
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Research Article(ISSN: 2641-1709) 
Role of Postoperative Intravenous Administration of Dexamethasone on Outcomes of Tonsillectomy Procedure: As Comparative Prospective Audit Volume 9 - Issue 4
Khalid Mohamed Bofares*
- Professor, Department of otorhinolaryngology, Omar Almoukhtar University, ELbyda, Libya
Received: December 19, 2022; Published: January 09, 2023
Corresponding author: Khalid Mohamed Bofares, Professor, Department of otorhinolaryngology, Omar Almoukhtar University, ELbyda, Libya
DOI: 10.32474/SJO.2023.09.000317
Abstract
Background and aims: Tonsillectomy is considered as the most common surgical procedure in the specialty of otorhinolaryngology. Therefore, there are frequent thoughts regarding this procedure to improve its conditions from different aspects, indications, time of surgery, techniques, safety measures, and postoperative care. One of big issues regarding this procedure is the post-operative sequel and complications namely post-operative pain, hemorrhage, nausea and vomiting, dehydration, metabolic as well as nutritional deficiencies, and air way obstruction. Therefore, this study was conducted prospectively to confirm the effect of intravenous administration of dexamethasone on outcomes of this procedure as compared to the effect of rectal administration of indomethacin as well as oral administration of paracetamol after tonsillectomy in children.
Patients and methods: One-thousand, five-hundred, sixty-four (1564) cases of patients aged from 8 months to 85 years presented at ENT department- ALTAWRA central teaching hospital, and ALTRAHOM private clinic – ELByeda – Libya as well as ALNGAH private clinic –DARNA- Libya, at period from September 2005 to September 2022. The patients were presented as cases of chronic tonsillitis (with or without adenoid enlargement among childhood patients), with different varieties of surgical indications for tonsillectomy. These indications were snoring and apnea attacks, persistent secretory otitis media, frequent attacks of acute suppurative otitis media, failure to thrive among children, repetitive attacks of chest infection, mal-occlusive dental deformity, recurrent attacks of acute tonsillitis (according to Paradise’s criteria), and unilateral enlarged tonsils with high suspicious of neoplastic changes for tonsillectomy-biopsy. The patients were divided into two groups, group-A including seven-hundred, eightytwo patients, and the remaining half of patients was representing the group-B. The patients among group-A were administered with intravenous dexamethasone, while the other group receiving just paracetamol. As prospective analytic study, two groups compared in relation to significant postoperative complications risk, which were in form of post-tonsillectomy pain, bleeding, nausea and vomiting, respiratory distress, dehydration, post-adeno-tonsillectomy negative pressure pulmonary edema, and metabolic as well as nutritional deficiencies. In addition, these groups compared for any significant difference regarding the period of postoperative hospitalization, which can be used as objective indicator to measure the postoperative morbidity rate.
Results: Dexamethasone administration caused significant improvement in pain intensity and thus improving the postoperative oral intake as compared to paracetamol group. From the other view, there was significant reduction in the incidence of posttonsillectomy upper air way obstruction, nausea and vomiting, dehydration, bleeding, and metabolic as well as nutritional deficiencies among group-A as compared to group-B.
Conclusion: Dexamethasone can be considered as potent analgesic drug after tonsillectomy procedure and in same time, it plays significant rule in the improvement of outcomes of this common procedure as compared to the other commonly used nonsteroidal anti-inflammatory drugs.
Keywords: Post tonsillectomy dexamethasone administration; Post-tonsillectomy antinociception; Post-tonsillectomy analgesia; post tonsillectomy complications
Introduction
Tonsillectomy procedure (with or without adenoidectomy) is the most common surgical procedure in the specialty of otorhinolaryngology [1,2]. Post-operative pain is a significant problem that continues to be untreated in the pediatric population. Post-adenotonsillectomy pain can be in the form of sore throat, odynophagia, otalgia or trismus [1-5]. The presence of post- tonsillectomy pain especially in the form of sore throat, or severe odynophagia may restrict swallowing and lead to severe dehydration and weight loss [1-5]. Thus post-tonsillectomy pain can be considered as the most significant contributing factor for other post- tonsillectomy complications namely bleeding, air way obstruction, dehydration, metabolic as well as nutritional deficiencies therefore by proper control of post-operative pain, the other complications incidence will be reduced [1-5]. For this reason there is continuous research for potent anti-nociceptive agent to be used post-operatively after tonsillectomy procedure. Although many studies have been carried out to evaluate the effect of diclofenac sodium as well as paracetamol and indomethacin on post-tonsillectomy pain [1,3,5-7], it was felt at the time of initiating this study that there is a lack of data and information regarding the effectiveness of intravenous administration of dexamethasone after tonsillectomy. The specific aims of the study were
a) To assess the analgesic efficacy of dexamethasone on post-tonsillectomy pain and oral intake.
b) To compare the analgesic efficacy of dexamethasone with that of indomethacin and paracetamol as most common analgesic drugs used after adeno-tonsillectomy.
c) To postulate the effect of intravenous administration of dexamethasone on outcomes of tonsillectomy procedure as compared to indomethacin and paracetamol.
Patients and Methods
One-thousand, five-hundred, sixty-four (1564) cases of patients aged from 8 months to 85 years presented at ENT department- ALTAWRA central teaching hospital, and ALTRAHOM private clinic – ELByeda – Libya as well as ALNGAH private clinic –DARNA- Libya, at period from September 2005 to September 2022. The patients were presented as cases of chronic tonsillitis (with or without ad enoid enlargement among childhood patients), with different varieties of surgical indications for tonsillectomy. These indications were snoring and apnea attacks, persistent secretory otitis media, frequent attacks of acute suppurative otitis media, failure to thrive among children, repetitive attacks of chest infection, mal-occlusive dental deformity, recurrent attacks of acute tonsillitis (according to Paradise’s criteria), and unilateral enlarged tonsils with high suspicious of neoplastic changes for tonsillectomy-biopsy. Patients with renal disease, gastrointestinal disease, chronic pain states or daily intake of NSAID were excluded. Informed consent was obtained from the patients as well as patients’ relatives for participation at the study. All patients were admitted one day prior to surgery after normal routine investigations. The patients were divided into two groups, group-A including seven-hundred, eighty-two patients, and the remaining half of patients was representing the group-B. The patients among group-A were administered with intravenous dexamethasone, while the other group received just paracetamol. In accordance, by simple random sampling, each group contains a variety of ages from selected age spectrum. Group-A patients were administered by intravenous dexamethasone (4mg-8mg\ dose) as three doses first dose was administrated intra-operatively. Group-B patients received oral paracetamol (10-15 mg/kg) in four divided doses first dose after two hours from surgery. Inhalation anesthesia was used and supplemented with intravenous Fentanyl 200- 400mg, and intubation either performed by oral endotracheal or naso-tracheal tube insertion.
Adenoidectomy was carried out by curette, while tonsillectomy by simple dissection method. Homeostasis was secured by Bipolar Electrocautery, ligation or by pack pressure. All patients underwent extubation in the operative room then transferred to the recovery station, vital signs were assessed and after appropriate care in recovery room, the patients were transferred to the in- patient ward. During this period, any instances of crying, vomiting or agitation were recorded. The patients were assessed 6, 12, 18 and 24 hours after surgery to see whether they required pain medication. The pain was assessed subjectively using visual analog scale (VAS) by looking to facial expression of the patient during swallowing process. Time of first oral intake and quantity was recorded; temperature, nausea and vomiting were also recorded. Although there were some cases that attained some degree of improvement in pain after administration of analgesic drug, they were considered as having pain, while those who improved completely were considered as having no pain. As prospective analytic study, two groups compared in relation to significant postoperative complications risk namely post-tonsillectomy pain, bleeding, nausea and vomiting, respiratory distress evidence, dehydration, post-adeno-tonsillectomy negative pressure pulmonary edema, and metabolic as well as nutritional deficiencies. In addition, these groups compared for any significant difference regarding the period of postoperative hospitalization, which can be used as objective indicator to measure the postoperative morbidity rate. Data were presented by using descriptive analysis as means ± standard error of mean (s.e.m) and percentages. Test of significance was measured; using chi-square test and twoway analysis of variance ~.A probability less than 0.05 was considered as significant, the degree of significance was determined by using level of standard deviation test. Student — t — test was used for dependent sample, as well as contingency coefficient was calculated as measurement of association between studied variables.
Results
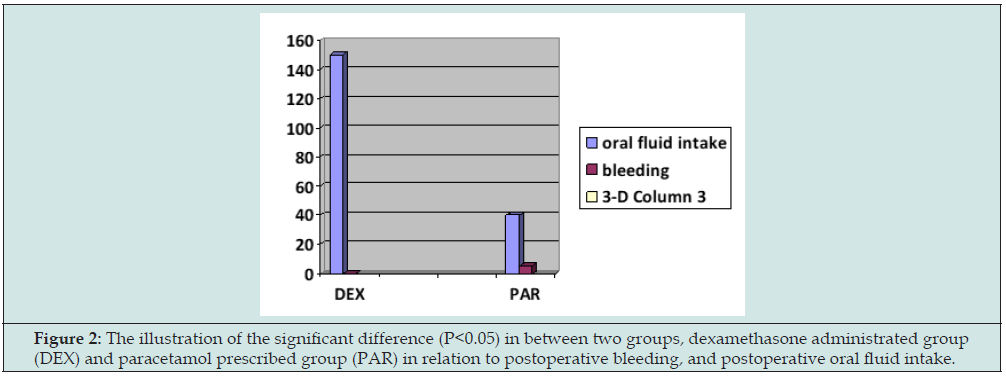
As can be illustrated at Figure 1, the results presented significant reduction in post tonsillectomy throat pain and otalgia after administration of dexamethasone in comparison to paracetamol (P<0.01), Therefore the amount of ingested fluids was increased significantly by administration of dexamethasone (P<0.01) as compared to paracetamol. There was significant reduction in the incidence of post-operative vomiting tendency by administration of dexamethasone as compared to paracetamol (P<0.05) as it is shown at Figure 1. On the other hand, as can be noted at Figure 2, this study showed significant decrease in the risk of post-tonsillectomy bleeding after administration of dexamethasone as compared to paracetamol (P<0.1). Occasionally there was significant difference between the studied groups regarding the incidence of post-tonsillectomy dehydration; the hydration status was significantly improved after administration of dexamethasone as compared to paracetamol (P< 0.01) as it was postulated at Figure 1. In fact there was not any significant difference between two groups regarding the occurrence of post-tonsillectomy airway obstruction (P>0.5) i.e. there was no any post- operative air way obstruction cases recorded by this presented study. By same manner, there was not any significant difference between two groups regarding the appearance of post-tonsillectomy metabolic or nutritional deficiencies (P>0.5). In addition, there was not any significant difference between two groups in relation to post-operative hospitalization time, all patients among two groups were discharged from the hospital after 12 hours maximum from time of the surgery performance (P>0.5).
Figure 1: the illustration of the significant difference (P<0.05) in between two groups, dexamethasone administrated group (DEX) and paracetamol prescribed group (PAR) in relation to postoperative pain intensity, postoperative vomiting tendency, as well as postoperative dehydration incidences.
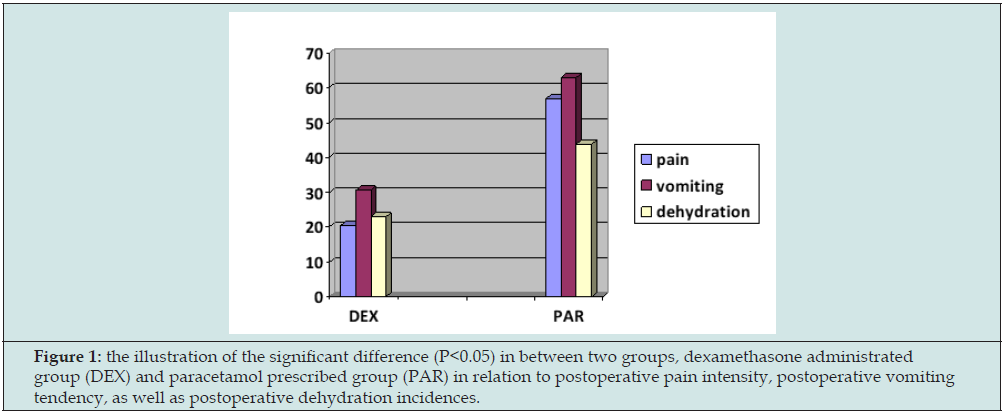
Figure 2: The illustration of the significant difference (P<0.05) in between two groups, dexamethasone administrated group (DEX) and paracetamol prescribed group (PAR) in relation to postoperative bleeding, and postoperative oral fluid intake.
Discussion
Adeno-tonsillectomy and tonsillectomy procedures are considered as the most common surgical procedures in the specialty of (ENT). Post-operative pain is a significant problem that continues to be untreated in the pediatric population, which leads to the inability to tolerate oral intake and unplanned hospitalization [1-5]. Prostaglandins contribute to pain and inflammation after tissue injury and the anti-nociceptive action of Non-Steroidal Anti Inflammatory Drugs is attributed usually to the peripheral inhibition of prostaglandin synthesis [1-7]. It has been demonstrated that the administration of diclofenac sodium decreases postoperative pain results in a lower incidence of nausea and vomiting, and increases oral intake as compared to paracetamol [3,5,7]. In the same study, it has been shown that by the administration of diclofenac sodium still there is risk of post tonsillectomy complications. Whereas among 80 children; there was one child developed reactionary hemorrhage and one child developed secondary hemorrhage, this is most probably due to platelets dysfunction which may be caused by the administration of diclofenac sodium [3,5,7,8].
On the other hand; it was found that indomethacin given (1- 3mg/kg) in three divided doses after tonsillectomy reduces pain, increases liquid intake in the first 24 hours and resulted in earlier discharge from hospital. Although indomethacin was given earlier with less frequency, but still it is showing more potent analgesic effect as com-pared to paracetamol. This can be explained by longer duration of action of indomethacin as compared to paracetamol [1]. In addition, it was found that the intra-operative as well as postoperative intravenous administration of dexamethasone would help in the maintenance of airway as patent as much as possible due to the potent anti-inflammatory action of this agent. In same manner the systemic administration of dexamethasone was approved to relief the post-tonsillectomy throat pain thus, it helps in the recovery of normal swallowing mechanism as soon as possible, and due to platelets aggregation stimulating effect of dexamethasone, its systemic administration was found to reduce the risk of post-tonsillectomy hemorrhage [9-14]. The protocol of dexamethasone administration which applied in this presenting study was 4-8 mg administered intravenously at time of anesthesia induction then followed by 4-8 mg administered intravenously every eight hours postoperatively for first 24 hours and after that the child will continue with oral administration of dexamethasone as 1 mg \ kg \ day for 7-14 days accordingly [9-14].
Although there were multiple factors which usually affect severity of pain and tolerance of the patients to pain intensity, one of them is the age factor. The adult patients can tolerate pain more than children. Another factor is the technique for bleeding control, the use of bipolar electrocautery and ligation technique create more painful situation as compared to pack pressure technique [2,8]. However, the effects of these factors on the results of the study were overcome by random selection of the patients participated in each group. Moreover, each group included all age varieties in the presenting study. In addition, the random distribution of patients in each group was made regarding the technique which was used intra- operatively for control of bleeding. On the other hand, the vomiting tendency can be correlated with the pain intensity, that the pain severity is directly proportionate to the induction of vomiting tendency [4,6,9]. This can be explained by the relationship between the pain and vasovagal attack i.e. the pain is an important inducing factor of vasovagal attack, thus the stimulation of vasovagal attack will induce vomiting [4,6,9]. This may explain the significant reduction of vomiting tendency after administration of dexamethasone as compared to paracetamol.
Conclusion
Dexamethasone can be considered as potent analgesic drug after tonsillectomy procedure and in same time, it plays significant rule in the improvement of outcomes of this common procedure as compared to the other commonly used non-steroidal anti-inflammatory drugs. However, the tonsillectomy is a commonest procedure in ENT specialty that creates the interest of the all levels of ENT surgeons, including juniors as well as seniors, thus continuous research activities are recommended to resolve all the issues and problems, which can be associated with this common procedure.
Ethical Approval
The administrator of ALTAWRA central teaching hospital- ELByeda- Libya approved the research ethically.
References
- Hotta O, Tanaka A, Tani S (2016) The importance of epipharyngeal procedures in internal medicine: now, another breakthrough is expected. Somata-Pharyngeal 29(1): 99-106.
- Hotta O, Nagano T (2018) Considerations on a variety of conditions suggested to be associated with chronic epipharyngitis and epipharyngeal abrasive therapy. Somata-Pharyngeal 31(1): 69-75.
- Ito H (2022) Heart rate variability analysis of autonomic nerve reflex in epipharyngeal abrasive therapy (EAT). The Autonomic Nervous System 59(3): 320-326.
- Uebaba K (2017) Epipharyngeal abrasive therapy and venous hub theory. The 5th Annual Meeting of the Japanese Society for Lesions and Diseases, Tokyo 2017-9-2.
- Uebaba K, Nishikawa M (2017) New Edition of Indian Life Science - Ayurveda. Rural Cultural Association, Tokyo pp. 100-101.
- Uebaba K (2017) Considerations on the Mechanism of Action of Stinging Therapy Part 1: The “Venous Circulatory System Hub Hypothesis” and the “Venous Congestive Pain Hypothesis. Eastern Medicine 33(1): 63-77.
- Shomoto Y (2017) Physical Therapy occupational visual text. Yodosha, Tokyo pp.55-67.
- Torino D (2004) High-voltage pulse current therapy. Progress in Physical Therapy 15(1): 27-40.
- Ito H, Takahashi E, Fujimatu M (2021) Statistical study of the effects of hyperthermia and electrical stimulation therapy on autonomic nervous activity. Eastern Medicine 37(1): 3-25.
- Ito H (2022) Effect of epipharyngeal abrasive therapy on long Covid with chronic epipharyngitis. Scholarly Journal of Otolaryngology 8(5): 860-864.
- Mogitate M (2022) Effectiveness of epipharyngeal abrasive therapy on chronic epipharyngitis and the exhaled nitric oxide levels. Internal medicine Tokyo, Japan.
- Mogitate M (2022) Exhaled nitric oxide levels are associated with the severity of chronic epipharyngitis and decreased via epipharyngeal abrasion. Auris Nasus Larynx 49(6).
- Kimura T (1982) Dialectical interpretation of qi pathology - hypothesis that qi is a bioelectric current. Practica Oto-Rhinol. Laryngologia 75(2): 751-755.
- Lesondak D, Superviso KT (2020) Fascia: its existence and unknown role. Ijido no Nihonsha, Yokosuka
- Ito H (2022) Effects of biotherapy on EEG. Presentation at the 29th Biotherapy conference. Tokyo, Japan pp. 10-13.
- Yamada K (2015) Practice of microcurrent therapy. Nagoya Chubu Nihon Kyoiku Bunka Kai Co.
- Nagao T (1973) Safety measures between hospitals and ME equipment. Medical Electronics and Biomedical Engineering. 11(3): 61-68.
- Cheng N, Van Hoof H, Bockx E (1982) The effects of electric currents on ATP generation, protein synthesis and membrane transport in rat skin. Clinical Orthopaedics and Related Research 171: 264-272.
- Fujitani H (2018) Microcurrent stimulation therapy in sports. Journal of St. Marianna University School of Medicine 45: 265-269.
- Ichikawa K (2009) Trends in electric shock hazards and hazard limits of electric shock. Safety Engineering 48(6): 407-412.
- Moriyama S, Brestoff J R, Flamar A-L (2018) β2-adrenergic receptor- mediated negative regulation of group 2 innate lymphoid cell responses. Science. 359(6379): 1056-1061.
- Kimura K (2019) The influence of acupuncture treatment on peripheral circulation and its mechanism of action-A study from basic research. Autonomic Nervous System 56: 146-149.
- Imai K, Yamano T, Nishi S (2022) Epipharyngeal abrasive therapy (EAT) has potential as a novel method for long COVID treatment. Viruses 14(5): 907.
- Nishi K, Yoshimoto S, Nishi S (2022)epipharyngeal abrasive therapy (EAT) reduces the mRNA expression of major proinflammatory cytokine IL-6 in chronic epipharyngitis. International Journal of Molecular Sciences 23(16): 9205.
- Varga Z, Flammer A J, Steiger P (2020) Endothelial cell infection and endotheliitis in COVID-19. Lancet 395(10234): 1417-1418.
- Kuratsune H (2021) Myalgic encephalomyeritis/chronic fatigue syndrome (ME/CFS)-Recent aspects-Neurotherapy 38: 164-169.
- Inoue Y (2016) Repetitive transcranial magnetic stimulation therapy. Neurotherapy 33(2): 228-233.
- Ogata K, Tobimatu S (2015) Fundamentals and clinical applications of transcranial direct current stimulation (tDCS). Measurement and Control 54(2): 106-113.
- Sabel BA, Zhou W, Huber F (2021) Non-invasive brain microcurrent stimulation therapy of long-COVID-19 reduces vascular dysregulation and improves visual and cognitive impairment. Restorative Neurology and Neuroscience 39(6): 393-408.
- Loaiza L A, Yamaguchi S, Ito M, Ohshima N (2002) Electro-acupuncture stimulation to muscle afferents in anesthetized rats modulates the blood flow to the knee joint through autonomic reflexes and nitric oxide. Autonomic Neuroscience: Basic and Clinical 97(2): 103-109.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




