Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Research Article(ISSN: 2641-1709) 
Post-Operative Complications of Hyperthyroidism Surgery: A Study of 42 Cases Operated in Yaoundé and Douala Volume 9 - Issue 1
Andjock Nkouo Yves Christian1,2*, Bola Siafa Antoine1,3, Mevaa Biouele Roger Christian1,4, Ngono Ateba Gladys5, Anoumedem Ngoufack winnie linda1, Mindja Eko David1,4, Djomou Francois1,3 and Njock Richard1,6
- 1Department of ENT, Ophthalmology & Stomatology, Faculty of Medicine, and Biomedical Sciences, University of Yaounde I, Cameroon
- 2Department of ENT and Head and Neck Surgery, Yaounde General Hospital, Cameroon
- 3Department of ENT and Head and Neck Surgery, Yaounde University Hospital, Cameroon
- 4Department of ENT and Head and Neck Surgery, Yaounde Central Hospital, Cameroon
- 5Department of Anesthesia, Douala General Hospital, Cameroon
- 6Department of ENT and Head and Neck Surgery, Douala General Hospital, Cameroon
Received: September 06, 2022; Published: September 20, 2022
Corresponding author: Andjock Nkouo Yves Christian, Department of ENT and Head and Neck Surgery, Yaounde General Hospital, Cameroon
DOI: 10.32474/SJO.2022.09.000302
Abstract
Introduction: Surgical treatment of hyperthyroidism can achieve rapid euthyroidism but is responsible for recurrence nerve and bleeding morbidity. The aim of this study was to evaluate the postoperative complications of hyperthyroidism surgery and to search for possible risk factors for these complications.
Methodology: This was a retrospective descriptive study, conducted from 1 January 2010 to 31 January 2021, in the university hospitals of Yaounde and Douala. Sociodemographic, clinical, therapeutic and evolutionary data were studied.
Results: 42 patients were included, representing a frequency of 12.8% of thyroidectomies. Female predominance with a sex ratio of seven females to one male. The average age of the patients was 45±11 years. The etiologies of hyperthyroidism were 23 (55%) Graves’ disease, 17 (40%) toxic GMNH and 2 (5%) toxic nodules. Failure of medical treatment was the main preoperative indication (32 patients). Total thyroidectomy was the most commonly used technique (37 patients). 19 (45.2%) patients had postoperative complications. These complications were divided into 1 (2.3%) case of acute thyrotoxic crisis leading to death, 6 (31.5%) cervical hematomas. 3 (15.7%) cases of transient recurrent paralysis. 17 (89.4%) patients had hypocalcemia. Operative mortality was 2.3%.
Conclusion: Surgery for hyperthyroidism is a useful therapeutic modality, albeit with significant complications.
Keywords: Thyroid surgery; hyperthyroidism; Yaounde; Douala
Introduction
Hyperthyroidism is a group of conditions characterized by high circulating thyroid hormone levels. These conditions include Graves’ disease, toxic thyroid adenoma, multinodular goiter (TNG), iodineinduced hyperthyroidism, and thyroiditis [1]. Hyperthyroidism is common, affecting 1-2% of the world’s population with a large female predominance (sex ratio of 8 women to 1 man) [2]. In Cameroon, its prevalence is 24%. [3]. In our environment, medical treatment and surgery are the most commonly used therapeutic modalities [3]. Medical treatment is used in the first instance, but surgical treatment is the one that allows rapid euthyroidism to be achieved [4]. These surgeries are known to be associated with potential complications. Few data found in the literature deal with these complications in our environment. The aim of this study was therefore to study the postoperative complications of patients who underwent surgical management of hyperthyroidism in the ENT departments of the University Hospitals of the cities of Yaoundé and Douala.
Objectives
The general objective was to study the postoperative complications of hyperthyroidism surgery in the university hospitals of Yaounde and Douala.
Specifically:
a) To determine the frequency of hyperthyroidism surgery among thyroid surgeries.
b) To analyse the epidemiological and clinical profile of patients operated on for hyperthyroidism and the type of hyperthyroidism.
c) To identify postoperative complications in patients operated for hyperthyroidism.
d) To investigate the predictive factors for the occurrence of these postoperative complications in hyperthyroid surgeries.
Patients and Methods
We carried out a retrospective descriptive study, from 1st January 2010 to 31st January 2021, in the different university hospitals of the cities of Yaounde and Douala. Six hospitals were involved: Yaounde General Hospital, Yaounde Central Hospital, Yaounde university Hospital, Yaounde national social insurance fund Hospital, Douala Laquintinie Hospital, Douala General Hospital. We included in the study all the records of patients who were previously medically monitored for hyperthyroidism and who underwent thyroidectomy, whatever the technique. From these files, sociodemographic and clinical data concerning hyperthyroidism, medical follow-up and the surgical modality used were collected. We also collected evolutionary data on postoperative complications, as well as the biological outcome of the patients. Data processing and analysis were performed using CS Pro version 7 software. Values of p<0.05 were statistically significant.
Results
During the study period, we recorded 468 thyroid surgeries in the different hospitals, of which 60 were indicated for hyperthyroidism. Of these 60 cases operated on for hyperthyroidism, 8 were excluded because of incomplete records and 10 cases could not be located. We worked with the 42 complete files.
Epidemiological aspects
Frequency of surgical hyperthyroidism
468 cases of thyroid surgery in different hospitals were recorded, of which 60 were indicated for hyperthyroidism, a percentage of 12.8%.
Distribution by gender
Our study population was predominantly female, 88.1% of the total workforce, with a sex ratio (M/F) of seven women to one man.
Age distribution
The mean age of the participants was 45.45 years (±11.25), with a minimum and maximum of 23 and 66 years respectively. The modal age was 37 years. The most represented age group was 30- 60 years with 88.3% (n=35) of cases.
Distribution according to socio-demographic parameters
27 (63.2%) had secondary education, followed by higher education with 11 (26.2%) cases. The majority lived in cities; 37 (88.1%) and the most represented sectors of activity were the liberal sector and the unemployed with 19 (43.3%) and 10 (23.8%) cases respectively.
Clinical aspects
Distribution according to clinical history
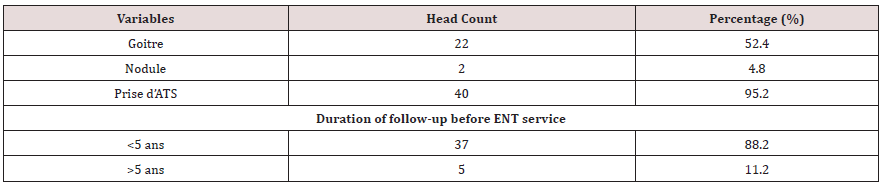
As thyroid history, goitre was found in 22 (52.4%) patients. 40 (95.2%) patients were taking synthetic antithyroid drugs; most of them had been medically monitored for less than 5 years before being referred to the ENT department. Table 1 shows the distribution of the population according to thyroid history.
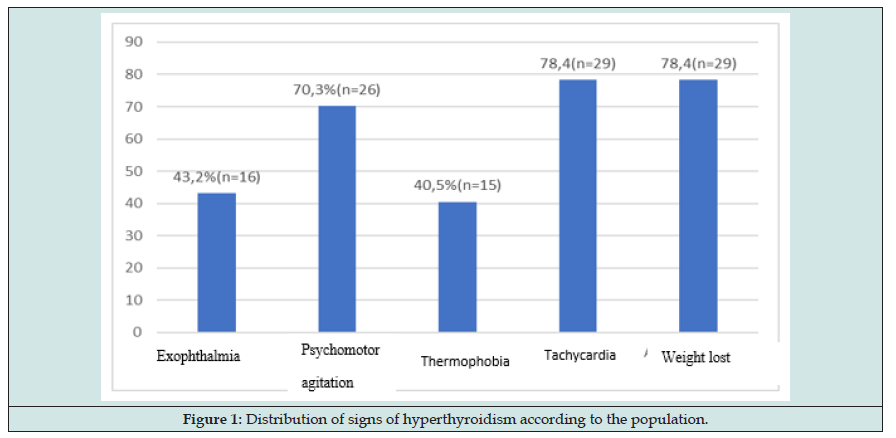
Distribution of signs of hyperthyroidism found in the study population
The main signs of thyrotoxicosis were tachycardia and emaciation found in 29 (78.4%) patients, followed by psychomotor agitation and exophthalmos with 26 (70.3%) and 16 (43.2%) cases respectively. Figure 1 shows the distribution of signs of hyperthyroidism found in the study population.
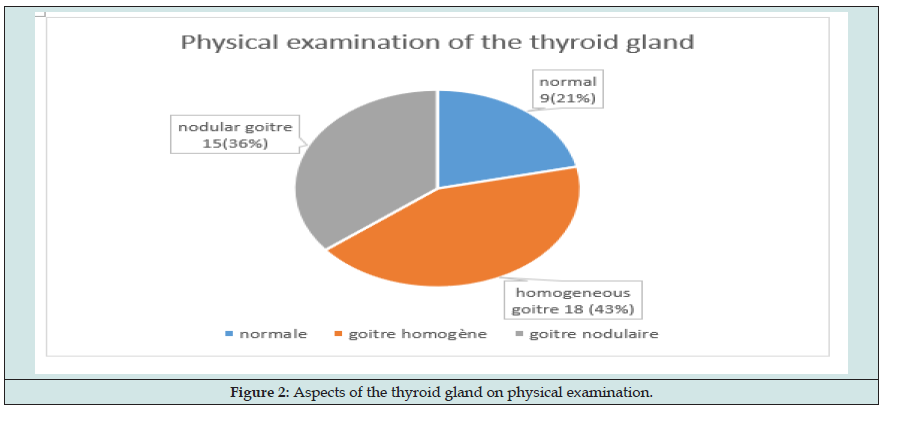
Different aspects of the thyroid gland on physical examination
18 (42.9%) of the study population had homogeneous goitres on physical examination (Figure 2).
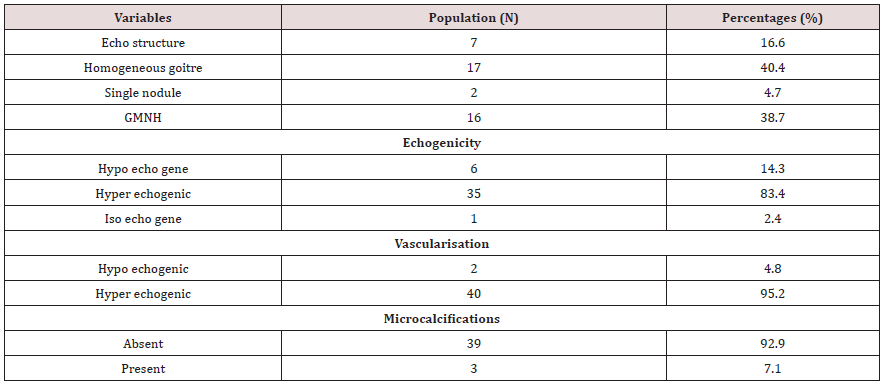
Ultrasonographic aspects of the thyroid glands in the study population
The echo structure revealed a homogeneous goitre and a GMHN in 17 (40.5%) and 15 (35.7%) cases respectively. These lesions were hyperechoic in 35 (83.4%) and hyper vascularised in 95.2% of cases. Microcalcifications were found in 3 patients. Table 2 shows the distribution of the study population according to the ultrasound aspects
TIRADS score of the study population
TIRADS 2 and 3 scores were the most common with 13 (31%) and 20 (47.6%) cases respectively, TIRADS 4 (14.3%) TIRADS 1 (7.1%)
Distribution of the study population according to the etiology of hyperthyroidism
The main etiology of hyperthyroidism was Graves’ disease 23 (55%) cases, followed by toxic multiheteronodular goitre 17 (40%), and toxic nodule 2 (5%).
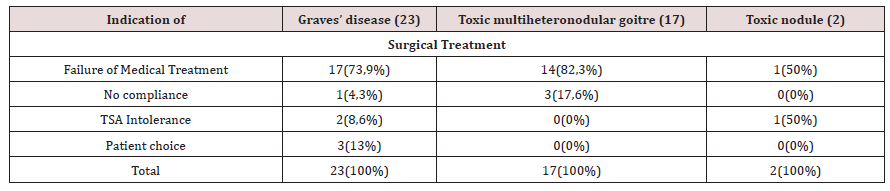
Distribution of the study population according to surgical indications
Failure of medical treatment was the main indication for surgical treatment of hyperthyroidism. Table 3 shows the indications for surgical treatment according to the type of hyperthyroidism.
Preoperative TSH and FT4 values in the study population
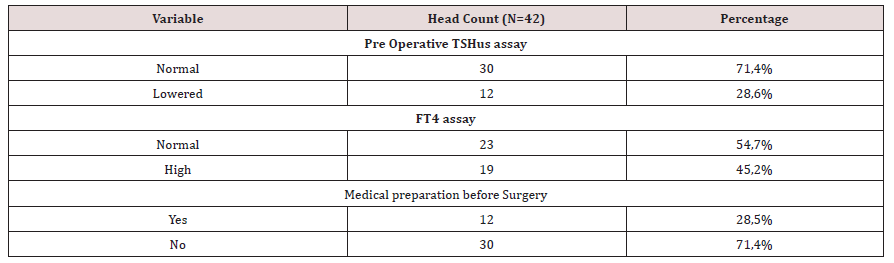
12 (28.6%) of the patients had a lowered preoperative TSH; 19 (45.2%) had an elevated FT4. 12 patients underwent medical preparation of TSA with beta-blockers prior to surgery. Table 4 shows the distribution of the population according to the biological check-up and the anaesthetic preparation.
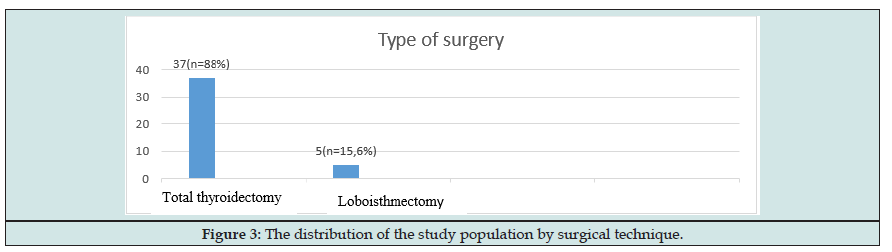
Distribution of the surgical technique used according to the etiology of hyperthyroidism
Total thyroidectomy was the most commonly used surgical technique (88%). No patient had undergone subtotal thyroidectomy. Figure 3 shows the distribution of the study population by surgical technique.
Table 4: the distribution of the population according to biological assessment and anaesthetic preparation.
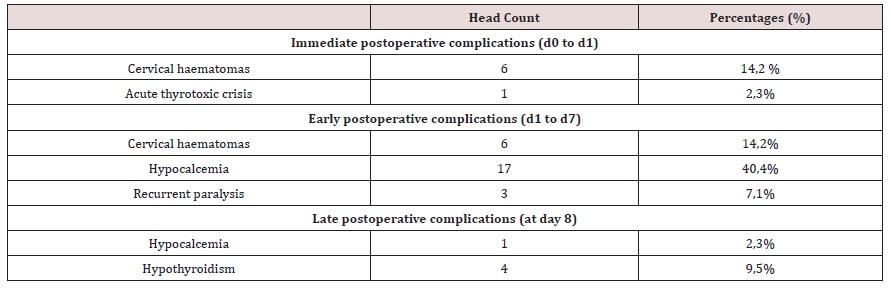
Postoperative complications in the study population
Incidence of postoperative complications
19 patients had postoperative complications, i.e., 45.2% of the population. Of these 19 patients, 17 (40.4%) had transient complications and only 1 (2.3%) had permanent complications. We had 1 (2.3%) case of death.
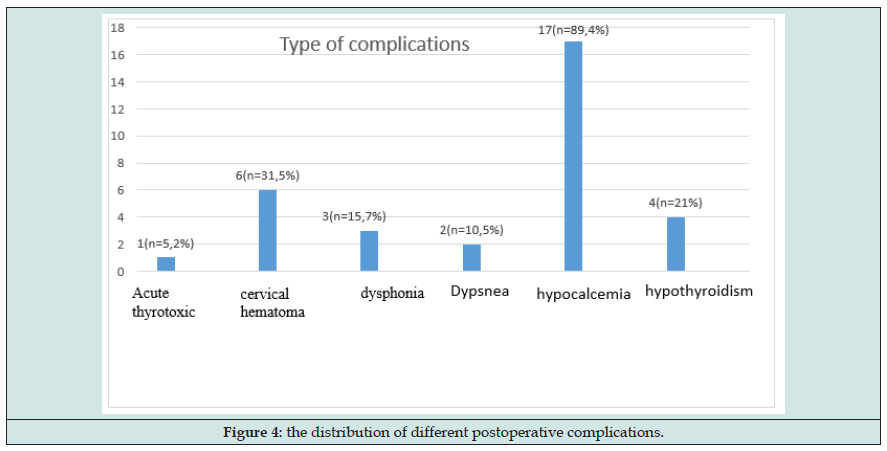
Distribution of postoperative complications
Hemorrhagic (cervical hematoma) and endocrine complications were the most common complications in our series with respectively 31.5% and 89.4%. Among the 6 patients, 3 were compressive cervical haematomas that required repeat surgery. No patient had severe dyspnea requiring tracheostomy. One case of death was recorded in relation to an acute thyrotoxic crisis. Figure 4 shows the distribution of the different postoperative complications.
Evolution of post-operative complications
Early complications were in the majority with a frequency of 61.7%. Table 5 shows the post-operative complications according to time.
Distribution of postoperative complications according to the type of hyperthyroidism
Graves’ disease and toxic GMNH had a similar rate of postoperative complications. The difference was not statically significant (p= 0.23).
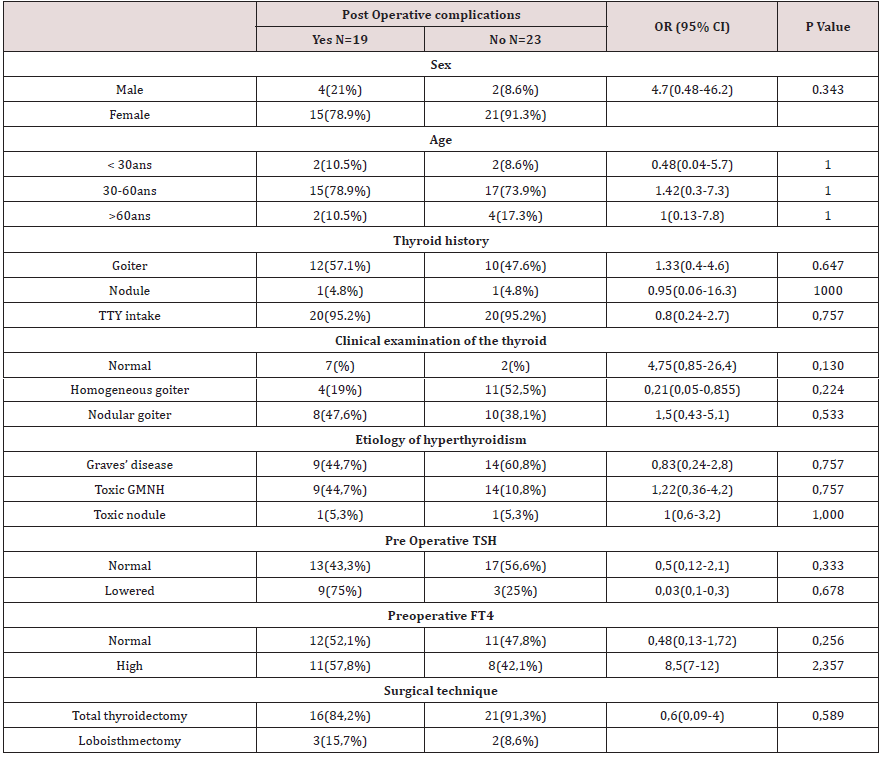
Research into factors predictive of the occurrence of postoperative complications
No significant association was found between the different parameters studied and the occurrence of complications (p>0.05). However, there was a large predominance of postoperative complications in the group with low TSH and those with high FT4. This trend was not significant. (p=0,2). Table 6 shows the correlation between epidemiological, clinical and postoperative complications.
Evolution of TSH in the postoperative period
Postoperatively, we had an increase in the number of euthyroid patients from 30 to 38 patients. This difference was not statically significant. 4 (9.5%) postoperative patients were hypothyroid.
Table 6: Correlation between epidemiological and clinical parameters with postoperative complications.
Discussion
Epidemiological aspects
42 patient files were included in our study. The age of our patients varied from 23 to 66 years with an average of 45 years. The most represented age group was 30-60 years with 88.3% (n=35) of the cases. We also found a clear female predominance in our study (88.1%) with a sex ratio of 7 women to 1 man. These data are superimposed on those of Darouassi et al. [1] who found an average age of 46 years and a female predominance in their series. Ztati [5] also found a majority age range of 40 to 50 years. thyroid disease is a female pathology [6] with the most affected age group being 40-50 years old and even more so in populations of patients with hyperthyroidism which is the second most common cause of thyropathy (24%) after endemic goitre in Cameroon.
Clinical and paraclinical aspects
Weight loss and tachycardia were the most common signs of thyrotoxicosis (78%). These results are similar to those of Koffi et al. [7] in Abidjan, who found in their study a frequency of 87.7% of weight loss and 72.6% of tachycardia. Indeed, tachycardia and weight loss without loss of appetite are the first signs suggestive of hyperthyroidism [8]. We found a homogeneous goitre appearance in 42.9% (n=18) followed by a normal appearance in 35.7% (n=15). In Cameroon, the literature shows a predominance of Graves’ disease, which represents 80% of all cases. [7] of hyperthyroidism in Cameroon, so the clinical aspect is a homogeneity of the gland. The main aetiology of hyperthyroidism was Graves’ disease 23 (55%) followed by toxic GMNH at 40% (n=17). Toxic nodule was found in 2 (5%) patients. Nouedoui et al. [3] found similar results in their series in Yaoundé.
The TIRADS 4 score and the presence of microcalcifications, pejorative elements of malignancy, were not found in 6 (14.3%) and 3 (7.1%) patients respectively. This is consistent with the literature. [1] and is justified by the protective character of hyperthyroidism on malignancy. 12 (28.6%) patients in our study had low ultrasensitive TSH levels (biological hyperthyroidism) at the time of the operative indication. Medical preparation with high-dose synthetic antithyroid drugs over a short period of time to achieve biological euthyroidism before surgery. In accordance with most protocols found in the literature [1].
Therapeutic aspects
Failure of medical treatment was the main indication for surgery in all types of hyperthyroidism. Treatment of hyperthyroidism with synthetic antithyroid drugs is used as first-line therapy in Cameroon and has high recurrence rates of 51-68% [9,10]. Surgery for these cases becomes the only recourse. The main surgical technique found in our series was total thyroidectomy, whatever the aetiology of the hyperthyroidism. The practices found in the literature are similar [11]. This is consistent with the option of radical treatment for hyperthyroidism refractory to medical treatment. One of the particularities of our study is that we found 5 cases (15.6%) of partial thyroidectomies, which is rare, the indications of these partial surgeries were not found.
Post-operative complications were simple in 23 patients (55%) and 19 (45%) patients had post-operative complications. Of these 45% of complications, 40.4% were transient complications. Darouassi, on the other hand, found transient postoperative complications to be lower with 25% in his study population [1]. This difference could be explained by the difference in sample size (42 versus 60). The complication rate found in our series differs from some data in the literature, with lower rates, indeed Bola et al in Cameroon found a rate of 18.9%. This could be explained by the fact that their study also included euthyroid thyroid tumours. [12]. Hypocalcaemia (89.4%), cervical haematoma (31.5%) and recurrent paralysis with dysphonia (15.7%) were the main postoperative complications found. This result is similar to that of Mssouri [11] and Tresallet [13] in 2004. Hypocalcaemia and recurrent paralysis are the most common complications encountered during thyroid surgery. Surgery for hyperthyroidism, particularly Graves’ disease, is known to be quite haemorrhagic due to the chronic inflammation and increased local vascularity. This increases the risk of bleeding complications as found in our series after the standard complications of thyroid surgery [14].
Regarding the evolution of postoperative complications, the vast majority of patients in our study presented transient postoperative complications (40.4%) which resolved within three months of surgery. Definitive complications represented 2.3%. These results correlate with those of Bola and et al. [12] who found a permanent complication rate of 2.2% in their series, in a cohort of 90 thyroidectomies. The postoperative complications of hyperthyroidism surgery are also consistent with those of other thyroid surgeries. We had a mortality rate of 2.3% (n=1) from acute thyrotoxic crisis. Postoperative complications were similarly distributed in patients with Graves’ disease (n=9) and GMNH (n=9). This may be related to the surgical technique used in both groups which was the same, total thyroidectomy. No predictive factors for the occurrence of postoperative complications were found in our study. This may be due to the relatively small sample size and the fact that we were not able to compare the group of patients with postoperative complications to patients with postoperative complications after surgery for other thyropathies. We noted an increase in the number of patients with a normal TSH value on postoperative day 5 (from 30 to 38). This difference was not statically significant. Surgery is a therapeutic modality that offers a fairly rapid normalisation of the ultrasensitive TSH value and is available in all university hospitals in the cities of Yaoundé and Douala. In our series, we found 2 (4.7%) cases of malignancy (papillary carcinoma). Darouassi et al. [1] found one case of vesicular carcinoma in 60 cases (1.67%) [1]. These data are corroborated by those in the literature [7,15]. Although exceptional, malignancy is not uncommon in hyperthyroidism.
Conclusion
Our study found a frequency of surgical hyperthyroidism of 12.8%. Patients aged between 30 and 60 years were the preferred class of hyperthyroidism with a high female predominance. Graves’ disease was the most common etiology (55%), and failure of medical treatment was the main indication for surgery (76.1%). Transient hypocalcaemia (89.4%) and cervical haematoma (31.5%) were the main postoperative complications in our study population. No predictive factors for the occurrence of postoperative complications were found, and the vast majority of patients with a normal TSH us value at postoperative day 5. Although surgery for hyperthyroidism leads to postoperative complications (45.2%), these complications are transient (40.4%) and preventable. Surgery remains a therapeutic modality of choice given the difficulties of access to synthetic antithyroid drugs or radioactive iodine in our country.
References
- Darouassi Y, Hanine M, Aljalil A (2018) Chirurgies des Hyperthyroïdies: A propos de 60 cas. Pan Afr Med J p. 31.
- Adjibabi W, Amoussa Hounkpatin K, Lawson Afouda S (2009) Complications de la chirurgie de l’hyperthyroï Benin Med p. 12-14.
- Nouedoui C, Moukouri E, Juimo A (1999) Les Hyperthyroidies A Yaounde - Cameroun Quelques Aspects Épidémiologiques, Etiologiques Et Thérapeutiques: Bilan De Notre Experience. Médécine Afr Noire 46: 193-198.
- Biet A, Zaatar R, Strunski V (2009) Complications postopératoires dans la thyroïdectomie totale pour maladie de Basedow: comparaison avec la chirurgie des goitres non base dowiens Postoperative. Ann Otolaryngol Chir Cervico Faciale 126: 190-195.
- Ztati M (2014) Traitement chirurgical de l’hyperthyroïdie (À propos de 50 cas). Médécine Interne, Université Cadi Ayyad, Morocco.
- Chakroun A, El Alaoui A (2001) Traitement chirurgical de la maladie de Basedow. J TUN ORL 2: 21-24.
- Lemoine JF (2021) hyperthyroidie: trop d’hormones provoquent un hypermé
- Koffi D, Fagnidi F, Lokrou A (2019) Les Hyperthiroïdies à Health Sci Dis p. 20.
- Corvilain B, Hamy A, Brunaud L (2018) Treatment Of Adult Graves’ Disease. Ann Endocrinol 79(6): 618-635.
- Abraham-Nordling, Bystrom K, Lantz M (2011) Incidence of hyperthyroidism in Sweden. Eur J Endocrinol pp. 899-905.
- Mssrouri, R, Soufi , E, Benamr S (2001) Les hyperthyroïdies chirurgicales à propos de 1181 cas. Abstr 112e Congrès AFC.
- Bola Siafa A, Andjock Nkouo Y, Asmaou Bouba D (2020) Complications and Risk Factors of Thyroid Gland Surgery at the Yaounde University Teaching Hospital from 2013 to 2015. Health Sciences and Diseases pp. 9-15.
- Tresallet C, Chigot J, Menegaux F (2006) Comment prevenir la morbidité réurrentielle en chirurgie thyroidienne? Ann Chir 131: 149-153.
- Roulet M (2019) la maladie de Basedow: facteur de risque de la complication de la thyroidectomie totale. Medecine, d’angers.
- Haraj N, Ahandar H, El Aziz S (2016) Association hyperthyroïdie et cancers différenciés de la thyroï Pan Afr Med J p. 24.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...