Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Case Report(ISSN: 2641-1709) 
Primary Laryngeal Lymphoma and Voice Hoarseness: A Rare Etiology for A Common Clinical Feature Volume 5 - Issue 5
Periklis Giannakis1, Melpomeni Fetta2 and Anatoli Pataridou2*
- 1Medical School, National Kapodistrian University of Athens, Greece
- 2Department of Otolaryngology, Hygeia Hospital, Greece
Received: December 22, 2020 Published: January 07, 2021
Corresponding author: Anatoli Pataridou Department of Otolaryngology, Hygeia Hospital, Greece
DOI: 10.32474/SJO.2021.05.000222
Abstract
Primary Laryngeal Lymphoma is rare both as a hematological and as a laryngeal malignancy. Unlike squamous cell carcinomas, lymphomas require chemo-radiotherapy as 1st-line treatment. A 67-year-old lady presented with voice hoarseness, dyspnea and dysphagia for solids. An otherwise unremarkable physical showed “hot-potato like” voice. Labs were normal, while laryngoscopy and CT revealed an epiglottic mass, which was resected. Biopsy results showed DLBCL. The patient then underwent chemotherapy with complete success. Voice hoarseness has a vast differential diagnosis depending on its character and complementary symptoms. Less than a 100 cases of Primary Laryngeal Lymphoma have been reported in the literature, proving the rarity of this clinical entity.
Keywords:Primary laryngeal lymphoma; voice hoarseness; diffuse large B-cell lymphoma; larynx; lymphoma; epiglottis; dysphagia; dyspnea; “hot-potato like” voice
Abbreviations:CT: Computed Tomography; PET-CT: Positron Emission Tomography- Computed Tomography; NHL: Non-Hodgkin Lymphoma; ECOG: Eastern Cooperative Oncology Group; WBC: White Blood Cells; NEU: Neutrophils; LYM: Lymphocytes; MONO: Monocytes; EOS: Eosinophils; BASO: Basophils; RBC: Red Blood Cells; Hgb: Hemoglobin; Hct: Hematocrit; MCV: Mean Corpuscular Volume; MCH: Mean Corpuscular Hemoglobin; PLT: Platelets; ESR: Erythrocyte Sedimentation Rate; LFTs: Liver Function Tests; AST: Aspartate Transaminase; ALT: Alanine Transaminase; γ-GT: Gamma-glutamyl transferase; Bil: Bilirubin; dBil: Direct bilirubin; iBIl: Indirect bilirubin; Cr: Creatinine; BUN: Blood Urea Nitrogen; Glu: Glucose; Alb: Albumin; TC: Total Cholesterol; TGL: Triglycerides; LDH: Lactate Dehydrogenase; CRP: C reactive protein; DLBCL: Diffuse large B-cell lymphoma; LPR: Laryngopharyngeal Reflux; NK: Natural Killer Cells; R-CHOP: Rituximab, Cyclophosphamide, Andriamycin, Oncovin, Prednisone; HD-MTX: High Dose Methotrexate; CNS: Central nervous system; SCC: Squamous Cell Carcinoma; MALT: Mucosa-Associated Lymphoid Tissue; EBV: Eibstein Barr Virus; BMI: Body Mass Index
Introduction
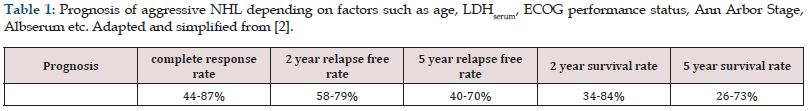
Despite the fact that NHLs are the second most frequently presenting hematologic tumors, they make up for just 1% of all primary laryngeal tumors [1]. However, primary laryngeal NHL should always be considered as a diagnosis, because in contrast with the most common laryngeal malignancies, the treatment of choice is chemo-radiotherapy and not surgical resection. Early detection of lymphomas allows improved patient care and may result in decreased dissemination of the disease process (Table 1). Diagnosis and classification of NHL requires an adequate biopsy specimen and pathologic evaluation because the clinical manifestations, prognosis, and management of lymphomas vary according to the type and the location of the lymphoma. We present a case of an isolated B-cell lymphoma located on the epiglottis, to demonstrate the rarity of its primary location.
Table 1: Prognosis of aggressive NHL depending on factors such as age, LDHserum, ECOG performance status, Ann Arbor Stage, Albserum etc. Adapted and simplified from [2].
Case Report
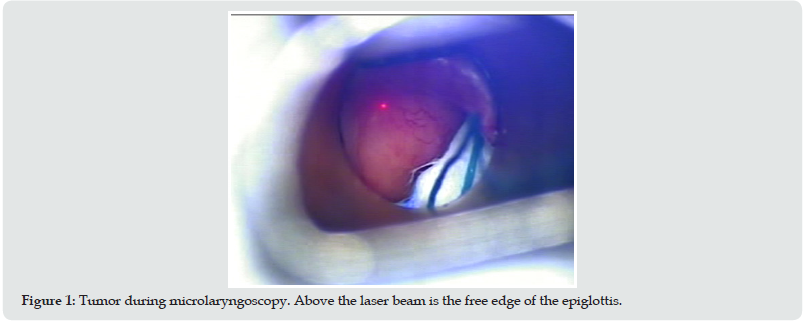
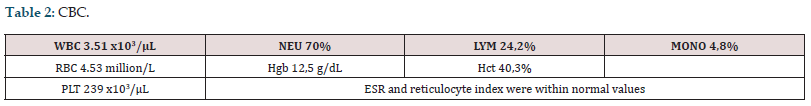
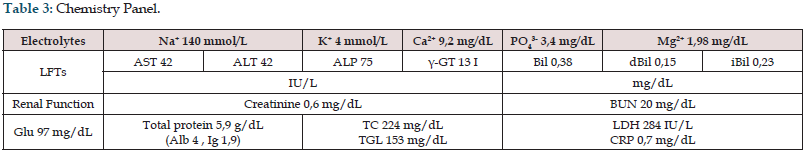
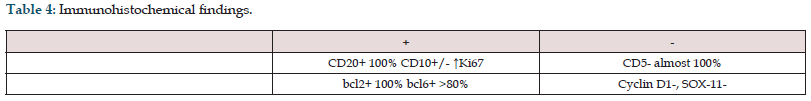
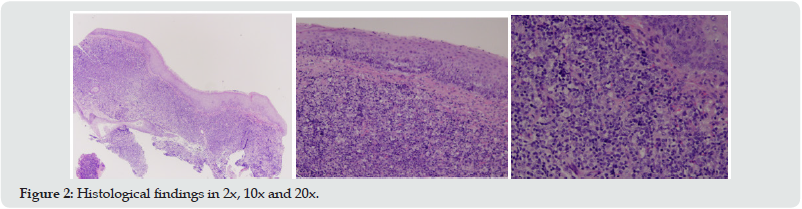
A 67-year-old non-smoking and non-alcohol abusing female patient presented with voice hoarseness, mild dyspnea and dysphagia for solid foods. No history of constitutional or systematic symptoms was reported. The rest of her medical history was free of co-morbidities, past-hospital stays and surgeries. Physical examination showed “hot-potato like” voice. No mass or node was palpable in the head and neck area. She then underwent endoscopic fiberoptic examination that showed a mass on the laryngeal surface of epiglottis. CBC and chemistry panel findings were normal (Tables 2 & 3). CT of the abdomen, thorax and mediastinum showed neither lymphadenopathy nor other abnormal findings, while CT scanning of the neck showed an infiltrative soft tissue mass on the epiglottis. The patient underwent micro laryngoscopy with excision of the mass using laser CO2 (Figure 1). The specimen was sent for pathological evaluation. Macroscopic evaluation revealed pathologic tissue infiltrated by atypical cells, most likely of lymphocytic origin. Microscopic and immunologic analysis of the specimen confirmed the afore-mentioned theory, with findings related to DLBCL (Figure 2 & Table 4). It is worth mentioning that the first biopsy had some limitations due to some sporadic findings, but a second one covered any prior doubt. The patient was brought in by a hematologic clinic for further evaluation and treatment. Lumbar puncture findings were vague, with no sign suggesting a lymphatic hyperplasia or bone marrow infiltration. The patient underwent 6 cycles of R-CHOP, as well as 2 cycles of HD-MTX for CNS prophylaxis. Appropriate supportive medication was given as needed. The patient went through all phases and as a result, complete resolution of the tumor was achieved. Finally, her followup was relapse free. Endoscopy of the larynx was clear, as well as the CT scans and the full body PET-CT scan.
Discussion
Hoarseness is an alteration to the wave properties of the voice and can happen through different mechanisms, functional or organic. Neurological dysfunction due to prior non-thyroid neck surgery has surfaced as the most common reason for vocal dysfunction, followed by unilateral or bilateral vocal cord paralysis [3,4]. Other common etiologies are acute and chronic laryngitis, benign vocal cord lesions, malignancy, LPR and rare systematic causes. Before examining the larynx endoscopically, a careful history and physical are mandatory in order to form a hierarchy in our differential diagnosis. Duration, onset, pattern, known triggering and exacerbation factors, other head, and neck symptoms, smoking and alcohol use, past neck surgery or endotracheal intubation and comorbidities should always be asked thoroughly in history. Head and neck symptoms such as mild dyspnea and solid dysphagia led us to believe that there was a mechanical obstruction blocking the upper airway. For these features to co-exist, anatomical placement of this mass effect should be near the epiglottis. Physical examination for voice hoarseness can happen as we are taking history. “Voice hoarseness” is a broad term that covers disturbances such as actual hoarseness, breathiness, vocal fatigue, “hot-potato like” voice and tremor. These different entities, if examined can suggest the mechanism and the anatomic location of the pathology. “Hot-potato like” voice may sound gurgling, as it indicates salivary pooling, and is a common finding in peritonsillar abscess, epiglottitis and supraglottic masses-tumors. Our endoscopic evaluation matched our prediction, which highlights the importance of following all the steps and accessing the patient’s history and physical. In more difficult cases, when the endoscopic image is not so clear, a great history and physical could be our “navigation system” to observe some anatomical structures with more caution and possibly find lesions that otherwise could go unnoticed.
As far as head and neck is concerned, the malignancies are most of the times (90%) SCCs [5]. Primary NHLs present rarely, with the most common site involved the Waldeyer ring [1], supraglottically, followed by the glottic and subglottic areas [6]. NHL most frequently arises in the GI tract, but the head and neck area, in which cervical nodules are included, is the second most frequent region [1]. Risk factors for NHL are infectious agents (e.g., EBV and Burkitt lymphoma) immunosuppression, autoimmune diseases, and smoking. Alcohol has shown a protective effect, while obesity and generally increased BMI have only been associated with DLBCL [7]. High protein and high fat intake diets have also shown to play a minor role [8].
NHLs CBC is nonspecific, and can range from normal findings to mild anemia, thrombocytopenia and leukopenia or leukocytosis when there is hypersplenism or bone marrow infiltration. LDH and albumin serum levels can sometimes be altered, but these findings are better used for prognosis and have little diagnostic value [2]. Baseline electrolytes and BUN-Cr levels should always be established for successful chemo monitoring. CT scanning was used to exclude other possible tumor sights that would need further evaluation. The next step for us was a diagnostic-therapeutic micro laryngoscopy with laser excision of the tumor and pathologic evaluation of the lesion, which was critical for planning the best possible treatment strategy. In the literature, the cases of lymphoproliferative tumors arising from the larynx reported (including both NHL and immunosuppression-related lymphoproliferative diseases) are less than 100 [9]. NK/T-cell lymphomas that origin in the epiglottic area is only a few [10], and MALT lymphomas occupying the epiglottis are less than 3 cases [11,12]. Treatment for B-cell lymphomas consists of chemotherapy, usually 4-6 cycles of CHOP or R-CHOP.
Conclusion
While primary laryngeal lymphomas may be one of the last possibilities as far as primary laryngeal tumors are concerned, they should never be the least of our concern. They should always, when indicated, be a part of our differential diagnosis, because early recognition and an individualized treatment regimen are key to a really favorable prognosis (Table 1). B-cell lymphomas are more common than T-cell lymphomas and have better prognosis [13]. Early symptoms are not specific, and the diagnosis is often difficult. The take home message from this case highlights the importance of correct medical practice, the pathologic evaluation, and the symptom-treatment driven differential diagnosis. Two or more medical entities that have similar features, but different treatments should always be considered, even if they have a huge difference in likelihood.
Conflict of Interest
History and physical examination: Anatoli Pataridou, Melpomeni Fetta. Laryngoscopy and surgical resection: Anatoli Pataridou. Histopathological evaluation: Thomas Georgiadis Oncologictherapeutic Team: Hematologic Department, Evaggelismos Hospital. Data collection: Periklis Giannakis, Melpomeni Fetta Manuscript: Periklis Giannakis, Melpomeni Fetta. Expert’s opinion: Anatoli Pataridou
Conflict of Interest
We declare no conflict of interest. No funding was received.
References
- Yilmaz M (2012) Primary marginal zone B-cell lymphoma of the larynx. J Craniofac Surg 23(1): 1-2.
- (1993) A predictive model for aggressive non-Hodgkin's lymphoma. N Engl J Med 329(14): 987-994.
- Ramadan HH, Wax MK, Avery S (1998) Outcome and changing cause of unilateral vocal cord paralysis. Otolaryngol Head Neck Surg 118(2): 199-202.
- Rosenthal, L.H., M.S. Benninger, and R.H. Deeb, Vocal fold immobility: a longitudinal analysis of etiology over 20 years. Laryngoscope, 2007. 117(10): p. 1864-70.
- Horny, H.P. and E. Kaiserling, Involvement of the larynx by hemopoietic neoplasms. An investigation of autopsy cases and review of the literature. Pathol Res Pract, 1995. 191(2): p. 130-8.
- Markou, K., et al., Primary laryngeal lymphoma: report of 3 cases and review of the literature. Head Neck, 2010. 32(4): p. 541-9.
- Zhang, Y., et al., Risk Factors of Non-Hodgkin Lymphoma. Expert Opin Med Diagn, 2011. 5(6): p. 539-550.
- Chang, E.T., et al., Nutrient intake and risk of non-Hodgkin's lymphoma. Am J Epidemiol, 2006. 164(12): p. 1222-32.
- King, A.D., et al., Non-Hodgkin lymphoma of the larynx: CT and MR imaging findings. AJNR Am J Neuroradiol, 2004. 25(1): p. 12-5.
- Hirai, T., et al., [A case of epiglottic NK/T cell malignant lymphoma]. Nihon Jibiinkoka Gakkai Kaiho, 2011. 114(10): p. 814-9.
- Azzopardi, C.P., et al., Laryngeal lymphoma: the high and low grades of rare lymphoma involvement sites. Case Rep Med, 2014. 2014: p. 284643.
- Liu, M., et al., Mucosa-associated lymphoid tissue lymphoma of the larynx: a case report and literature review. Medicine (Baltimore), 2015. 94(17): p. e788.
- Uthamalingam, P., et al., Primary laryngeal peripheral T-cell lymphoma--An autopsy report with review of literature. J Cancer Res Ther, 2015. 11(3): p. 647.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...