
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Case Report(ISSN: 2641-1709) 
Trans Oral Robotic Surgery (TORS) for Treatment of Tongue-Base Angioleiomyoma Volume 8 - Issue 2
Einav G Levin*, Gideon Bachar and Uri Alkan
- Department of Otolaryngology & Head and Neck Surgery, Rabin Medical Center, Petah Tikva and Sackler Faculty of Medicine, Tel Aviv University, Israel
Received: April 01, 2022; Published: April 12, 2022
Corresponding author: Einav G. Levin, Department of Otorhinolaryngology – Head and Neck Surgery Rabin Medical Center, Petah Tikva, Israel
DOI: 10.32474/SJO.2022.08.000281
Abstract
Angioleiomyoma is a benign vascular neoplasm that rarely occurs in the head and neck, particularly the oropharynx. This report aimed to highlight a rare case of tongue-base angioleiomyoma excised by transoral robotic surgery (TORS). A rare case report of angioleiomyoma of the tongue base in a 72-year-old man who presented with hoarseness, muffled voice, and stridor. Preoperative endovascular embolization was performed owing to the high vascularity of the lesion, followed by TORS using the da Vinci Robotic System. The tumor was excised completely with minimal complications. There were no signs of local recurrence during the followup period. Tongue-base angioleiomyoma poses treatment challenges owing to its vascularity and difficult location. We suggest that the appropriate treatment of tongue-base angioleiomyoma should consist of embolization and tracheostomy, followed by TORS excision. To our knowledge, this is the first use of robotic minimal invasive technique for excision of angioleiomyoma in this location.
Keywords: Angioleiomyoma; tongue base; transoral robotic surgery (TORS)
Introduction
Angioleiomyoma (ALM) is a benign soft-tissue tumor originating in the smooth muscle of blood vessels. It usually measures from a few millimeters to 2 cm. As the tumor is painless and slow-growing, diagnosis may be delayed. Median age at diagnosis is 45 years; there is a small male predominance (58%) [1]. ALM appears histologically as a well-circumscribed capsulated tumor; alpha-smooth muscle actin (SMA) positivity on immunohistochemistry is considered a good diagnostic marker [2]. Treatment is by surgical excision. Recurrence is uncommon, unless the tumor was not removed completely, and prognosis is good. Malignant transformation has not been reported [3]. ALM rarely occurs in the oropharynx and oral cavity, especially the tongue base. This report describes a case of tongue-based ALM and the first use of transoral robotic surgery (TORS) for the treatment of ALM in this location.
Case Presentation
Case history
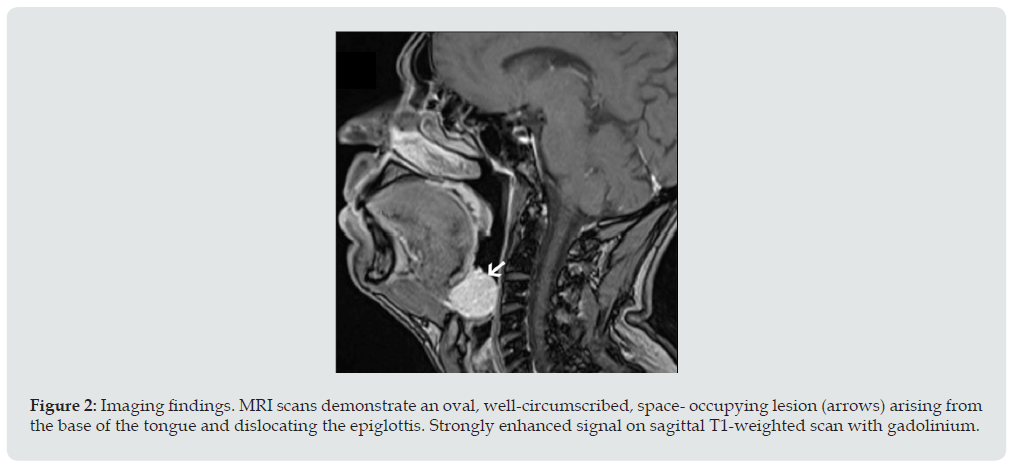
A 72-year-old man presented with hoarseness, muffled voice, stridor, and mild dyspnea that appeared during minor physical activity, in addition to unintentional weight loss of 4 kg in the last year. His medical history was remarkable. Clinical examination revealed an oropharyngeal tongue-base lesion and an offensive smell from the oral cavity. Laryngoscopy exposed a vascular 2.6 cm mass pushing the epiglottis posteriorly and filling the vallecula inferiorly (Figure 1). Magnetic resonance imaging (MRI) revealed an oval well-circumscribed space-occupying lesion located between the tongue base and epiglottis, hyperintense throughout and strongly enhanced on T2-weighted scans. The lesion caused partial obstruction of the oropharyngeal airways with slight asymmetry to the left (Figure 2). No metastases were identified. Considering the benign appearance of the tumor and its high vascularity, a preoperative biopsy was not taken to avoid the risk of excessive bleeding which could lead to airway obstruction. Accordingly, concerns of intraoperative bleeding prompted the use of preoperative endovascular embolization, which was performed by an invasive neuroradiologist under general anesthesia. Diagnostic catheter angiography demonstrated that the left lingual artery was the sole supply source to the lesion. Therapeutic catheterization was followed by endovascular embolization using a coaxial catheter system. During navigation of the microcatheter, minor bleeding was observed from the artery supplying the tumor and promptly stopped with liquid embolic glue. Total devascularization of the tumor-feeding artery was achieved without complications. The absence of distal obstructions was verified by injections to the vertebral arteries.
Figure 1: Laryngology findings. Preoperative laryngoscopic examination exposes vascular mass of diameter 2.6 cm in the tongue base, dislocating the epiglottis
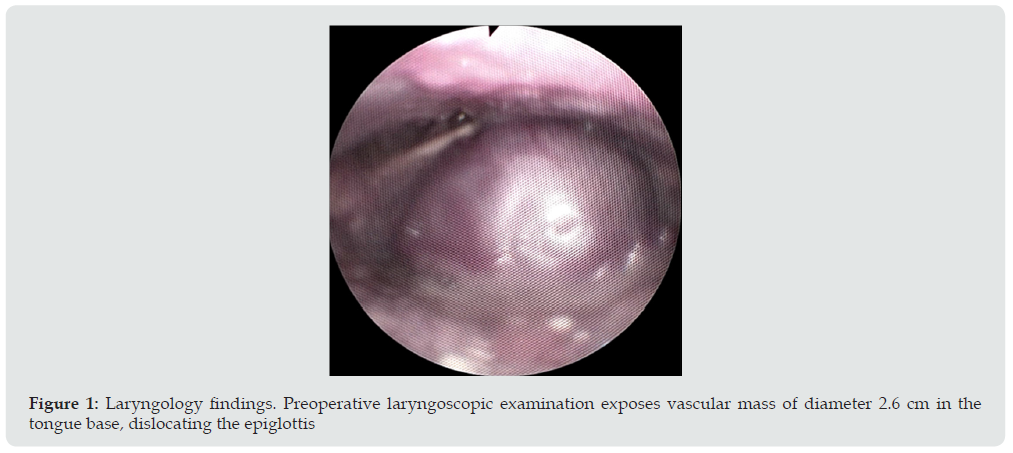
Figure 2: Imaging findings. MRI scans demonstrate an oval, well-circumscribed, space- occupying lesion (arrows) arising from the base of the tongue and dislocating the epiglottis. Strongly enhanced signal on sagittal T1-weighted scan with gadolinium.
TROS was performed under general anesthesia 3 days later (Figure 3). Surgery was preceded by preventive tracheotomy for intraoperative protection of the airway and safer postoperative management. The tongue base was exposed using a Crowe retractor, and visualization of the oropharynx was achieved with an 8 mm, 30-degree, three-dimensional endoscope that was inserted, facing upward, through the retractor. A 5 mm monopolar cautery and 5 mm Maryland dissector were then inserted and brought into endoscopic view. The tumor was excised enbloc with 0.5 cm margins using the da Vinci Robotic System [Intuitive Surgical Inc., Sunnyvale CA, USA). The TORS procedure took 110 minutes. Moderate bleeding events occurring during the procedure were managed with electrocautery, vascular clips, and biological glue; there was no excessive intraoperative bleeding or other perioperative complications. The postoperative course was uneventful. The patient was fed via a nasogastric tube for the first 2 days and then proceeded to soft oral intake. He was treated with antibiotics (cefamezin and metronidazole) and decannulated prior to discharge within 5 days. At the 1-year follow-up, there were no signs of local recurrence, and the stoma was closed.
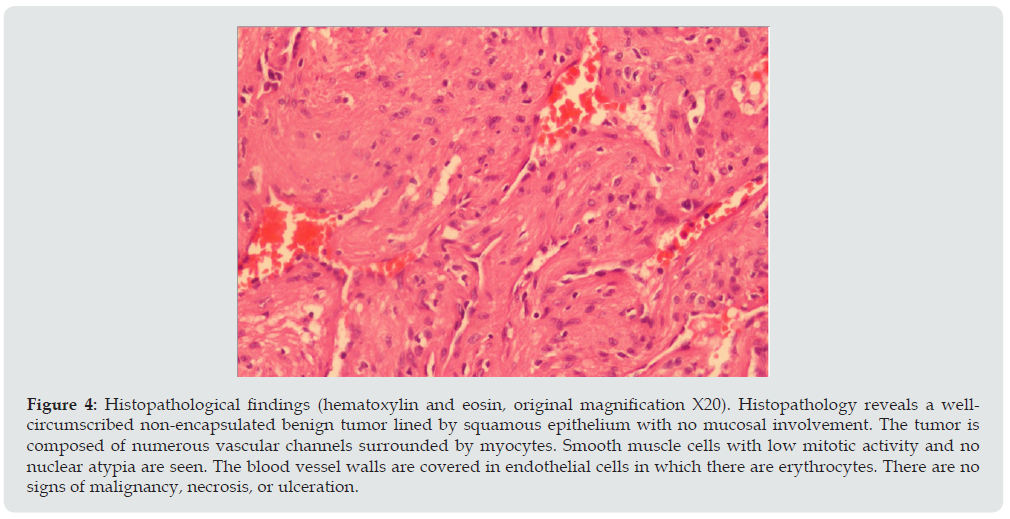
Postoperative histopathologic examination revealed a well-circumscribed 2.3-cm ALM composed of myocytes and vascular spaces, with no nuclear atypia and low mitotic activity. Immunohistochemistry staining was negative for HMB45, S100, and desmin, and positive for SMA. Ki67 proliferation index was 4-5%, indicating a benign neoplasm (Figure 4).
Figure 3: Intraoperative TORS images. The whole tumor (arrow) covered the epiglottis completely. Pushing the tumor aside exposes the epiglottis. The tumor was completely resected.
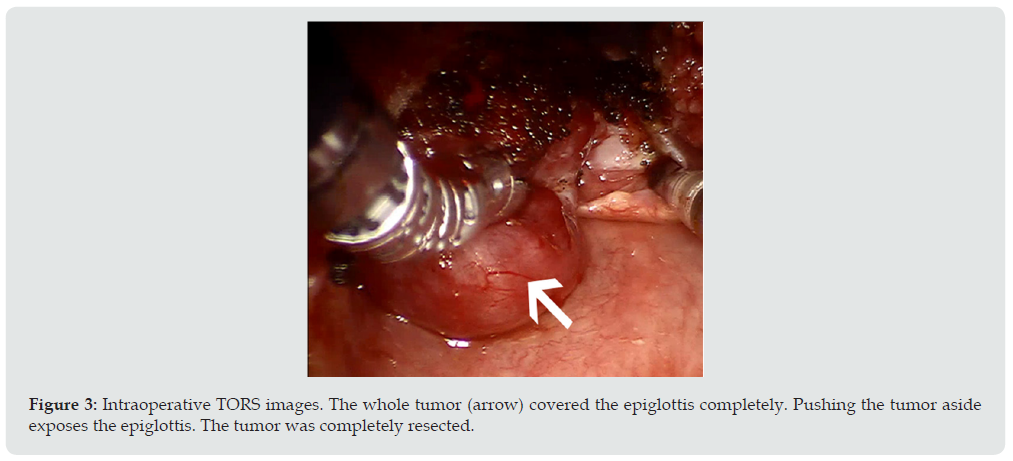
Figure 4: Histopathological findings (hematoxylin and eosin, original magnification X20). Histopathology reveals a wellcircumscribed non-encapsulated benign tumor lined by squamous epithelium with no mucosal involvement. The tumor is composed of numerous vascular channels surrounded by myocytes. Smooth muscle cells with low mitotic activity and no nuclear atypia are seen. The blood vessel walls are covered in endothelial cells in which there are erythrocytes. There are no signs of malignancy, necrosis, or ulceration.
Discussion
We presented a case of ALM in the tongue base. To our knowledge, a few cases of tongue ALM have been described, and only several specifically in the tongue base [4-6]. The clinical differential diagnosis of ALM of the tongue includes hemangioma, lymphangioma, vascular malformation, abscess, lingual thyroid, and other benign mesenchymal tumors such as fibroma, neurofibroma, and granular cell lesion. In our case, the intense enhancement of the lesion on T2-weighted images and T1-weighted images with gadolinium pointed to a hypervascular pattern, narrowing the differential diagnosis to a vascular mass. Surgical approaches to tongue-base tumors include transoral excision, submandibular approach, suprahyoid or lateral pharyngotomy, and lip split with mandibulotomy. For small and well-encapsulated lesions, transoral excision is preferred. However, gaining adequate access to the tongue base can be challenging owing to its remote location and the presence of important neurovascular structures [7]. Fan et al. [8] used an ultrasonic harmonic scalpel with an advanced hemostasis mode in 12 patients with other tongue-base benign lesions. The technique yielded good outcomes with minimum complications but was limited by lack of depth perception and low visualization of the surgical field with inadequate lesion exposure [9].
More recently, Danic et al. [4] and Kim et al. [6] described two cases of tongue-base ALM, in a 76-year-old man and a 2-monthold infant, respectively, who underwent endoscopic surgery with a harmonic scalpel. Additionally, Marden et al. [5] managed a tongue-based ALM that bled vigorously during diagnostic biopsy with endovascular embolization followed one day later by hemiglossectomy with mass resection. In the present case, the vascularity of the tumor prompted our decision to perform preoperative endovascular embolization of the selective tumorfeeding branch (left lingual artery), as described by Marden et al. [5] followed by surgical excision. However, unlike the previous cases, [4-6] we used a TORS approach. TORS has been reported to overcome the limitations of traditional surgical methods and to improve surgeon dexterity, precision, and depth perception [10]. By providing three-dimensional visualization, it allows for complete tumor removal with fewer complications while preserving important structures and nerves. We found the procedure to be safe and efficient for excision of a tongue-base ALM. The main disadvantages of TORS are the relatively high operating costs and absence of tactile feedback. However, the advantages seem to outweigh the disadvantages. This report supports the use of a robotic minimal invasive technique for excision and partial glossectomy of benign lesions at the tongue base, especially vascular lesions like ALM.
In conclusion, we report a rare case of a tongue-base ALM that posed treatment challenges owing to its vascularity and difficult location. Treatment consisted of embolization and tracheostomy followed by TORS excision. To our knowledge, this is the first report documenting treatment of tongue-base ALM using TORS. We achieved optimal visual exposure that allowed for safe and complete tumor excision with minimal complications.
Acknowledgment
Conflict of Interest and Financial Disclosures: The authors have no funding, financial relationship, or conflicts of interest to disclose.
Funding: None
Previous Publication or Submission: The authors have not published any related papers from this study. The article is not under consideration for publication elsewhere at the time of manuscript submission.
Data availability statement: The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethics statement: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Wang CP, Chang YL, Sheen TS (2004) Vascular leiomyoma of the head and neck. Laryngoscope 114: 661-665.
- Yoon TM, Yang HC, Choi YD, Lee DH, Lee JK, et al. (2013) Vascular leiomyoma in the head and neck region: 11 years’ experience in one institution. Clin Exp Otorhinolaryngol 6: 171-175.
- Mahima VG, Patil K, Srikanth HS (2011) Recurrent oral angioleiomyoma. Contemp Clin Dent 2: 102-105.
- Danic D, Hadzibegovic AD, Stojadinovic T, Damjanovi D, Gudelj A, et al. (2012) Harmonic scalpel surgical treatment of the tongue angioleiomyoma- Case report and review of the literature. Coll Antropol 36(2): 167-170.
- Marden FA, Calilao GC, Guzman G, Roy SS (2004) Glossal angiomyoma imaging findings and endovascular treatment. Head Neck 26: 1084-1088.
- Kim YH, Jang YW, Pai H, Kim SG (2010) Congenital angiomyoma of the tongue - case report. Dentomaxillofac Radiol 39: 446-448.
- Sitenga JL, Aird GA, Nguyen A, Vaudreuil A, Huerter C (2017) Clinical features and surgical treatment of schwannoma affecting the base of the tongue: A systematic review. Int Arch Otorhinolaryngol 21: 408-413.
- Fan S, Zhang DM, Chen WL (2017) Endoscopy-assisted resection of benign lesions on the base of the tongue via the transoral approach using a harmonic scalpel. Oral Maxillofac Surg 75: 2242-2247.
- Folk D, D’Agostino M (2017) Transoral robotic surgery vs. endoscopic partial midline glossectomy for obstructive sleep apnea. World J Otorhinolaryngol-Head Neck Surg 3: 101-105.
- O’Malley BW, Weinstein GS, Snyder W, Hockstein NG (2006) Transoral robotic surgery (TORS) for base of tongue neoplasms. Laryngoscope 116: 1465-1472.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




