
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Case Report(ISSN: 2641-1709) 
The Migration of a Fish Bone into Posterior Cervical Space Volume 7 - Issue 1
Nguyen Nguyen1*, Thanh Thai Le1, Duy Huy Nguyen3, Thi My Duong1 and Kyu Sung Kim2
- 1Department of Otolaryngology, Hue University of Medicine and Pharmacy, Hue University, Vietnam
- 2Department of Otolaryngology Head & Neck Surgery, Inha University Hospital, Korea
- 3Department of Otolaryngology, Hue City Hospital, Vietnam
Received:June 26, 2021; Published:July 07, 2021
Corresponding author: Nguyen Nguyen, Department of Otolaryngology, Hue University of Medicine and Pharmacy, Hue University, Vietnam
DOI: 10.32474/SJO.2021.07.000254
Abstract
Esophageal foreign bodies are commonly encountered in otolaryngology clinic. The most common esophageal foreign bodies are fish bones which are encountered in Southeast Asia and in Vietnam. The rare complication due to the ingested foreign body is its migration to the deep neck space and the formation of cervical abscess. This case depicts a patient with a fish bone in the esophagus that migrated extraluminally into the posterior cervical space. Moreover, the difficulties in removing the foreign body as well as the management of esophageal perforation are described in detail.
Keywords:Fish bone; Esophageal perforation; Migration; Posterior cervical space
Introduction
Accidental ingestion of fish bone being lodged in the esophagus is a common emergency in otolaryngology practice in Vietnam. Primarily, this is explained by a consequence of long- lasting eating habits and local cooking. Most foreign bodies (FB) can be discovered by taking a careful history and a lateral neck radiograph. The unusual complications due to FB ingestion have been described in a few reports [1]. It is worth noting that esophageal perforation (EP) and migration of FB into spaces of the neck are absolutely rare occurrences. These complications if present, can result in significant morbidity, even mortality. Therefore, the migrated foreign body must be retrieved as soon as possible. The incidence of the complications in the medical literature have been reported less than 1% [2], and up to 1500 deaths annually due to the foreign body ingestion in the USA [3]. One of the most significant consequences of the migrated FBs, EP, was a potentially damaging event that may be difficult to diagnose as well as treat properly. Furthermore, in spite of the relatively precise computed tomography location of the FBs in deep space neck, the surgeon must be meticulous to dissect delicate structures of the space. The EP remains to present a therapeutic challenge in spite of decades of the clinical experience as well as advance in surgical technique. There are three approaches for the treatment of EP: conservation, endotherapy, and surgery. The application of these approaches depends on the size and location of the EP, viability of the esophageal mucosa, underlying pathology and degree of the sepsis [4]. The goals of the treatment are treating infection, minimization and prevention of further septic contamination, providing nutritional support and restoration of the continuity of the esophagus [4,5]. Here, we report a case of the complication with migration of fish bone into the posterior cervical space, and an attempt of closure of the EP.
Case Presentation
A 49-year-old female patient presented to the otorhinolaryngology outpatient clinic room of Hue University hospital, Vietnam, with a history of pain immediately after having breakfast with rice and cooked ray for the previous 3 days. She complained of the odynophagia, moderate pain of the left neck. Physical exam showed no crepitation or palpable fluid collections. The lateral neck radiograph showed a FB at the level of the 5th and 6th cervical vertebrae (Figure 1). Rigid esophagoscopy under general anaesthesia was done at the operation room. The FB was not detected in the lumen of esophagus during rigid esophagoscopy. In the meantime, she developed severe odynophagia, dysphagia, poor neck extension and diffuse tenderness, at which time she was referred to the otorhinolaryngology department. The patient had no dyspnea and change of her voice. Then, a computed tomography (CT) scan was performed, and it showed a 20x2 mm FB into posterior cervical space at the level of the C5-C6 vertebrae on the left side. A heterogeneous area with air pockets extending from esophagus to the FB suggested that an abscess and esophageal fistula were formed in the left posterior space of the neck (Figure 2).
Figure 2: The case. A: Diffuse swelling and the position of the FB was marked (arrow) by intraoperative ultrasonography. B,C: The FB is found with associated abscess formation into posterior neck space at the level C5 vertebrae (arrow).
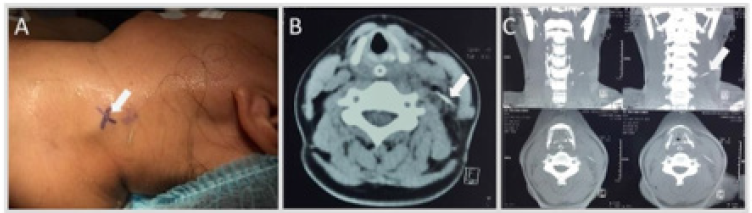
Figure 3: The surgical procedure. A: Intraoperative ultrasound indicated the accurate position of the fish bone related to the sternocleidomastoid (SCM) muscle and surrounding tissue. B: Intraoperative field with the FB removal from posterior neck space. The SCM have been retracted anteriorly. C: The ray tail was removed.
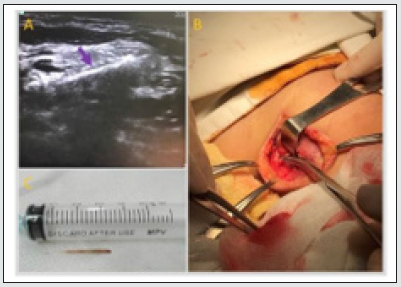
An emergency surgical exploration of the left lateral neck was performed through an apron incision under general anaesthesia. The wound was opened in layers of the lateral neck: skin with subcutaneous tissue, then platysma. After retraction of the sternocleidomastoid (SCM) muscle, a saw-toothed fish bone was detected below the SCM muscle through intraoperative ultrasound guidance (Figure 3A& 3B). The wound was irrigated thoroughly. A vacuum surgical drain was positioned in the wound, and then the wound was closed in layers. A nasogastric tube was placed and secured. Broad-spectrum antibiotics were administered against anaerobic and aerobic germs. To avoid a secondary infection, the drain was removed on the third day after surgery, although purulent drainage still appeared in the vacuum surgical drain. Esophageal perforation was discovered through the wound exploration. Therefore, we left the wound open to perform a wound toilet and then pack it open with damp betadine gauze. The patient was referred to the operating room where she was inserted a feeding gastrostomy tube for long-term enteral feeding 3 days later. The gastrostomy tube was removed 3 weeks later, since the wound was dry, clean and spontaneous closure of the wound.
Discussion
Most common esophageal FBs were fish bones in adult patients. They were mostly swallowed accidentally. Uncommon complications of the esophageal FBs were penetration and migration into the deep neck space. The location of the FBs was considered as a possible risk factor for the complications. The FBs was likely to be impacted or lodged in four areas of natural anatomic narrowing of the esophagus such as the upper esophageal sphincter, the aortic notch, the traversing of the main stem bronchus, and the gastroesophageal junction. In a previous study, 76.19% of cervical EPs were found at the level of the upper esophageal sphincter [6]. This vulnerable position of cervical esophagus was explained by the lack of muscle wrapping Killian’s triangle posteriorly. In addition, the shape of FBs was another factor that might be related to the risk of complications. In our case, the FB was sharp, linear and saw-toothed. A saw-toothed FB was a sharp-ended bone and a sharp transverse scales, like saw, on both sides. The saw-tooth increased the possibility of penetration into the neck space and perforation of the esophagus that it impacted. Furthermore, the saw-toothed shape promoted movement of the FB to deeper neck space, and it also prevented the bone from withdrawing from the mucosa. To push the FB into the stomach, the patient gulped some rice, and this practice can increase the migration of saw-toothed FB extraluminally.
The physician should consider the possibility of EP and migration of the FBs into the neck space. Especially, the patient continues to complain of neck swelling and constant pain, fever after a history of the FB swallow, even if the FB was not found by lateral neck radiograph, endoscope examination, and a conventional physical examination. Upon encountering this case, a CT scan will help to identify the exact location of the FB, its relationship to the important anatomic structures in the neck and plan removal approach. The previous study showed that sensitivity of lateral neck radiograph detection for FB ranges from 27% to 57% [7]. On the other hand, the sensitivity and specificity of CT scan are over 90% and 100%, respectively [8], [9]. We must keep in mind that the position of the neck was not the same during CT scan and surgery because soft-tissue structures of the neck are movable in relation to the cartilaginous and bony structures [10]. Moreover, because of the extension of the neck during surgery, the FB was found lower than what we saw on CT scan.
Therefore, the surgeon has sometimes had a frustrating experience with the surgical exploration of the lateral neck to find the FB as we felt in the current case. Use of intraoperative ultrasonography was another imaging option, which was successfully used to locate the FB in the current case. Based on the clinical situation and severity, treatment of a cervical esophageal perforation can be either nonsurgical or surgical. Nonsurgical methods included broad spectrum antibiotics, cessation of oral intake, total parenteral nutrition, feeding gastrostomy tube, and percutaneous drainage. In a previous study, Hasan et al showed that nonsurgical (conservative) management of the EP had a survival of 84.6% [11]. Their study also revealed that the EPs had advantageous outcomes when they were diagnosed within 6 hours. In another review, successful nonsurgical therapy resulted in fewer complications, lower mortality rate, and shorter hospitalization in comparison with surgical treatment [12]. The management of EPs is still a challenge for clinicians, and it depends on the location and etiology of Eps as well as the customs of the clinicians. Generally, cervical EPs are less severe and easier management than thoracic and abdominal EPs. The indications for the nonsurgical management are small perforations, early diagnosis, cervical or thoracic perforations, nontumoral perforations, and the absence of infective syndrome [4].
Conclusion
Our case highlights the importance of the identification of the esophageal perforation and the migration of an ingested fish bone into the posterior cervical space. The CT scan of the neck without oral contrast is a useful tool to diagnose and locate such foreign bodies preoperatively. Intraoperative ultrasound can be a significant help in finding the foreign body.
Conflicts of Interest
Authors have none to declare
References
- Chung SM, Kim HS, Park EH (2008) Migrating pharyngeal foreign bodies: a series of four cases of saw-toothed fish bones. European Archives of Oto-Rhino-Laryngology 265(9): 1125-1129.
- Lam HCK, Woo JKS, van Hasselt CA (2003) Esophageal Perforation and Neck Abscess from Ingested Foreign Bodies: Treatment and Outcomes 82(10): 786-794.
- Sung SH, Jeon SW, Son HS (2011) Factors predictive of risk for complications in patients with oesophageal foreign bodies. Digestive and Liver Disease 43(8): 632-635.
- Chirica M, Champault A, Dray X (2010) Esophageal perforations. Journal of Visceral Surgery 147(3): e117-e128.
- Bufkin BL, Miller JI, Mansour KA (1996) Esophageal perforation: emphasis on management. The Annals of thoracic surgery 61(5): 1447–1452.
- Jiang J, Yu T, Zhang YF (2012) Treatment of cervical esophageal perforation caused by foreign bodies. Diseases of the Esophagus 25(7): 590-594.
- Evans RM, Ahuja A, Rhys Williams S (1992) The lateral neck radiograph in suspected impacted fish bones — Does it have a role? Clinical Radiology 46(2): 121-123.
- Eliashar R, Dano I, Dangoor E (1999) Computed Tomography Diagnosis of Esophageal Bone Impaction: A Prospective Study 108(7): 708-710.
- Akazawa Y, Watanabe S, Nobukiyo S (2004) The management of possible fishbone ingestion. Auris Nasus Larynx 31(4): 413-416.
- Verma RK, Panda NK (2014) Metallic foreign body migrating into prevertebral muscles: how we did it? Oman medical Journal 29(1): 64-66.
- Hasan S, Jilaihawi ANA, Prakash D (2005) Conservative management of iatrogenic oesophageal perforations — a viable option. European Journal of Cardio-Thoracic Surgery 28(1): 7-10.
- Abbas G, Schuchert MJ, Pettiford BL (2009) Contemporaneous management of esophageal perforation. Surgery 146(4): 749-756.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...





