Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Research Article(ISSN: 2690-5752) 
Non-Scheduled Surgical Tracheostomy: Our Experience Volume 10 - Issue 4
Lekassa P1,2*, Andjock Nkouo YC3, Agui A1, Ngoma Manfoumbi AB1, Manfoumbi Manfoumbi KD1, Miloundja J1,2, and Nzouba L1,2
- 1ENT and CFS Department, Omar Bongo Ondimba Army Instruction Hospital, Libreville, Gabon.
- 2Department of Surgery and Surgical Specialties, University of Health Sciences, Owendo, Gabon.
- 3ENT and CFS Department, Yaoundé General Hospital.
Received: February 05, 2024; Published: March 05, 2024
Corresponding author: Lekassa P, Department of Surgery and Surgical Specialties, University of Health Sciences, ENT and CFS Department, Omar Bongo Ondimba Army Instruction Hospital, Libreville, Gabon.
DOI: 10.32474/JAAS.2024.10.000342
Abstract
Introduction: Tracheostomy is the temporary or permanent surgical opening of the cervical trachea followed by the placement of a cannula.
Objective: To describe the indications and complications of unscheduled surgical tracheostomy in our context.
Materials and Method: This was a retrospective descriptive study conducted in the ENT and CFS department of HIAOBO, involving 67 medical records of hospitalized patients in whom a surgical tracheostomy was performed in emergency from January 2011 to December 2020.
Results: The study involved 51 men (76%) and 16 women (24%), a ratio of 3.18. The mean age was 45.85 years with extremes of 5 and 78 years. Laryngeal dyspnea was the reason for consultation in 86.57% of cases. The indications were malignant tumors of the upper aero-digestive tract in 54% of cases, difficult extubation in patients in intensive care 12% of cases, laryngeal papillomatosis in 12% of cases, inflammatory pathology 7 cases, traumatic pathology 4 cases, extrinsic compression of the trachea, muscle disease and laryngotracheal stenosis in 1 case each. Tracheostomy was performed under general anesthesia in 73% of cases and under local anesthesia in 27% of cases. Complications were observed (16.42%).
Conclusion: Emergency tracheostomy is a life-saving procedure. The mastery of the technique, the right choice of equipment, the perfect knowledge of the anatomical relationships of the trachea, and the postoperative care make it possible to minimize complications.
Keywords: Emergency tracheostomy; Laryngeal dyspnea; Cancers; Papillomatosis; Foreign body
Research Article
Tracheostomy is the opening of the cervical trachea followed by the placement of a cannula. It is intended to short-circuit the upper airway [1,2]. Its technique can be surgical or percutaneous and concerns both children and adults. The ideal technique is the surgical technique performed in the operating room. Surgical tracheostomy was described and well codified by Chevalier Jackson in 1909 [3]. This procedure is being supplanted by tracheal intubation in developed countries. However, tracheostomy remains an effective means of resuscitation in developing countries. Indeed, it makes it possible to fight against severe respiratory distress or even to prevent it [4]. The unscheduled tracheostomy is performed according to the patient’s clinical condition. Indeed, a dyspneic patient who fights effectively, the tracheostomy is performed in emergency but regulated in the operating room [5]. On the other hand, it is performed in extreme urgency in a patient in the preanoxic stage, with disturbances of consciousness, disappearance of signs of struggle, pauses in breathing and major cyanosis [5]. Tracheostomy is also performed in intensive care on patients on prolonged mechanical ventilation (greater than 7 days) or for difficult extubating [4].
Although tracheostomy remains a life-saving procedure, it involves significant morbidity and mortality [6] and its complications must remain in the minds of healthcare staff because they are sometimes daunting. This surgery is widely practiced in Africa in general and in Gabon in particular where a 1st study was carried out in the ENT and Head and Neck Surgery (CFS) department of the Omar Bongo Ondimba Army Training Hospital (HIAOBO) on tracheotomies and which revealed an incidence of 42.16% of emergency tracheotomies [6]. Thus, these different works highlight the importance of tracheostomy in a hospital setting and the objective of this work was to study the indications and complications of unscheduled tracheostomy in our context.
Materials and Method
This is a retrospective descriptive study conducted in the Department of Otorhinolaryngology and Head and Neck Surgery (ENT and CFS) of the Omar Bongo Ondimba Army Training Hospital (HIAOBO). It included 67 medical records of hospitalized patients who underwent an unscheduled surgical tracheostomy from January 2011 to December 2020. All records of patients who received inpatient or emergency tracheostomy were included. Records of patients who had been tracheostomized for other causes such as safety tracheotomy, tracheostomy performed for intubation during suspension laryngoscopy or prolonged intubation in the intensive care unit were not retained.
Data were collected from the hospitalization register, the operating theatre, consultation records, registers of care procedures and their collection on a standardized survey form. The parameters studied were age, sex, history, time to consultation, reason for consultation, clinical signs, indications for tracheostomy, etiologies of tracheostomy, and complications after tracheostomy. The capture and analysis of our data was carried out using the EPI INFO version 7 software. Microsoft Office’s EXCEL 2013 spreadsheet was used to create the charts. The anonymity and dignity of the patients were respected.
Results
During the study period, 125 tracheostomies were performed, of which 67 were unscheduled and therefore urgent, i.e. 53.6% and an annual incidence of 6.7%. Males accounted for 51 cases (76.12%) and females 16 cases (23.88%), for a sex ratio of 3.19. The median age was 45.85 years with extremes of 5 years and 78 years. The 50-60 age group accounted for 16 cases or 24%. Fifteen patients (22.4%) were under 20 years of age and 52 patients (77.6%) were adults. The symptoms that prompted the consultation were laryngeal dyspnea in 58 cases (86.57%), followed by miscarriage and dysphonia in 2 cases each.
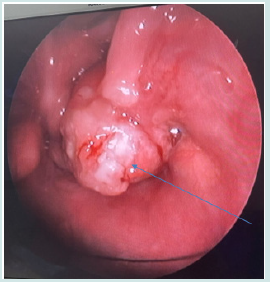
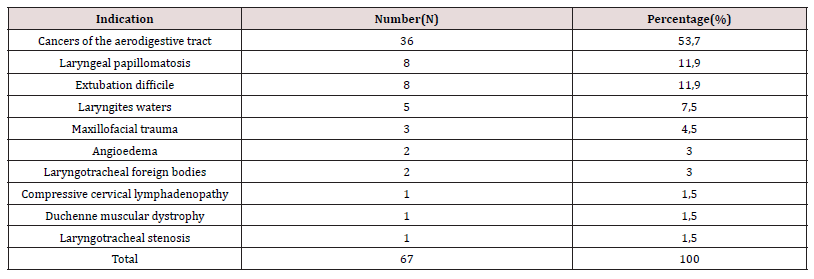
Indications for tracheotomy were pharyngo-laryngeal malignancies with 36 cases or 53.73% (Figure 1) followed by laryngeal papillomatosis (Table I). Tracheostomy was performed in the bedside department or in the treatment room, in extreme emergency, to save patients in 18 cases (27%). These patients had stage 4 dyspnea, for which it was not possible to wait for the availability of the operating room. However, tracheostomy was performed in the operating room in 49 cases (73%). Postoperative follow-up was simple in 56 patients, or 83.6%. However, complications were noted in 11 cases (16.4%).
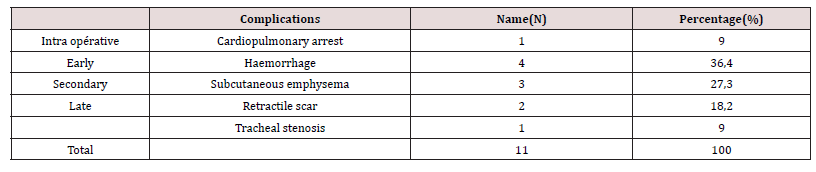
These complications were intraoperative with cardiopulmonary arrest in 1 case, early with hemorrhage in 4 cases (36.36%) and secondary complications such as emphysema in 3 cases (27.27%) (Table II). The mean duration of decannulation averaged 4 to 20 days. However, a patient with nasopharyngeal fibroids kept the tracheostomy tube for 6 months awaiting evacuation for surgical treatment.
Dicussion
Tracheostomy is a common procedure in ENT practice. The hospital prevalence of unscheduled surgical tracheostomies was 53.6%. The annual incidence was 6.7. This result is similar to that of Akolbout et al [5] in Congo, who report 7 emergency tracheostomies per year. However, it is lower than that of Zegbeh-N’guessan et al [6] in Côte d’Ivoire which report 9.75 tracheostomies per year.
An international study by Estéban et al [7] found an average tracheostomy performance of 13.5% in patients. Tracheostomy is a common procedure in ENT practice and a significant inter-country variability.
The male predominance noted in this series is also reported by other authors [4]. This can be explained by the fact that certain pathologies such as laryngeal tumors are more common in men than women. The same applies to laryngeal papillomatosis and lower respiratory tract foreign bodies (RIB) in children [8]. The median age in this study was 45.8 years. These results are higher than those of Dalil et al [9] in Gabon, with an average age of 40.62 years, and Goueta et al [4] in Burkina Faso, who report an average age of 37 years.
The explanation may be the fact that cancerous pathologies of the upper aerodigestive tract, which represent the majority of indications for tracheostomy, are more common in adulthood. Emergency tracheostomy is indicated when there is life-threatening upper respiratory distress and tracheal intubation is impossible or contraindicated. In this series, the tracheostomy was performed under local anesthesia in 27% of cases, at the patient’s bedside or in the treatment room in extreme emergency. Zegbeh-N’guessan et al [6] report 10.2% of tracheostomies performed in the chair. Akoboult et al [5] performed 91% of tracheostomies under local anesthesia, of which 4% were performed at the sickle bed in 4%.
When the patient arrives in or presents respiratory distress in the ward and the operating theatres are unavailable, tracheostomy is required in the ward [8]. Tracheotomy is usually an emergency procedure in an ENT specialist. Indeed, since its origins, tracheostomy has been a life-saving emergency procedure; respiratory distress being the main indication. It was performed in the operating room in 73% of cases. In the study by Zegbeh- N’guessan et al [6], tracheostomy was performed in the operating room in 89.74%.
The reason for consultation in this study was essentially laryngeal dyspnea with 86.57% of cases. This finding agrees with several studies such as that of Akobout et al [5] which report 96% of cases of dyspnea[9]. Respiratory distress accounted for 78.94% of cases in Kabore’s study [10]. Tracheotomy is a life-saving procedure for paroxysmal respiratory failure. In our countries, tracheostomy is often the only alternative in the face of dyspnea, which is lifethreatening in the short term. The underlying ENT pathology was dominated by pharyngo-laryngeal tumors with 61%. Dalil et al [9], in Gabon in the same ENT and CCF department report 36%. The study by Akolbout et al [5] in Congo shows a predominance of these tumors with 41.81%.
This can be explained in our context by a delay in consultation, the clinical signs such as dysphonia long neglected by patients. Thus, patients consult at an advanced stage of the disease. This emergency tracheostomy was performed for very advanced lesions classified as T3 and T4. In developed countries, the alternative to tracheostomy for dyspneizing VADS tumors is laser de obstruction [11]. Thus, the large series of 266 patients with malignant tumors of the larynx and hypopharynx, reported by Breneman of the University of Cincinnati, includes only 7.9% of tracheostomy cases [12]. In children, the etiology of laryngeal dyspnea in this study was laryngeal papillomatosis with 11.94%, followed by dyspneizing laryngitis with 7.46%. In the study by Akolbout et al [5], laryngeal papillomatosis was found in 21.81% of cases. Vroh et al [13] show that papillomatosis was the 2nd most common pathology leading to a tracheostomy with 21.87% and in first place were laryngotracheal foreign bodies with 37.5% of cases. Acute dyspaeizing laryngitis was noted in 7.47% of cases in this study. In the Badiane series [14] in Senegal, they accounted for 3.72% of tracheostomies performed.
In our developing countries, where there is a proven shortage of qualified personnel, and where extraction equipment is not always suitable and available, it seems prudent to us to first ensure the freedom of the lower respiratory tract by means of tracheostomy [5]. Complications of emergency surgical tracheostomy are diverse. In this series, 83.6% of postoperative outcomes were simple. However, complications were noted in 16.88% of cases. These complications were intraoperative in 1 case, early postoperative in 5 cases, secondary in 3 cases and late in 2 cases. The study by Goueta et al [4] found intraoperative complications in 7 cases, early complications in 9 cases, secondary complications in 5 cases, and late complications in 4 cases. Our study mainly found secondary complications with mainly hemorrhage in 5 cases, all of which required exploration and hemostasis in the operating room under general anesthesia. This was followed by subcutaneous emphysema in 3 cases. The series of Goueta et al [4] finds that the most frequent complications were cannula obstructions by a mucosal plug with 16% of cases, followed by subcutaneous emphysema with 12% and bronchopulmonary disease with 12% of cases.
The emergency context in which the majority of our tracheotomies are performed could explain this high complication rate in our context. Tracheostomy has a significant morbidity and mortality that remind us that it is a surgical procedure requiring mastery of the surgical technique, a minimal technical platform and rigorous asepsis [4, 15]. In the series of Zegben-Nguessan et al [6], the complication rate was 10.26% and cardiopulmonary arrest was the most objectified complication intraoperatively with 57.14%, followed by obstruction by the mucosal plug. The mean time to decannulation in this series averaged 3 to 60 days. A patient with nasopharyngeal fibroids kept the cannula on for 6 months while waiting to be evacuated for surgical treatment. In Goueta’s study [4], this time frame was 17 days, with extremes of 1 day and 40 days. The mortality rate in this study was 9.09%. The study by Goueta et al [4] notes a mortality rate of 3.7%.
Conclusion
Unscheduled tracheostomy is performed in our context for the management of severe laryngeal dyspnea.
This simple, life-saving surgical procedure with the slightest material and personnel requirements should be known to every doctor to provide assistance in case of need.
References
- Laccourreye L, Dubin J (2015) Traché EMC (Elsevier, Paris), Techniques chirurgicales-tête et cou 46-430.
- Chouikh C, El Moqaddem A, Benmakhlouf A, Naanaa S, and El koraichi A, et al. (2014) Migration -trachéale dune canule de trachéotomie: complication exceptionnelle. Pan African Medical Journal 18(41): 1-3.
- Jackson C (1909) Tracheostomy. Laryngoscope 19: 285-90.
- Gouéta A, Oubian S, Sanou E, Bakyono KE, and Bambara C, et al. (2020) Complications de la trachéotomie en ORL au Burkina Faso. J accr Africa 4(3): 359-65.
- Akolbout D, Itiere Odzili Fa, Gérard Chidrel Ngouoni Gc, Gontran Ondzotto G, and Otouana B, et al. (2016) Trachéotomie En Urgence À Propos DE 55 CAS : Expérience Du Chu De Brazzaville. Annales De L’université Marien Ngouabi, 16(1): 12-18.
- Zegbeh-N’guessan EK, Bérété PIJ, Ory DMAO, Djemi EM, and Ngattia KV,et al. (2023) Trachéotomie: indications et avantages dans la prise en charge des patients en Chirurgie Maxillo-Faciale au CHU de Bouaké (Côte d’Ivoire). J TUN ORL 49: 21-24.
- Esteban A, Anzueto A, Frutos F, Alia I, and Brochard L, et al. (2002) Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA 287(3): 345-55.
- Mvoumi OS, Ndock R, Ndjolo A, Bengono G (2005) Trachéotomie en urgence à l’Hôpital Général de Douala(Cameroun). Rev Afr Orl 1(3): 63-66.
- Kabore A (2018) Trachéotomie dans le service d’Oto-Rhino-Laryngologie et Chirurgie Cervico-Faciale du Centre Hospitalier Universitaire Sourô Sanou de Bobo-Dioulasso: technique, indications, ré Thèse N°153, Université Nazi Boni. Institut Supérieur Des Sciences De la Sante (IN.S.SA).(Burkina-Faso).
- Dial A, Miloundja J, Ngonyeki A, Nzenze S, and Nziengui A, et al. (2015) La trachéotomie à l’hôpital d’instruction des armées Omar Bongo Ondimba-Libreville. Med Afr Noire 62(5): 271-275.
- Paleri V, Stafford FW, Sammut MS (2005) Laser debulking in malignant upper airway obstruction. Head Neek 27(4): 296-301.
- Breneman JC, Brad Shaw A, Gluckman J, Aron BS (1988) Prevention of stornal reccurence for advanced laryngeal and pharyngeal tumors. cancer 62(4): 802-805.
- Vroh BTS, Adjé YA, Ory OAD, Zégheh NE, and Kouassi NH, et al. (2023) Trachéotomie chirurgicale chez l'enfant au centre hospitalier universitaire de Bouaké à propos de 32 cas / Surgical tracheotomy in children at the university hospital center of Bouake about 32 cases. Rev Col Odonto-Stomatol Afr Chir Maxillo-fac 30(3): 73-77.
- Badiane O (1999) La trachéotomie dans un service d’ORL d’Afrique noire: bilan de 10 ans. Thèse en Médecine N°44 Université Cheick Anta Diop de Dakar.
- Koffi Aka V, Kouassi A, Adjoua RP, De Meiederos E, and Ehono E (2004) Trachéotomie en urgence: expérience du service d’ORL du CHU de Treichville(Abidjan). Med Afr Noire 51(6): 301-305

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...