described earlier. These patients can resume an oral liquid diet following a barium swallow study on the first postoperative day (Figures 5-7).
Although Mosher and colleagues reported the first endoscopic management of ZD in 1917, it was not until the 1960s that Dohlman and Mattson reported a large series of successful endoscopic management with a specially designed laryngoscope (Dohlman diverticuloscope) (Figure 8) to isolate the partying wall separating the diverticulum from the esophagus [10]. Although they reported the use of electrocautery, more recent series have reported on the success of using the CO2, KTP, or Argon laser [11]. The next significant development was the introduction of the endoscopic stapling device, which has since become the method most commonly used [12]. The critical step in this technique is adequate exposure of the partying septum; this may be difficult in patients with prominent teeth, cervical kyphosis, retrognathia, or temporomandibular joint disease. These factors contribute to an overall 5% conversion rate to open surgery. When exposure is not hindered, this minimally invasive technique is quick and associated with much less morbidity compared with open surgery. This technique has a reported leak rate that is negligible and is associated with an overall 5% recurrence rate. However, the endoscopic stapling technique cannot effectively address small diverticula (<2cm). For small diverticula (<2cm) and associated cricopharyngeal bars, an endoscopic laser technique can be implored. In fact, lasers have been used recently during upper endoscopy to respect the diverticulum instead of staples. Overall, lasers have been shown to have fewer recurrences and faster improvement in symptoms compared to the use of staplers.
Conclusion
The treatment of choice, for both small and large diverticula, remains rigid endoscopic management; this is associated with a 95% success rate and minimal morbidity. With the lack of randomized controls trials comparing the different endoscopic techniques, surgeon comfort and training remain the most important factor for successful endoscopic management. Open surgery is reserved for failed endoscopic therapy or inability to provide adequate endoscopic exposure and is associated with excellent results albeit with an increased morbidity compared with endoscopic techniques.
References
- Anagiotos A, Preuss SF, Koebke J (2010) Morphometric and anthropometric analysis of Killian’s triangle. Laryngoscope 120(6): 1082-1088.
- Broniatowski M, Sonies BC, Rubin JS (1999) Current evaluation and treatment of patients with swallowing disorders. Otolaryngol Head Neck Surg 120(4): 464-473.
- Westrin KM, Ergun S, Carlsoo B (1996) Zenker’s diverticulum-a historical review and trends in therapy. Acta Otolaryngol 116(3): 351-360.
- Dzeletovic I, Ekbom DC, Baron TH (2012) Flexible endoscopic and surgical management of Zenker’s diverticulum. Expert Rev Gastroenterol Hepatol 6(4): 449-465.
- Ekberg O, Lindgren S (1986) Gastroesophageal reflux and pharyngeal function. Acta Radiol Diagn (Stockh) 27(4): 421-423.
- Zaninotto G, Costantini M, Boccu C (1996) Functional and morphological study of the cricopharyngeal muscle in patients with Zenker’s diverticulum. Br J Surg 83(9): 1263-1267.
- Butcher RB, Larrabee WF (1979) Surgical treatment of hypopharyngeal (Aenker’s) diverticulum. Arch Otolaryngol 105(5): 254-257.
- Holinger PH, Schild JA (1969) The Zenker’s (hypopharyngeal) diverticulum. Ann Otol Rhinol Laryngol 78(4): 679-688.
- Johnson JT, Weissman J (1992) Diverticular imbrication and myotomy for Zenker’s. Laryngoscope 102(12 Pt 1): 1377-1378.
- Dohlman G, Mattsson O (1960) The endoscopic operation for hypopharyngeal diverticula: a roentgen cinematographic study. AMA Arch Otolaryngol 71: 744-752.
- Wouters B, van Overbeek JJ (1990) Pathogenesis and endoscopic treatment of the hypopharyngeal (Zenker’s) diverticulum. Acta Gastroenterol Belg 53(3): 323-329.
- Collard JM, Otte JB, Kestens PJ (1993) Endoscopic stapling technique of esophagodiverticulostomy for Zenker’s diverticulum. Ann Thorac Surg 56(3): 573-576.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...