Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Research Article(ISSN: 2641-1709) 
Prophylactic Eyebrow Fixation Following Temporal Nerve Sacrifice in Cancer Surgery Volume 8 - Issue 1
Javad Rahmati MD1,2, Shahriar Haddady Abianeh MD1,2,Hosseinali Abdolrazaghi MD3 and Hojjat Molaei MD1*
- 1Department of Plastic & Reconstructive Surgery, Tehran University of Medical Sciences, Iran
- 2Department of Plastic & Reconstructive surgery, Razi Hospital, Tehran University of Medical Sciences, Iran
- 3Department of Hand & reconstructive surgery, Sina Hospital, Tehran University of Medical Sciences, Iran
Received: March 07, 2022; Published: March 16, 2022
Corresponding author: Hojjat Molaei, Department of Plastic & Reconstructive Surgery, Tehran University of Medical Sciences, Valie-asr Hospital, IKHC, Iran
DOI: 10.32474/SJO.2022.08.000279
Abstract
Background: BCC and SCC are common facial skin cancers may need motor nerves` sacrifice to have safe margin. This surgery results in non-functional frontalis muscle and brow ptosis. There are several solutions to save facial symmetry. Here, we present our experiences in prophylactic brow fixation.
Patients and methods: 11 patients who had BCC or SCC in lateral brow region and expected to lose their temporal nerve during cancer surgery, entered a descriptive study. During procedure after tumor resection with safe margin including temporal nerve, brow fixation was done by permanent sutures to orbital rim and reconstruction of skin defect was done. Demographic and intraoperative evaluations were recorded and analyzed.
Results: 3 women and 8 men underwent surgery. 4 SCC and 7 BCC were resected. BCCs were mostly infiltrative. The mean size of skin defect after tumor resection was 6.74 cm2 . Reconstruction of skin defects were as 3 local flaps, 4 FTSG, and 4 STSG.
Discussion: Facial skin cancer surgery demands respect to safe margin which may result in sacrifice vital motor nerves of face and distortion and asymmetry. Despite operative and medical solutions to conquer this events, nerve reconstructive surgery outcomes are not optimal, and it seems intraoperative brow fixation to orbital rim can be acceptable alternative in these patients.
Conclusion: Prophylactic brow fixation after temporal branch sacrifice in cancer surgery may save facial symmetry and prevents future brow ptosis.
Keywords: Skin cancer; temporal nerve; prophylactic brow fixation; browpexy
Introduction
Skin cancer management is associated with some basic steps, and it seems the most important item is safe margin during surgery to get rid of tumor and reserve proper prognosis. Safe margins are defined for every tumor according to previous evaluations. Each cancer surgeon is aware of having safe margin in depth and radial aspects and should obey to overcome cancer recurrences. Skin cancers especially BCC and SCC are common in worldwide and surgeon encounter them in different patients- low risk or high risk patients. According to accepted protocols safe margin should be respected in surgeries which may be up to 4-6 mm in BCCs and 10 mm in SCCs [1]. Facial area is important aesthetically and functionally in such operations, as radical resection may distort the appearance or injure facial nerve branches. Lateral peri-orbital area is commonly involved by skin cancers and contain temporal branch of facial nerve. As demonstrated by Farahvash et al. (2013) described the anatomy of facial branches in Persian cavers and defined local points, the temporal branch has its traditional rout in zygomatic and forehead region [2]. Thus, temporal branch sacrifice is inevitable in wide local resections. As a result, inability to elevate frontalis muscle and eyebrow causes asymmetric eyebrow position and depressed eyebrow. On the other hand, resulted skin defect requires skin graft or large flaps to cover, which may interfere with nerve graft. We tried to share our experiences in intraoperative approach to manage upcoming depressed eyebrow, which have done in referral facility of skin cancers.
Patients and Methods
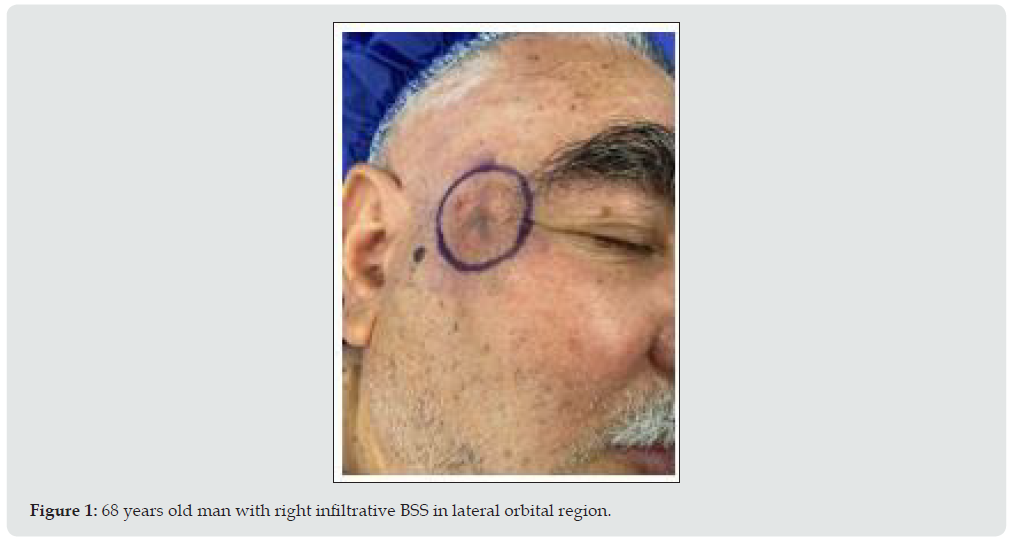
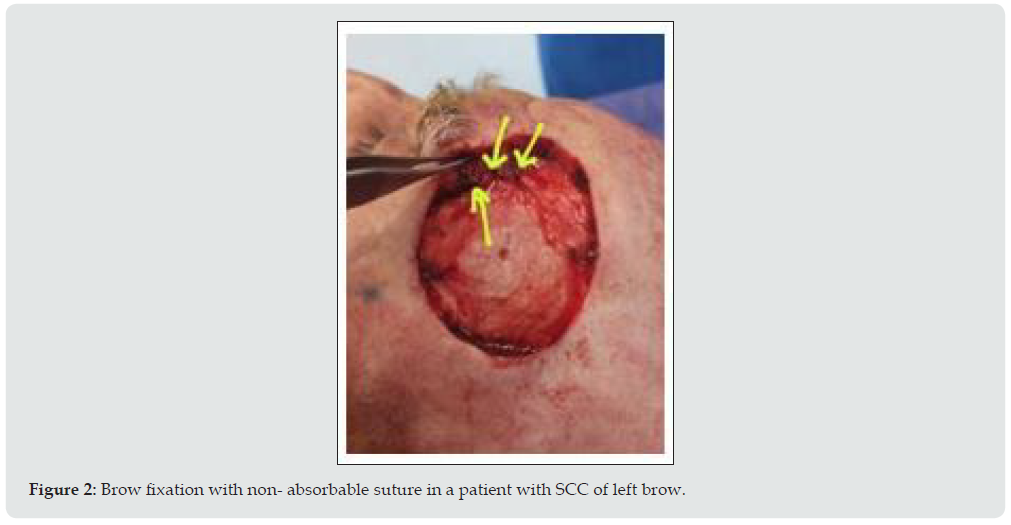
All patients with skin cancer of peri- orbital and zygomatic area who referred for oncoplastic surgery and had wide local tumor excision and temporal nerve branch sacrifice, included in the study (Figure 1). Patients had signed informed consent and had received enough information about plans and ultimate outcome. After tumor resection and confirming safe margin by frozen tissue diagnosis, unilateral browpexy to orbital rim was done by non- absorbable 3-0 sutures (Figure 2). This procedure followed by reconstructive operations to cover skin defect as skin defect- partial thickness or full thickness- or local flaps (Figure 3). All the demographic and operative data gathered and recorded.
Figure 3: Three patients with browpexy and reconstruction by local flaps, full thickness, and partial thickness skin graft respectively.

Results
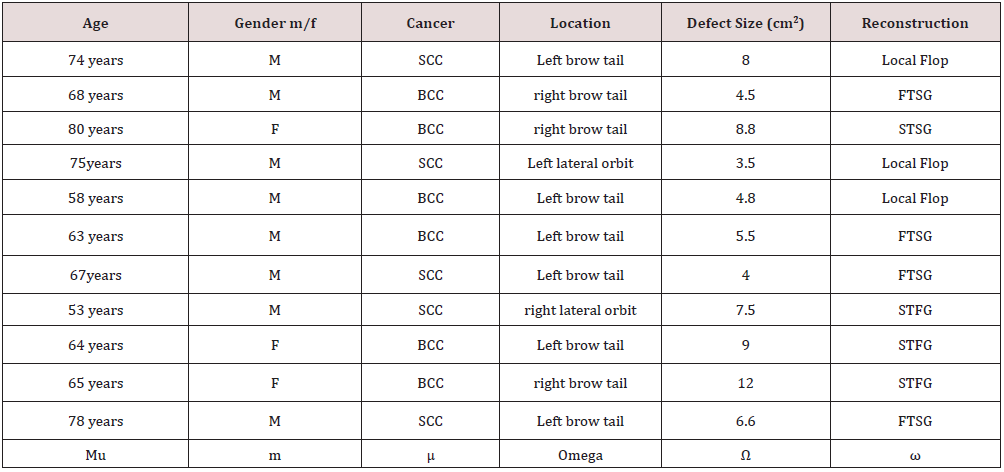
11 patients entered the study completed the questionnaire. 3 patients were women (27%), and mean age was 67.7 years old. Of 11 patients, 4 cases (36.6%) were SCC, and the others were BCC. It is of important that BCCs were infiltrative type mostly- as reported in ultimate tissue diagnosis. 4 tumors (36.6%) were on right side and mostly were on left side. Considering safe margins, large skin defects were resulted which illustrated in Table 1. The mean size of resulted skin defect after cancer surgery was6.74 cm2. Reconstruction of skin defects planned according to general condition of patients and sizer of defect. 3 patients (27%) underwent local flap surgery. 4 patients (36.6%) FTSG and 4 patients (36.6%) STSG received.
SCC: Squamous Cell Cancer; BCC: Basal Cell Cancer; FTSG: Full Thickness Skin Graft; STSG: Split Thickness Skin Graft
Discussion
Transection of the temporal branch of the facial nerve following cancer surgery may be inevitable to enhance long term prognosis which results in paralysis of the frontalis muscle with ptosis of the eyebrow with upper visual field defects [3]. Although, autologous nerve transplantation has been the gold standard in the treatment of facial nerve injury, and substitute conduits can reserve some functional capacity of grafted nerve [4], but previous evaluations demonstrated suboptimal results, especially in distal parts of nerve, there is lower chance of successful recovery of nerve and muscle function. Our cases were tumors in lateral brow area, in which the nerve is in its thinnest situation and coaptation of graft is not as successful as its proximal size. Moreover, most of reconstruction surgeries were skin grafts. It is clear that recovery of nerve graft is not good under skin graft, and surgeons may look for other options to overcome subsequent brow ptosis. Dolen et al (2017) on an experimental study on 28 rabbits we have developed a hypothesis of a chemical agent which prevents excessive calcium transition into the cell, with an assumption of having a role in diminishing mechanically induced nerve injury, therefore improving tissue recovery demonstrated the accelerating effect of nimodipine on neural tissue healing, but despite its attractiveness, it seems ineffective under fibrotic tissues of grafted skin and should be evaluated in clinical trials with more details [5].
Direct brow lifting, which generally targets brow sagging, is reserved for especial circumstances such as male pattern baldness or unusual hairline. It is simply approached by surgeons with acceptable learning curve. Though, ultimate scar is challenging, and patients should be informed. Nowadays, periorbital aesthetic procedures are frequently associated with brow level improvement or correction [6-8]. Brian et al (2011) presented their innovation in brow ptosis correction via upper blepharoplasty incision in selected patients and concluded it as a simple and easily available technique. In this way, they fixed the subcutaneous tissues of brow to marked point of orbital rim by Enditine [9]. In our patients there is not necessary to extra incision in upper lid, as the field was ready after tumor resection and fixation was done. However, Endo tine was not easily available and not safe under skin graft. Skin cancer surgery has its basic rules and sufficient safe margin in surgery is the key point. This can result in sacrifice vital anatomical elements such as motor nerves. Ultimate sequel is permanent brow ptosis and forehead asymmetry. Here, we shared our experiences in prophylactic brow fixation to orbital rim after tumor resection and before skin defect reconstruction, which had acceptable asymmetry even months later.
Conclusion
Prophylactic brow fixation after temporal branch sacrifice in cancer surgery may save facial symmetry and prevents future brow ptosis.
Conflict of Interest
None of the authors has a financial interest in any of the products or drugs mentioned in this article.
References
- Quazi SJ, Aslam N, Saleem H, Rahman J, Khan S (2020) Surgical Margin of Excision in Basal Cell Carcinoma: A Systematic Review of Literature. Cureus 12(7): e9211.
- Farahvash MR, Yaghoobi A, Farahvash B, Farahvash Y, Hadadi Abiyaneh S (2013) The extratemporal facial nerve and its branches: analysis of 42 hemifacial dissections in fresh Persian (Iranian) cadavers. Aesthet Surg J 33(2): 201-208.
- Grabski WJ, Salasche SJ (1985) Management of temporal nerve injuries. J Dermatol Surg Oncol 11(2): 145-151.
- Nakamura Y, Takanari K, Ebisawa K, Kanbe M, Nakamura R, et al. (2020) Repair of temporal branch of the facial nerve with novel polyglycolic acid-collagen tube: a case report of two cases. Nagoya J Med Sci 82(1): 123-128.
- Dölen T, Kaygusuz, Akpolat N, Alpay HC, Kelefl E, et al. (2017) The effect of nimodipine and prednisolone on traumatic facial nerve injury treatment. ENT Updates 7(1): 1-8.
- Booth AJ, Murray A, Tyers AG (2004) The direct brow lift: efficacy, complications, and patient satisfaction. Br J Ophthalmol 88(5): 688-691.
- Genaidy MM, Elshafei AM, Abdallah RM, Shetawy MM (2018) Direct brow lift versus transblepharoplasty browpexy for correction of brow ptosis. J Egypt Ophthalmol Soc 111: 70-75.
- https://entokey.com/direct-browlift-internal-browpexy-browplasty/
- Brian D Cohen, Alyssa J Reiffel, Henry M Spinelli (2011) Browpexy Through the Upper Lid (BUL): A New Technique of Lifting the Brow With a Standard Blepharoplasty Incision, Aesthetic Surgery Journal 31(2): 163-169.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...