Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Research Article(ISSN: 2641-1709) 
Predictive Value of Middle Ear Risk Index Score in the Outcome of Tympan mastoidectomy and Tympanoplasty Volume 8 - Issue 3
Abhinav Agarwal1, JC Passey2, Vikas Malhotra2, Vikas Kumar1* and Mansi Sharma3
- 1MS, Senior Resident, Department of Otorhinolaryngology, Lok Nayak Hospital and Maulana Azad Medical College, India
- 2MS, Director Professor, Department of Otorhinolaryngology, Lok Nayak Hospital and Maulana Azad Medical College, India
- 3Junior Resident, Department of Otorhinolaryngology, Lok Nayak Hospital and Maulana Azad Medical College, India
Received: June 08, 2022; Published: June 21, 2022
Corresponding author: Vikas Kumar, Senior Resident, Department of Otorhinolaryngology, Lok Nayak Hospital and Maulana Azad Institute of Medical Sciences, India
DOI: 10.32474/SJO.2022.08.000289
Abstract
Background and Objectives: Chronic Otitis Media (COM) is an otological challenge especially prevalent in developing countries like India for which tympanoplasty with or without mastoidectomy is the treatment of choice. In this study we aim to assess the predictive value of middle ear risk index (MERI) score in the outcome of tympanoplasty.
Subjects and Methods: 50 patients who underwent surgery in Lok Nayak hospital for chronic suppurative otitis media were given preoperative meri score and were followed and results were assessed according to meri score.
Results: There is a statistical significance with respect to graft uptake and hearing gain according to meri score. As the meri score increased chances of graft uptake decreased and mean hearing gain also decreased with increasing meri score.
Conclusion: All patients undergoing surgery for com should be assessed preoperative for meri score so that appropriate counselling and prognostication can be done about the chances of success of surgery.
Keywords: Tympanoplasty; MERI score; chronic otitis media
Introduction
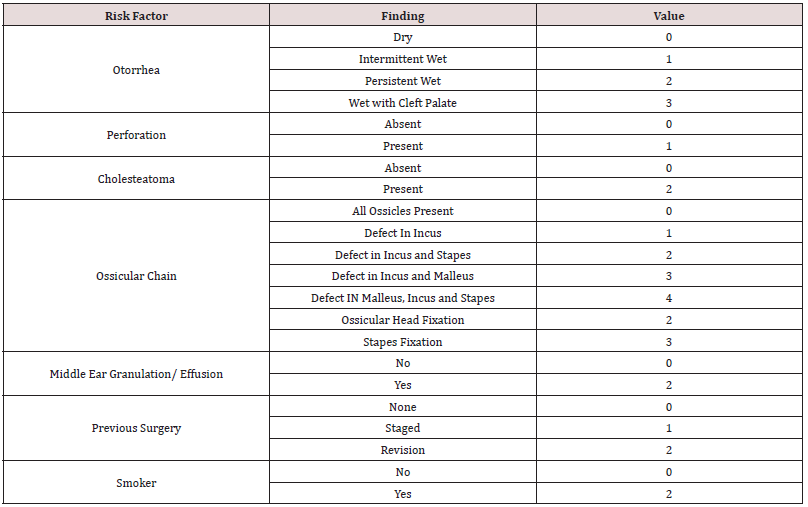
Tympanoplasty is a very common surgery that is being performed by Ear Nose Throat (ENT) surgeons worldwide. There are different techniques and grafting materials that are being used by surgeons. The outcome of surgery also depends on multiple patient and disease factors like the severity of the disease, its extent and various other factors. Multiple studies have been done to assess the disease preoperatively and guide the patient accordingly about the prognosis and outcome of the surgery. Bellucci [1] performed one such study in which he developed a grading system according to symptoms like ear discharge, eustachian tube dysfunction, nasal allergy and tried to improve the risk factors before the surgery to improve the outcome of the surgery. For ossiculoplasty Austin [2,3] proposed a system, comprising of four anatomical situations in 1971 which was modified by Kartush [4] in 1994 after which three more categories were added. The Middle Ear Risk Index (MERI) was given by Kartush in 19944. It is a combination of Austin- Kartush classification of ossicular defects, the Belluci classification of otorrhea and includes the presence of tympanic membrane perforation, middle ear granulations and cholesteatoma. It generates a numerical score that corresponds to the severity of the disease and helps in predicting the successful outcome after surgery. “Meri score is calculated as shown in Table 1”. Based on MERI score the patients are classified as: Mild disease category for score 1-3. Moderate disease category for score 4–6. Severe disease category for score – more than 6.
This helps in guiding case selection for the surgery, counselling of patients pre-operatively and for research purposes too. It helps to decide intraoperatively whether a canal wall up or canal wall down mastoidectomy needs to be done and if ossicular reconstruction should be done primarily or as a second stage surgery. The original MERI had scoring from 0 to 12 but was later modified in 2001 to include smoking as a risk factor and the weightage of granulation and cholesteatoma was increased thus taking a maximum score upto 16.5.
Tympanoplasty and tympanomastoidectomy surgeries are being performed in good numbers and with the increasing awareness of patients, it is imperative to prognosticate the patient according to the disease severity and possible outcome of surgery to avoid any unrealistic expectations and possible medicolegal implications. The present study was conducted to assess the predictive value of MERI score in the outcome of tympanoplasty among Chronic Otitis Media patients [5].
Materials and Methods
After the approval of Institutional Review Board, this was a comparative study done at the ENT department of Maulana Azad Medical College and associated Lok Nayak Hospital, Delhi. All patients of 18 to 60 years of age with COM who attended ENT OPD of the hospital and were planned for tympanoplasty were included in the study. Patients with systemic diseases making them unfit for surgery were excluded from the study.
The patient’s elaborate history was taken which included the demographic details, nature of ear discharge, the period of dryness, hearing loss, any previous ear surgery, history of tobacco smoking, long-term use of ototoxic drugs and any other medical illness. Then examination with otoscope was done to assess the tympanic membrane if intact or perforated, any granulation tissue and for the presence of cholesteatoma. Tuning fork tests were done to assess the type of hearing loss. Patients with conductive hearing loss alone were taken for the study. Those with sensorineural and mixed hearing loss were excluded from the study.
Pure tone audiometry was done to assess the type and degree of hearing loss. Hughson and Westlake method modified by Carhart and Jerger was used to calculate the hearing loss. The mean air-bone gap was measured from the air and bone conduction thresholds at 0.5 kHz, 1 kHz, 2 kHz, and 3 kHz. High resolution computed tomography (CT) scan of the temporal bone was obtained for the squamosal type of COM cases to assess the extent of disease and ossicular status. Routine blood investigations like haemogram and serum electrolytes were done before the surgery. The MERI score was calculated for each patient and then they were stratified into mild (0-3), moderate (4-6) and severe (>6) category.
Procedure
According to the examination and CT temporal scan findings, the type of tympanoplasty and tympanomastoidectomy to be done was planned but could be modified according to the extent of the disease and the ossicular status intraoperatively. For graft temporalis fascia autograft was used in all the patients. Electrical drill and burr were used to drill the mastoid cortex and all the cholesteatoma, granulation tissue, was cleared from the middle ear. Ossiculoplasty was done wherever required and eroded ossicles were refashioned or conchal cartilage was used. The temporalis fascia graft was placed by underlay technique in all procedures. Oral antibiotics and analgesics were given in the post operative period and continued for 7 days, and patients were discharged on the next day after surgery after assessing the suture line and with mastoid dressing. Patients were reviewed every week for 1 month and then once a month for next 3 months and then patients were called 6 monthly. The outcome of surgery was based on two factors:
a) Graft status
b) Pure tone audiometry
Graft status was assessed using otoscopic examination
a. Successful – healed graft
b. Graft failure or perforation within graft
Pure tone audiometry was done at the end of three months post operatively. Hearing benefit was calculated based on the difference between preoperative and postoperative air bone gaps.
Results
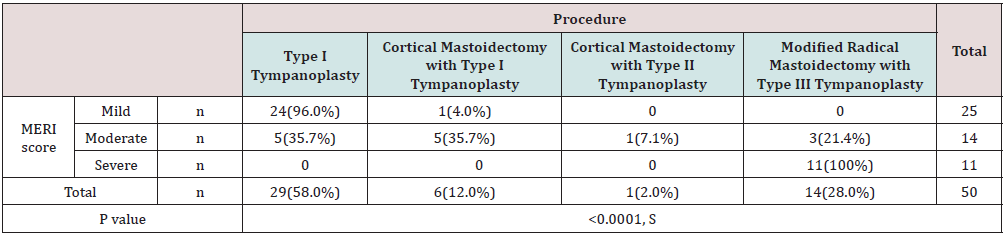
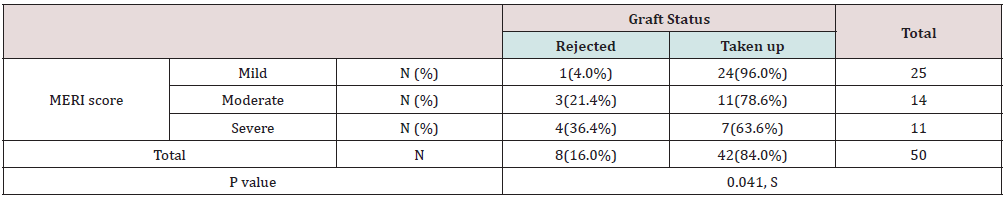
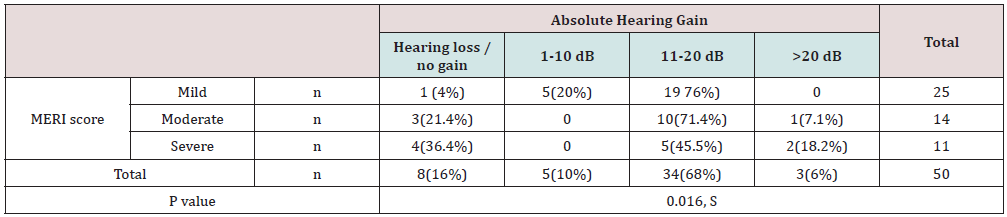
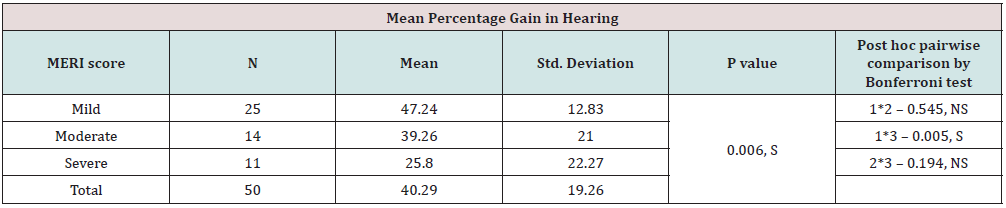
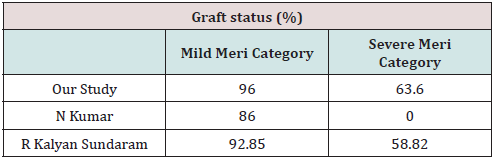
In our study the most common age group for com was 21-30 years of age comprising 42 percent of the total cases. 72 percent of the cases had mucosal type of com and the remaining 28 percent were squamosal type of com. 70 percent of cases required type 1 tympanoplasty, 2percent required type 2 tympanoplasty and the remaining 28 percent required type 3 tympanoplasty. As the meri score increased from mild to severe procedure required changed from type 1 tympanoplasty to type 3 with p value being very significant. “The data to show the type of surgery required according to meri score has been depicted in Table 2”. With increasing meri score the success rate of graft uptake decreased from 96 percent to 63.6 percent,“ as shown in Table 3”. In the Tables 4 & 5 we can see that with increasing meri score hearing gain is compromised both in absolute and mean percentage gain with p value being significant. “Table 4 depicts the absolute hearing gain according to meri score”. “Table 5 shows the mean percentage gain in hearing according to meri score”
Discussion
COM remains prevalent and troublesome disease for a significant population. The mainstay of treatment is surgery for most of the cases. Even after improvements in surgical technique, improved microscopes and sterility we still do not achieve 100 percent positive outcome after surgery. There are multiple factors which hinders the achievement of 100 percent mark, which lead to development of MERI score which combines multiple factors affecting the outcome of surgery and helps in guiding both the patient and doctor about the chances of success of surgery and what to expect after the surgery. So, in this study, we discuss if MERI scoring is an efficient and effective tool for prognosticating patients of CSOM.
Meri Category
According to the preoperative findings, patients were placed in mild, moderate or severe category of MERI score. In our study, we got 50 percent of the cases in mild category, 28 percent in moderate category and the remaining 22 percent in the severe category of MERI. Most of the patients of mucosal type of COM lied in the mild MERI category and most of the patients of squamosal type of COM lied in moderate or severe category of MERI. The distribution of the types of intervention required was found to be significantly different among patients with different categories of MERI score. Among patients with mild MERI score, majority underwent Type 1 tympanoplasty. While among patients with severe MERI score, all underwent Modified Radical Mastoidectomy with tympanoplasty. Similar results were obtained in the study conducted by Mahmood Shishegar et al. [6] where they concluded that with increasing MERI score, there was a statistically significant higher chance of the need for mastoidectomy and as the MERI score decreases, the need for mastoidectomy decreases and only tympanoplasty may be required.
Graft status
After the surgery, patients were followed up for 3 months. Graft status was considered successful when on otoscopic examination the graft was completely taken up and there was no residual or recurrent perforation during that time period. Out of the total 50 cases that were operated, there was an overall 84 percent graft uptake rate. The graft status was found to be significantly different among patients with different categories of MERI score. Among patients with mild MERI score, among majority, the graft was successfully taken up, while, among patients with severe MERI score, the rejection rate was significantly high as compared to that among subjects with mild MERI score. These results are similar to the study conducted by Nishant Kumar et al. [7] in which there was 86 percent graft uptake rate in mild MERI score category and there were only 2 cases of severe category of MERI score and in both of them graft was rejected. Another study conducted by Rameshbabu Kalyansundaram et al. [8] also got similar results in which 92.85 percent of the cases belonging to mild category of MERI score had a successful graft uptake and the success rate in severe category of MERI score was 58.82 percent. “Table 6 shows the comparison of graft status from our study and with other previous studies by N Kumar and R Kalyansundaram.”
Hearing Gain
The other factor that we studied was the audiological gain after the surgery. We assessed the amount of audiological gain as compared to the preoperative level and the variation in the audiological gain if it exists in the different comparison groups that are the mild, moderate and severe category of MERI score. Hearing gain was calculated by PTA done preoperatively and at three months post operatively. The mean air-bone gap was measured from the air and bone conduction thresholds at 0.5 kHz, 1 kHz, 2 kHz, and 3 kHz as advised by the Committee on Hearing and Equilibrium of the American Academy of Otolaryngology-Head and Neck Surgery for the evaluation of results for treatment of conductive hearing loss [9]. Magnitude of hearing gain was found to be significantly different in patients with mild, moderate & severe MERI score. Significantly more proportion of patients having mild MERI score had a hearing gain of 11-20 dB as compared to that among having severe MERI score. Also, significantly more proportion of patients having severe MERI score had hearing loss / no gain as compared to that among having mild MERI score. Similar results were obtained when the mean hearing gain was calculated with respect to different MERI categories. Mean Percentage gain in hearing was found to be maximum in mild MERI score group, followed by moderate & severe MERI score group in decreasing order. Mean percentage gain in hearing in mild MERI score group patients was found to be significantly high as compared to that in severe MERI score group patients. While the mean percentage gain in hearing in moderate MERI score group subjects did not show any significant difference with other two groups.
So, as the severity of disease increased and the MERI score increased, the mean hearing gain decreased with the increasing MERI score. In the study conducted by Sevim Aslan Felek et al. [10] they also found a statistically significant difference between the mean hearing gain in the mild MERI group as compared to the severe category of MERI. In their study, they also found statistically significant difference in hearing gain between moderate and severe, mild and moderate categories also, but our study although found a clinically significant difference in hearing gain in all three groups but statistical significance was found between mild and severe category only. The study conducted by Khalid Almazrou et al. [11] which was done on children could not find a significant difference in hearing improvement in the different categories made according to the MERI score. In the study conducted by Aftab Ahmed et al. [12], they also stated that there was a significant difference in the hearing gain in mild category of MERI as compared to severe category.
Conclusions
a) MERI scoring is an important tool for assessment of disease severity in cases of COM.
b) It allows us to preoperatively predict the possible outcome of surgery, which helps the surgeon counsel and prognosticate the patient.
c) Lesser the MERI score, more favorable are results in terms of graft uptake.
d) Better hearing gain is seen in patients with lesser MERI score.
e) Being a simple assessment and prognostic tool, MERI scoring can be made a part of surgical work up for every case of COM.
Acknowledgement
The authors would like to thank all the faculty and staff of Department of Otorhinolaryngology and Head Neck Surgery, Maulana Azad Medical College & Associated Lok Nayak Hospital for their generous help and support.
References
- Bellucci RJ (1989) Selection of cases and classification of tympanoplasty. Otolaryngol Clin North Am 22(5): 911-926.
- Austin DF (1972) Ossicular reconstruction. Otolaryngol Clin North Am 5(1): 145-160.
- Austin DF (1985) Reporting results in tympanoplasty. Am J Otol 6(1): 85-88.
- Kartush JM (1994) Ossicular chain reconstruction. Capitulum to malleus. Otolaryngol Clin North Am 27(4): 689-715.
- Becvarovski Z, Kartush JM (2001) Smoking and tympanoplasty: implications for prognosis and the Middle Ear Risk Index (MERI). The Laryngoscope 111(10): 1806-1811.
- Shishegar M, Faramarzi M, Ravari MR (2019) Evaluation of middle ear risk index in patients undergoing tympanoplasty. Eur Arch Otorhinolaryngol 276(10): 2769-2774.
- Kumar N, Madkikar NN, Kishve S, Chilke D, Shinde KJ (2012) Using middle ear risk index and et function as parameters for predicting the outcome of tympanoplasty. Indian J Otolaryngol Head Neck Surg 64(1): 13-16.
- Kalyanasundaram R, Narendran G (2017) Correlation between Middle Ear Risk Index (MERI) and tympanoplasty-A prospective study. Panacea J Med Sci 7(2): 65-67.
- (1995) Committee on Hearing and Equilibrium Guidelines for the evaluation of results of treatment of conductive hearing loss. American Academy of Otolaryngology-Head and Neck Surgery Ffoundation. Inc Otolarygol Head Neck Surg 113: 186-187.
- Felek SA, Celik H, Islam A, Elhan AH, Demirci M, et al. (2010) Type 2 ossiculoplasty: prognostic determination of hearing results by middle ear risk index. Am J Otolaryngol 31(5): 325-331.
- Almazrou K, Alqahtani M, Alshehabi M (2013) Middle ear risk index as a prognostic factor in pediatric ossicular reconstruction. Indian J Otol 19(1): 23.
- Ahmed A, Sharma SC (2016) Middle Ear Risk Index [MERI] as Prognostic Factor in Tympanomastoidectomy with Tympano-plasty. Madridge J Otorhinolar 1(1): 15-22.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...