
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Case Report(ISSN: 2641-1709) 
Radiation-Induced Maxillary Osteosarcoma: A Case Report Volume 4 - Issue 2
Phan Huu Ngoc Minh1* and Hong Ki Hwan2
- 1Department of Otolaryngolory, Hue University of Medicine and Pharmacy, Vietnam
- 2Department of Otolaryngolory HNS, Chonbuk National University Hospital, Korea
Received: March 05, 2020; Published: March 12, 2020
Corresponding author: Phan Huu Ngoc Minh, Department of Otolaryngology, Hue University of Medicine and Pharmacy, Hue University, Vietnam
DOI: 10.32474/SJO.2020.04.000182
Abstract
The incidence of radiation-induced tumors is increasing in the oncology population as a result of increased survival, with improvement in cancer treatment. Exposure to therapeutic doses of radiation has also been shown to be associated with an increased risk of a second cancer, though the precise risk remains unknown. The occurrence of sarcomas in irradiated tissues is an uncommon but well-documented long-term complication of radiotherapy. In the current study, the case of a 55-year-old man presented with maxillary osteosarcoma occurring 22 years post radiation for his maxillary lymphoma.
Abbreviations: OS: Osteosarcoma; RIS: Radiation Induced Sarcomas; CT: Computed Tomography; RT: Radiotherapy; RB: Retinoblastoma Gene
Introduction
Osteosarcoma (OS) is the most common primary bone malignant tumor [1]. Although pathogenesis is unknown, various predisposing factors have been proposed, including pre-existing bone lesions, osteogenesis imperfect, fibrous dysplasia, trauma, genetic factors, virus and previous radiation [2]. Exposure to therapeutic doses of radiation has also been shown to be associated with an increased risk of a second cancer, though the precise risk remains unknown. Whereby, radiation induced sarcomas (RIS) are defined as tumors that develop after a latent period after radiation, within the field of radiation, and have histological confirmation of a sarcoma. Radiation therapy still occupies a more important position in the treatment of non-Hodgkin lymphoma, especially early-stage NHL. The head and neck area are one of the most frequent sites of NHL, the risk of a second head and neck cancer after radiation therapy for NHL remains unclearly. Here, we present a 55-yearold man with osteosarcoma of the maxilla occurring 22 years after radiotherapy for maxillary lymphoma.
Case Report
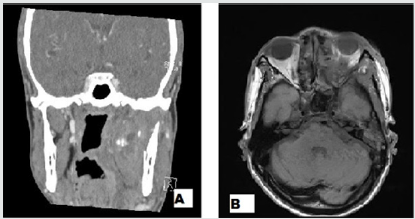
A 55-year-old man presented to our hospital with left facial pain and swelling over the cheek that was increasing in size and advancing towards the eye. Examination in an ENT Department showed an expansible mass in the left maxillary region. The patient had paranesthesia of the left side cheek, left nasal obstruction and anosmia. The overlying skin seems to be normal. The patient underwent a PNS Computed tomography (CT) which demonstrated an 8.2cm sized indeterminate ossifying mass in left maxillary sinus. Additionally, MRI revealed that the bony mass is suggestive of malignancy in left maxillary sinus such as osteosarcoma diagnosed T4bN2c (Figures 1&2). The mass extended into left orbit, nasopharynx, oropharynx, as well as hypopharynx. A diagnosis of osteoblastic osteosarcoma grade 3 (high grade) of the maxilla was confirmed by incisional biopsy at left nasal cavity. According to AJCC staging system, the patient was classified with staged IIB. He was check with PET-CT which revealed no lung metastases. On further questioning, patient was diagnosed to have left maxillary lymphoma 22 years ago. He was previously treated with radiation. He was well since, until he noticed a swelling of the left check and facial pain one year ago. We planned to perform total left maxillectomy followed by concurrent chemoradiotherapy. He denied undertaking an operation and then was lost to follow up.
Figure 1: A Clinical photograph shows a swelling expansile mass in the left maxillary region. B, the nasal endoscopy revealed a left irregular shape and margin mass on left maxillary sinus.

Figure 2: With osteosarcoma on the left maxillary sinus. A, The PSN CT image showed an indeterminate large ossifying mass in left maxillary sinus. B, The PNS MRI image showed a heterogenous enhancing mass which extended into left orbit, nasopharynx, oropharynx and hypopharynx.
Discussion
Progress of therapeutic modalities in recent decades have considerably improved the prognosis of malignant lymphoma. For indolent lymphomas, such as follicular lymphomas, marginal zone cell lymphomas, and small lymphocytic lymphomas are highly radio- responsive, radiotherapy (RT) is often used as the primary treatment alone, and the dose range is normally between 20 and 30 GY [3]. The incidence of radiation-induced tumors is increasing in the oncology population as a result of increased survival, with improvement in cancer treatment [4]. On the other hand, development of therapy-related second cancer as a late complication of treatment has become obvious [5]. In 1948, Cahan et al. [6] established four criteria for the diagnosis of radiationinduced osteosarcoma that are still valid today:
a) The origin of the neoplasm in the radiation field.
b) The nonmalignant nature of the initial bone condition.
c) The histological diagnosis of the neoplasm.
d) A relatively long latency period.
Our patient fulfilled the above-mentioned criteria. Following their criteria, the primary lesion for which RT was administered must be a benign disease. In the early part of the last century, RT was widely used for benign diseases such as tuberculous lymphadenitis, skin diseases, thyroid diseases and spondylitis. However, at present, RT is mainly used to treat malignancies. The limitation of the prior disease treated by RT to a benign disease might thus be impractical. Hence, Sakai et al. suggested that the reliability of the diagnosis of radiation-induced cancer depends on the pathological diagnosis, the organ of origin, the follow-up duration after RT (over 5 years) and on whether the lesion is in the irradiated field [7]. The occurrence of sarcomas in irradiated tissues is an uncommon but well-documented long-term complication of radiotherapy. The average latent period between radiation treatment and development of sarcoma has been reported to be 4 to 30 years with average of 12.5 years [5]. The exact mechanism of radiation induced sarcomas is not clear, these may occur after ortho (low energy) or mega voltage (high energy) radiation, however, with ortho voltage the dosage is lower, and period is longer [5]. In addition to radiation dose, development of RIS is probably influenced by other factors: age of the patient at radiation exposure, association of chemotherapy, and genetic predisposition [8]. It is suggested that the patient who harbor the mutation in tumor suppressor genes like p53 and retinoblastoma gene (Rb) are more prone to develop these tumors [5]. The most common clinical findings of the head and neck radiation-induced sarcoma are pain and swelling with pathological fracture also reported. A soft tissue mass and bone destruction due to new bone formation are the main characteristics on radiography and CT.
The degree of new bone formation on CT is variable. Tumor size and grade are the two most important prognostic factors for soft tissue sarcomas, including those associated with radiation therapy [9]. The prognosis of radiation-induced sarcoma is generally thought to be worse than primary sarcomas, regardless of site. In a review of 78 cases from Mayo Clinic, about 30% of the patients with sarcomas of the craniofacial bones survived 5 years without recurrence [9]. What should be the ideal treatment for post radiation sarcoma is still debatable. High-grade tumors that are larger than 5cm should be treated with primary chemotherapy followed by complete excision of residual disease. All low-grade tumors and high-grade tumors that are 5cm or smaller should be treated with a margin-negative surgical excision, and systemic chemotherapy should be considered when a negative margin is not accomplished [9]. However, as most of osteosarcoma metastasize by hematogenous route, and hence there is a rational for addition of adjuvant chemotherapy [10]. Some authors recommend neoadjuvant chemotherapy before a definitive surgery is undertaken [11].
Conclusion
Radiation-induced sarcoma is a potential late sequelae of radiation therapy. To prevent radiation-induced sarcoma, it is important to have meticulous attention to radiation dosimetry in carefully planned field. Although the condition is rare, the possibility of RIS must be considered in any patient who has received radiation treatment.
Conflict of Interest Disclosures
None of the authors has any conflict of interest, financial or otherwise. This article does not contain any studies with human participants or animals performed by any of the authors.
References
- Amaral MB, Buchholz I, FreireMaia B, Recher P, de Souza PE, et al. (2008) Advanced Osteosarcoma of the Maxilla: A Case Report. Medicina Oral Patologia Oral Y CirugiaBucal13(8):E492-E495.
- Arlen M, Higinbotham NL, Huvos AG,Marcove RC, Miller T(1971) Radiation Induced Sarcoma of Bone. Cancer28(5):1087-1099.
- Yahalom J, Illidge T, Specht L, Hoppe RT, Li YX, et al. (2015) Modern Radiation Therapy for Extranodal Lymphomas: Field and Dose Guidelines from the International Lymphoma Radiation Oncology Group. Int J Radiation Oncol Biol Phys92(1):11-31.
- Coleman CN (1982) Secondary Neoplasms in Parients Treated for Cancer: Etiology and perspective. Radiat Res92(1):188-200.
- Prakash O, Varghese BT, Mathews A, Nayak N, RamchandranK, et al. (2005) Radiation Induced Osteogenic Sarcoma of the Maxilla. World Journal of Surgical Oncology3(49):1-4.
- Cahan WG, Woodard HQ, Higinbotham NL, Steward FW, Coley BL (1998) Sarcoma Arising in Irradiated Bone: Report of Eleven Cases. Cancer82(1): 8-34.
- Pierce DA, Preston DL (2000) Radiation Related Cancer Risks at Low Doses among Atomic Bomb Survivors. Radiat Res154(2):178-186.
- Leclercq C, Penel N, Grosjean J, Fournier C, Vilain MO, et al. (2004) Prognosis of Post Irradiation Soft-Tissue Sarcoma: Case-Control Study. La Revue de Medecine Interne25(12) :886-871.
- Chabchoub I, Gharbi O, Remadi S, Limen S, Trabelsi A,et al. (2009) Post Irradiation Osteosarcoma of the Maxilla :A Case Report and Current Review of Literature. Journal of Oncology.
- Patel SG, Meyers P, Huvors AG, Wolden S, Singh B, et al. (2002) Improved Outcomes in the Patients with Osteogenic Sarcoma of Head and Neck. Cancer95(7):1495-1503.
- Junior AT, de Abreu Alves F, Pinto CA, Carvalho AL, Kowalski LP, et al. (2003) Clinicopathological and Immunohistochemical Analysis of Twenty-Five Head and Neck Osteosarcomas. Oral Oncology39(5):521-530.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




