Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Research Article(ISSN: 2641-1709) 
Prevalence of Abnormal Cervical Vestibular Evoked Myogenic Potential (CVEMP) Responses in Dizzy Patients Following Mild Traumatic Brain Injury Volume 6 - Issue 5
Dr. Eytan A David MD, FRCSC*, Kira Shalinsky BSc
- Department of Surgery, University of British Columbia, Canada
Received:June 12, 2021; Published:June 22, 2021
Corresponding author: Eytan A David, Department of Surgery, University of British Columbia, Canada
DOI: 10.32474/SJO.2021.06.000249
Abstract
Objective: We sought to assess the feasibility of cervical vestibular evoked myogenic potential (cVEMP) as a diagnostic tool for patients experiencing dizziness after mild traumatic brain injury (mTBI) in tertiary neurotology clinic. We used cVEMP to estimate the prevalence of saccular dysfunction after mTBI.
Design: This was a cross-sectional study of patients referred to a tertiary neurotology clinic for dizziness after mTBI. These patients were given a standard neurotology clinical examination and vestibular assessment in addition to a cVEMP test.
Results: 20 of 63 (31.7%) patients had an abnormal cVEMP response. 75% of these subjects showed no deficiency by clinical exam or VNG and 50% registered a deficiency by pure tone audiometry (PTA).
Conclusions: We found that abnormal cVEMP responses were common in dizzy patients post-mTBI and many had normal results in standard neurotological/vestibular tests. cVEMP may help identify those with vestibular dysfunction associated with saccular injury after mTBI.
Keywords: Vestibular evoked myogenic potential; TBI; cVEMP, saccule
Abbreviations: TBI: Traumatic Brain Injury; VEMP: Vestibular Evoked Myogenic Potential; SCM: Sternocleidomastoid; PTA: Pure Tone Audiometry; IAD: Interaural Amplitude Difference; PPPD: Persistent Postural Positional Dizziness
Introduction
Traumatic brain injury (TBI) has an incidence of over 2 million annually in the United States [1]. Most cases are mild (mTBI) and may be associated with symptoms such as headaches, fatigue, cognitive problems, depression, irritability, sleep disturbances, anxiety, heightened sensitivity to noise, visual disturbances, and imbalance/disequilibrium. Imbalance, or dizziness, is a common sequela of mTBI affecting approximately 2/3 of post-mTBI patients [2]. Following mTBI, patients with dizziness have poorer quality of life and are less likely to return to work than those without vestibular dysfunction [2]. Vestibular symptoms often resolve spontaneously over weeks or months, but symptoms are persistent in approximately 15% of cases [3]. Dizziness can result from injury to the central vestibular system in the brain [4,5], to the vestibular sensing organs of the inner ear, or to the vestibular nerves [6]. The vestibular sensing organs comprise the semicircular canals and the otolithic organs, the saccule and the utricle. The former sense angular acceleration, while the latter sense linear acceleration. Otolith defects tends to cause postural unsteadiness, a feeling that sufferers are about to fall, whereas semicircular canal dysfunction often causes vertigo, which is characterized by an illusion of motion [7]. Loss of function of any one vestibular sense organ can cause debilitating symptoms. Patients presenting with vestibular symptoms have commonly been assessed only for horizontal vestibular function using rotational or caloric tests. However, vestibular balance relies on the integration of signals from the otoliths and semicircular canals [7].
Saccular dysfunction is not frequently assessed in patients presenting with dizziness after mTBI. In many patients, no defect in the peripheral vestibular system is identified that explains the symptoms they are experiencing [8]. Vestibular evoked myogenic potential (VEMP) tests were first described in the early 1990s [9]. VEMP testing is a non-invasive test that uses air- or boneconducted sound to evoke a short latency muscle potential. This sound stimulus is thought to specifically stimulate the otoliths.
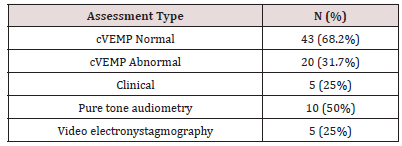
Cervical VEMP (cVEMP) measures an involuntary contraction of the sternocleidomastoid (SCM) in response to this stimulus, while ocular (oVEMP) measures an ocular reflex. Studies in animals and humans have linked VEMP responses to the utricle, in the case of oVEMP, and the saccule in the case of cVEMP. Dysfunction of the saccule, or of the inferior vestibular nerve, which mediates this signal, may result in abnormal latency or amplitude of the myogenic potential of the SCM muscle [7]. Thus, the cVEMP test has enabled detection of injury to the otolithic organs independent of the function of the semicircular canals, which may be intact in some patients with vestibular dysfunction. Indeed, otolith dysfunction as measured by VEMP has been found, in some studies, to be more common than semicircular canal dysfunction [10,11]. However, the cVEMP test has not been widely adopted and the prevalence of saccular deficiency in patients experiencing dizziness after mTBI is not well established. While dizziness has been reported after mTBI in a variety of contexts, it is unclear how often the saccule/inferior vestibular nerve axis is involved. In this study, we investigate the prevalence of abnormal saccular vestibular function in patients reporting dizziness after mTBI using cVEMP (Table 1).
cVEMP: Cervical Vestibular Evoked Myogenic Potential.
Materials and Methods
We recruited patients between the ages of 21 and 70 referred to our tertiary neurotology clinic due to the primary complaint of imbalance and with a mTBI within the past two years. Patients with a prior history of head injury, ear surgery, and prior dizziness or acoustic trauma were excluded as were patients with any conductive hearing loss. Patients provided informed consent and the study was performed in accordance with the Declaration of Helsinki. All participants underwent pure tone audiometry (PTA) testing, comprising tympanometry, speech audiometry, testing of the stapedial reflexes, and video electronystagmography (VNG). Participants underwent a standard neurotological examination including cranial nerve testing, cerebellar testing, and specialized clinical vestibular tests (head impulse testing, post-head shake nystagmus test, Dix- Hallpike test, Unter berger step test, and dynamic visual acuity test). The cVEMP assessment was performed during a ninety-minute session to test the functional integrity of the vestibular system. Before placement of the electrodes, the skin was cleaned and abraded. Electrodes were placed on the middle third of the SCM muscle. EMG scaling was used to ensure consistent results and control differences in background tonic EMG activity between sides.
Electrode impedances were maintained below 3Ω. Patients inserted ER3A-insert earphone (Etymotic Research, Elk Grove Village, IL, USA) into the contralateral ear of the contracted SCM muscle. Air conducted alternating 500Hz tone bursts were presented initially at 95 dB nHL while the patient was placed in supine position with their head elevated either toward the shoulder or at center. Response threshold was determined using a down 10, up 5 dB step procedure using one ear. A minimum of two VEMP responses from 150 stimuli were averaged within a 20-80 msec time window. A minimum wave reproducibility of 75% was required to determine whether a VEMP response was present or absent. The following parameters were measured as dependent variables: absolute and interaural latency differences for N1 and P1; response rate for each position and electrode positioning; absolute amplitudes for P1 and N1 and the interaural amplitude difference (IAD) ratio (the IAD ratio was calculated by dividing the inter-ear difference of p1-n1 intermixture by the sum of the p1-n1 interamplitude of both ears).
Results
Sixty-three patients who presented to the clinic with a previous mTBI and symptoms of dizziness and imbalance were enrolled in this study. 20 of 63 (31.7%) were found to have abnormal cVEMP responses. Among the 20 subjects with abnormal cVEMP findings, 5 also had at least one abnormal finding during the clinical neurotological exam. The most common clinical finding in these patients was a greater than 45-degree deviation during Unterberger step testing. 10 patients had an abnormal positive finding during audiometric (PTA) testing, mcharacterized by a mid-frequency moderate sensorineural asymmetric notched pattern. Five patients were found to have a unilateral vestibular weakness on bithermal caloric testing during the VNG test battery (Table 1).
Discussion
There have been few studies of vestibular function after TBI that assess cVEMP response. The prevalence of abnormal cVEMP responses have ranged from 18.5% to 50% after head trauma [10-12]. Consistent with these studies, 31.7% of the subjects in this study displayed abnormal cVEMP responses. Commonly used investigations for patients presenting with imbalance specifically, caloric testing – may not identify defects to the otolithic vestibular organs. Thus, in the absence of a specific test, patients with impairment of these organs may be given a diagnosis of persistent postural positional dizziness (PPPD), which offers no information about the etiology of their vestibular symptoms. Furthermore, some patients that have a vestibular defect identified clinically or on caloric testing, such as a unilateral vestibular weakness or semicircular canal dysfunction, may also have undiagnosed otolithic impairment, which may complicate their management or recovery. Indeed, in one study, 15 of 63 patients assessed by VEMP after blunt trauma to the head, neck, and cranio cervical junction were found to have an otolith disorder in addition to another vestibular abnormality [11]. Patients with otolith disorders were also found to have poorer resolution of their vestibular symptoms, though each of these patients had at least one other vestibular disorder in conjunction. Of the 20 patients in our study that had abnormal cVEMP responses, 75% had normal clinical findings and 75% did not demonstrate any dysfunction by VNG.
50% had no abnormal audiometric findings. Our results suggest that approximately 1/3 of patients reporting imbalance following mTBI have saccular dysfunction and that, further, most of these patient would have had no positive finding by conventional clinical assessment or VNG. This suggests that as many as 50% of patients presenting with imbalance that show no impairment in horizontal or rotational vestibular function may have undiagnosed saccular dysfunction that could be identified by cVEMP. This study lends support to the emerging use of cVEMP for assessment of the complex dizzy patient, particularly after mTBI. However, a recent systematic review pointed to insufficient evidence supporting the utility of cVEMP for assessment of vestibular symptoms, other than for SCDS [13]. While further study is needed to validate cVEMP as a robust measure of saccular function, this non-invasive test may identify patients with imbalance following mTBI and indicate an etiology for their symptoms that may be missed by conventional investigations. Validation of cVEMP for assessment of saccular function also present the opportunity to determine whether the presence or absence of saccular dysfunction is associated with severity or duration of vestibular symptoms, which is an important topic of future research.
References
- Taylor CA, Bell JM, Breiding MJ (2002) Traumatic Brain Injury-Related Emergency Department Visits, Hospitalizations, and Deaths - United States, 2007 and 2013. Morbidity Mortal Wkly Rep Surveillance Summ Wash DC, USA 66: 1-16.
- Chamelian L, Feinstein A (2004) Outcome after mild to moderate traumatic brain injury: The role of dizziness. Arch Phys Med Rehab 85: 1662-1666.
- Alexander MP (1995) Mild traumatic brain injury: Pathophysiology, natural history, and clinical management. Neurology 45: 1253-1260.
- Gattu R, Akin FW, Cacace AT (2016) Vestibular, balance, microvascular and white matter neuroimaging characteristics of blast injuries and mild traumatic brain injuries: Four case reports. Brain Injury 30: 1501-1514.
- Alhilali LM, Yaeger K, Collins M (2014) Detection of Central White Matter Injury Underlying Vestibulopathy after Mild Traumatic Brain Injury. Radiology 272: 224-232.
- Akin FW, Murnane OD, Hall CD (2017) Vestibular consequences of mild traumatic brain injury and blast exposure: a review. Brain Injury 31: 1188-1194.
- Curthoys I, Manzari L (2013) Otolithic Disease: Clinical Features and the Role of Vestibular Evoked Myogenic Potentials. Semin Neurol 33: 231-237.
- Fife T, Giza C (2013) Posttraumatic Vertigo and Dizziness. Semin Neurol 33: 238-243.
- Colebatch JG, Halmagyi GM (1992) Vestibular evoked potentials in human neck muscles before and after unilateral vestibular deafferentation. Neurology 42: 1635-1636.
- Lee JD, Park MK, Lee BD (2011) Otolith function in patients with head trauma. Eur Arch Oto-rhinol 268: 1427-1430.
- Ernst A, Basta D, Seidl RO (2005) Management of Posttraumatic Vertigo. Otolaryngology Head Neck Surg 132: 554-558.
- Chen G, Zhao X, Yu G (2019) Otolith dysfunction in recurrent benign paroxysmal positional vertigo after mild traumatic brain injury. Acta Oto-laryngol 139: 1-4.
- Fife TD, Colebatch JG, Kerber KA (2017) Practice guideline: Cervical and ocular vestibular evoked myogenic potential testing Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology 89: 2288-2296.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...