
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Case Report(ISSN: 2641-1709) 
The Edentulous Atrophic Mandible Fracture: A Case Report Supporting Use of Large Bone Plating Systems and Discussion of the Value of Identifying Patient Treatment Goals Volume 1 - Issue 4
Gary Nishioka1* and James Eyre2
- 1 Willamette Ear Nose and Throat & Facial Plastic Surgery, Oregon, USA
- 2 Willamette Valley Oral & Maxillofacial Surgery Inc, Oregon, USA
Received:January 28, 2019; Published: February 04, 2019
Corresponding author: Gary Nishioka, Willamette Ear Nose and Throat & Facial Plastic Surgery, Oregon, USA
DOI: 10.32474/SJO.2019.01.000118
Abstract
Surgical management of the atrophic edentulous mandible fracture is one of the most challenging types of mandible fractures to treat. This case report reviews some of the challenges involved in management of this category of mandible fracture. Observations and recommendations are made with regards to treatment, and the potential importance of discussing treatment goals with the patient are outlined.
Keywords:Edentulous; Atrophic mandible; Mandible fracture; Bone Plates
Introduction
Increasing longevity in the edentulous population who utilize a (lower) mandibular removable denture, and its adverse effect on the mandible with progressive resorption, will lead to continued or increased numbers of patients with atrophic mandible fractures despite a significant trend in preservation of existing dentition and use of dental implants. Management of the edentulous atrophic mandible is challenging given the volumetric bone loss and its effect on bone healing; loss of dentition which are used in treatment of mandible fractures for placement of maxillomandibular arch bars and fixation of variable duration; position of the inferior alveolar nerve rising to the surface of pseudo-alveolar ridge of the mandible; and to a lesser extent the marginal mandibular branch of the facial nerve with repairs using an external approach. Furthermore, these fractures are relatively rare and therefore surgical experience can be scant in the community setting making management of these complex fractures even more challenging. Because of aging, health issues can become significant factors in selection of treatment options with its impact on patient morbidity such as time under general anesthesia (operating time), wound site(s) morbidity (size) especially with bone grafting, blood loss, and postoperative recovery. A wide variety of treatment options have been employed over the years and are well described in large review articles [1-3]. In general, open reduction internal fixation with bone plating and screws of various sized plating systems appears to be the foundation of management, with or without bone grafting. If added, bone grafting is used as an attempt to facilitate bone healing and increase bone volume, with the latter attempting to prevent further fractures and facilitate restoration of mastication with fixed or removable dental prostheses (with or without dental implants). Bisphosphonates drug therapy has not been used postoperatively to try and facilitate bone healing and increase bone density in the patient’s with edentulous atrophic mandible fractures who underwent fracture repair, likely due to the concern of bisphosphonate related osteonecrosis and development of pathologic mandible fractures [4].
Case Report
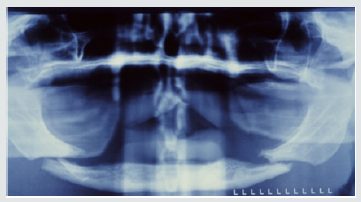
This 79-year old female suffered a fall resulting in bilateral mandibular body fractures, and this was her only significant injury. This patient had a Luhr class III edentulous atrophic mandible, less than or equal to 10 mm in vertical height at the mid-body region of the mandible [1]. The patient was in relatively good health, ASA class 2 with stable hypertension and atherosclerotic cardiovascular disease. The patient had significant pain and difficulty swallowing including liquids. Speaking was difficult because of pain with an unstable mobile anterior mandibular arch. The patient did have upper and lower dentures which were still intact and potentially usable. Bilateral dense hypoesthesia of both inferior alveolar nerves was present, with lower facial bruising and swelling. The mandibular fractures did not lacerate the intraoral gingiva or mucosa but significant ecchymosis and swelling at the fracture sites were seen. No evidence of any airway obstruction was present although there was a tendency for poor support for the tongue structures because of the mobile anterior mandibular arch. Discussion of treatment options were performed with emphasis on open reduction internal fixation with bone plating and screws (Figure 1). As part of this discussion, the patient was asked what their most important outcome parameters were, which included the following; relief of pain, restoration of the ability to take in adequate nutrition with swallowing liquids and very soft foods; and the ability to speak normally. The ability to wear a lower denture again was not an important priority as her denture did not fit being mobile over a flat pseudo-alveolar ridge.
Figure 1: Panorex radiograph demonstrating bilateral mandibular fractures in a patient with a Luhr class III atrophic mandible.
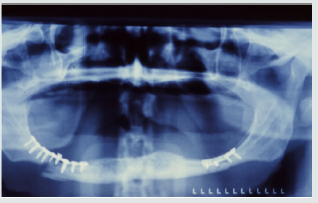
The patient underwent open reduction internal fixation (ORIF) without bone grafting using a 2.0 mm bone plating system through a transoral approach using nasotracheal general anesthesia. Bone plating was performed at each fracture site with immediate mobilization (no attempt at maxillomandibular fixation). Postoperatively the patient was placed on a pureed to very soft mechanical diet. The patient could not wear their dentures because they were painful and ill-fitting. Recovery was uneventful, and the bone plates showed good fracture reduction on panorex radiograph (Figure 2). After several weeks the patient developed pain and swelling at both fracture sites and a follow-up panorex radiograph was performed showing evidence of some additional bone loss involving the right mandibular fracture (Figure 3). The anterior mandibular arch showed mobility on clinical examination confirming failure of the bone plates and screws. The patient was returned to the operating room and underwent ORIF with a 2.4 mm bone plating system with a bone plate placed at each fracture site using an extraoral approach. A ramus to ramus long span reconstruction plate was not used but was an option. This treatment option selected was made to reduce operating time and the size of the surgical wound. The patient tolerated the procedure well and was immediately mobilized as with the first procedure.
Figure 2: Panorex radiograph showing reduction and stabilization of both right and left mandibular fractures using a 2.0 mm bone plating system.
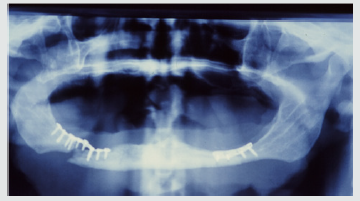
Figure 3: Panorex radiograph showing evidence of some additional bone loss at the right mandibular fracture at the time the patient demonstrated clinical mobility of both right and left bone plates.
Postoperatively, recovery was long and slow, but the patient was able to achieve their desired treatment goals even though she was not able to wear her lower denture because of discomfort due to contact with the bone plate hardware. There was no recommendation or patient desire to have the bone plates and screws removed or further reconstruction with bone grafting with or without dental implants.
Result and Discussion
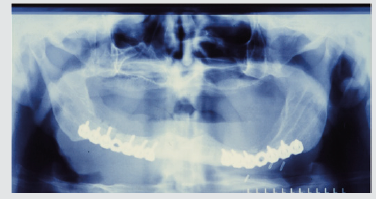
The patient underwent an open reduction internal fixation initially using a small 2.0 mm bone plating system without bone grafting using a transoral approach. This procedure failed with development of mobility at the fracture site resulting in loss of supporting bone for the bone plate and screws. A long span ramus to ramus reconstruction bone plate was not used but was an option that was considered as it would have provided an exoskeleton type support across both fractures as a single unit versus using two bone plates (Figure 4). This approach could theoretically provide continuity of the mandible even if a fibrous non-union occurred. Using two large bone plates with 2.4 mm screws greatly reduced the surgical wound size that would have been required for a full span ramus to ramus reconstruction plate. In addition, the operative time was likely shortened with this approach which did achieve the solid continuity of the mandible. Although using a 2.0 mm bone plating system has been reported with apparent success the experience from this case supports using a large bone plating system instead. A wide variety of treatment options are available to the surgeon1-3 and selection of the treatment option requires analyzing variables such as, is the mandibular fracture unilateral or bilateral, severity of mandibular atrophy, patient health (medical problems), and the patient’s desired goals or surgical outcome. The importance of the identifying the patient’s desired goals/surgical outcomes is deserving of comment.
Figure 4: Postoperative panorex radiograph showing reduction and stabilization of both right and left mandibular fractures using a larger 2.4 mm bone plating system.
The following are desired goals this patient described, and these are further expanded for the reader to consider when selecting a treatment option. The goals or outcomes to consider are separated into primary (more essential) outcomes and secondary, important but not essential for functioning at basal level.
Primary Goals Include
a) Relief of pain.
b) Restoration of ability to take in adequate nutrition.
c) Restoration of intelligible speech.
Secondary Goals Include
a) Achieving the patient’s desired ability to masticate (chew), generally restoring the ability to use dentures or have dental implants placed to support fixed or a removable prosthesis.
b) Desired facial aesthetics as it relates to support of the lower lip/chin region, and vertical facial height.
Trying to meet patient expectations by identifying their desired goals and selecting a treatment option that could achieve these goals is the pathway to success. Should the treatment option not be within the ability or comfort zone of the surgeon practicing in a community setting, transfer to a tertiary facility, such as level 1 trauma center, is an option the surgeon may want to consider.
References
- Novelli G, Sconza C, Ardito, Bozzetti A (2012) Surgical treatment of the atrophic mandibular fractures by locked plates systems: Our experience and a literature review. Craniomaxillofac Trauma Reconstr 5(2): 65-74.
- Emam HA, Ferguson HW, Jatana CA (2017) Management of atrophic mandible fractures: ab updated comprehensive review. Oral Surg 11(1): 1-3.
- Madsen MJ, Haug RH, Christensen BS, Aldridqe E (2009) Management of atrophic mandible fractures. Oral Maxillofac Surg Clin N Am 21(2): 175-183.
- Otto S, Paulke C, Hafner S, Hesse R, LF Reichardt, et al. (2013) Pathologic fractures in bisphosphonate-related osteonecrosis of the jaw - review of the literature and review of our own cases. Craniomaxillofac Trauma Reconstr 6(3): 147-154.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...











