Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Mini Review(ISSN: 2641-1709) 
NIS Amplification In A Rare Combination of Three Histological Subtypes of Collision Tumours of Thyroid Gland Identified by Whole Body I 131 and PETCT Imaging Volume 7 - Issue 4
P Shanmuga Sundaram* and Subramanyam Padma
- Clinical Professors, Department of Nuclear Medicine & Molecular Imaging, Amrita Institute of Medical Sciences & Research Centre, Amrita Vishwa vidyapeetham University, Kerala, India
Received: November 15, 2021; Published: November 30, 2021
Corresponding author: P Shanmuga Sundaram, Clinical Professor, Department of Nuclear Medicine & Molecular Imaging, Amrita Institute of Medical Sciences & Research Centre, India
DOI: 10.32474/SJO.2021.07.000269
Abstract
Radio iodine (I 131) is popularly called as a ‘magic bullet’ due to its maximum tumoricidal action (with least side effects) over thyroid remnant as well as in metastatic deposits in postoperative settings of Differentiated thyroid cancers (DTC). However, for undifferentiated and rare squamous cell thyroid cancers, different treatment options have been described which include surgery, chemotherapy and radiation with poor outcomes. Orally administered I 131 is maximally beneficially in thyrocytes concentrating I 131. Its targeted tumoricidal action is based on the crossfire effect arising from the 606 kilo electron volts beta irradiation that it exerts on thyrocytes. We present a case of an elderly lady with a rapidly enlarging neck mass. Patient underwent total thyroidectomy, cervical nodal clearance, and extensive tumour debulking followed by external radiotherapy to neck. Histopathology revealed collision tumour consisting of 3 different thyroid cancers; one component of differentiated (papillary) and 2 undifferentiated (Squamous cell Ca, SCC and anaplastic) variants. 18F Flurodeoxyglucose Positron emission tomography – computed tomography, FDG PETCT imaging was performed as part of the staging workup for SCC. PETCT showed a large neck mass with local infiltration and nodal metastases. Although stimulated thyroglobulin (Tg) was only 0.04 ng/ml, based on the DTC component, I 131 whole body scan was performed. Images revealed I 131 uptake due to sodium iodide symporter (NIS) expression in DTC part of the residual neck mass that was FDG negative (‘Flip flop phenomenon – I 131 positive but FDG negative’). Due to the identification of I 131 concentrating papillary component, patient was considered suitable for high dose I 131 therapy. Nuclear medicine investigation has helped in the staging of thyroid malignancy, prognosticating the aggressive nature of disease and by way of demonstrating NIS amplification in part of neck mass, received therapeutic benefit in the form of high dose I 131 therapy.
Keywords: Radio iodine, Collision tumour; thyroid gland; Undifferentiated thyroid cancer; Anaplastic thyroid cancer; Squamous cell thyroid cancer
Introduction
As per 2018 cancer screening registry, there were an estimated 53,990 new cases of thyroid cancer and over 750,000 people living with thyroid cancer [1]. DTC is the commonest form of thyroid malignancy arises from papillary or follicular cells, having a good prognosis. Primary SCC and Anaplastic variants of thyroid cancer (ATC) are aggressive types of undifferentiated thyroid malignancy with overall poor prognosis and a poor survival rate [2,3]. Both ATC and primary SCC are exceedingly rare forms of thyroid malignancy occurring in less than 1 % of population. Usually, the anaplastic variant arises from mutational transformation of one of the DTC variants like papillary, follicular or Hürthle cell carcinoma [4]. Primary thyroid SCC is extremely rare due to the absence of squamous epithelium in thyroid gland. SCC may arise as a primary tumour within the thyroid gland or as a component of anaplastic or undifferentiated thyroid tumours over a period. Our case highlights three important factors. There is no literature evidence showing a composite tumour of thyroid combining Thyroglobulin (Tg) secreting and 2 rare non-secreting aggressive components in the same patient. Secondly the duration of goitre is noticeably short; therefore, it may be assumed that cellular differentiation and malignant transformation from one variant to another may be rare in this case. Lastly a unique aspect of presenting this case is based on the NIS amplification in part of the right lobe thyroid lesion that was easily captured by I 131 scan leading to better therapeutic benefit from high dose I 131 therapy in the background of ATC and SCC harboring a dismal prognosis. We present the following article in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/aot-20-64).
Case Presentation
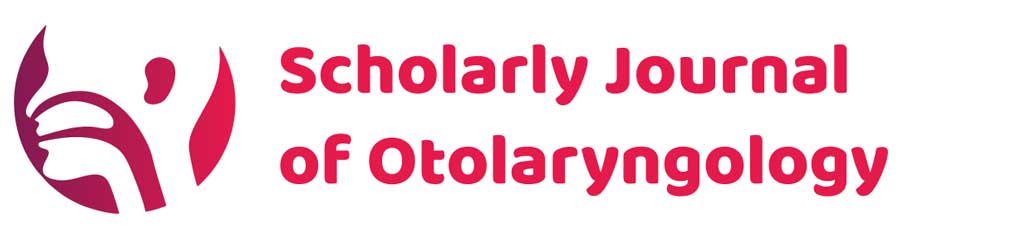
72-year-old lady presented with history of neck swelling of 2 months duration with sudden increase in size and local pain for 1 week. Clinical examination showed an ill-defined neck mass with nodularity occupying a large part of anterior neck. Mass was firm to hard in consistency measuring 9 x 8 cm, freely mobile on palpation with no breathing or swallowing difficulty. No obvious cervical lymphadenopathy was noted separately from the neck mass. Ultrasonography examination of neck revealed a TIRADS -3 nodule in left lobe of thyroid gland with retrosternal extension and causing minimal tracheal compression. Another small TIRADS -3 nodule in right lobe of thyroid gland was also noted. Thyroid function test was normal (FreeT4 1.6 ng/dl, normal 1-1.6, and TSH 2.9 uIU/ml, normal 0.27-4.3). FNAC was done from left lobe thyroid mass, and was reported as primary SCC of thyroid or metastatic deposit from an unknown primary. 18F FDG PETCT showed FDG avid left thyroid lobe replaced by an ill-defined, solid cystic heterogeneously enhancing mass extending upto superior mediastinum with infiltration into left Internal jugular vein (IJV) and causing encasement of the left internal carotid artery in its mid portion (Figure 1 A & B). Right lobe hypo enhancing nodule showed no abnormal FDG uptake (representing the DTC component, that displayed I 131 positivity on whole body I 131 scan). Metabolically active bilaterally level III cervical, left supraclavicular and highest mediastinal lymphnodal metastases were also reported (Figure 1C). FNAC, Fine needle aspiration cytology of FDG avid cervical lymph nodes confirmed metastasis from ATC and sample from left supraclavicular node revealed nodal metastases from SCC.
Figure 1: A: CT transaxial image.
B: Fused PETCT transaxial image.
C: MIP image (maximum intensity projection). Left thyroid lobe (bold arrow) appears completely replaced by an ill-defined
solid cystic, heterogeneously enhancing FDG avid mass measuring 7.4 x 7.0 x 8.5 cms causing tracheal shift to right, infiltrating
the strap muscles. Left IJV appears to be infiltrated by the mass. More than 180-degree encasement of the left common carotid
artery in its midway by the mass. Right lobe of thyroid shows another 7 x 12 mm hypo enhancing nodule (FDG non avid). Mass
lesion is extending into the superior mediastinum, however there is no retrosternal extension. FDG avid left level II, III and IV
nodal metastases ( dotted arrow), largest 10 mm in size. Another 13 x 8 mm FDG avid prominent superior mediastinal nodal
metastases was also noted.
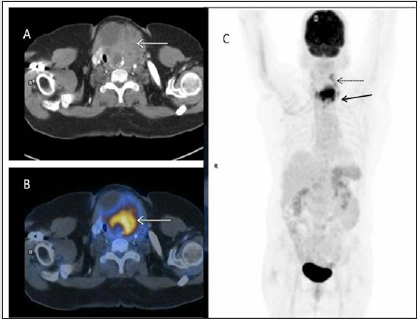
Patient subsequently underwent Total thyroidectomy, laryngeal shaving, central compartment clearance, right selective neck dissection (level II-IV), left modified radical neck dissection and Tracheostomy. Histopathological examination of Total thyroidectomy specimen (Figure 2) showed Papillary thyroid carcinoma associated with squamous cell carcinoma and features favouring an anaplastic thyroid carcinoma, squamous cell type [4x, hematoxylin and eosin (HE)]. Cohesive malignant cells were arranged in sheets, nests, cords, islands and trabeculae pattern. The large malignant cells exhibited pleomorphism, hyperchromatic to vesicular nuclei with large prominent eosinophilic nucleoli and abundant eosinophilic cytoplasm. Individual keratinization and intercellular bridges were visualized along with tumour cell spindling. Tumour size: 8.3x7.5x5cm involving left, right lobe and isthmus. No vascular invasion was seen. No solid or poorly differentiated areas were noted. No lymph vascular emboli or perineural invasion was seen. The tumour was abutting the strap muscles. Extrathyroidal extension was seen. All the resected margins were found to be free of tumour. Vessel cut margin and strap muscles were free of tumour. Lymph nodes dissected were 62 in number and all were free of tumour. Parathyroid tissue in the specimen was also free of tumour. Background showed lymphocytic thyroiditis. Histologically as per AJCC (American Joint Committee on Cancer) the tumour was staged as pT4N0. In view of the tracheal compression and laryngeal involvement, post-operative adjuvant radiation therapy (RT) using image guided radiotherapy, IGRT technique was advised, RT was given to tumour bed, thyroid bed and Bilateral level II, III,IV, V, VI nodal stations using 6 MV (Mega volts photon), 5400 centigray in 30 fractions. The RT portal site included mediastinal nodal regions upto carina.
Figure 2: Histology of the neck mass.
A: Anaplastic thyroid cancer with adjacent papillary component (x 200).
B: Keratin pearls indicating SCC of thyroid.
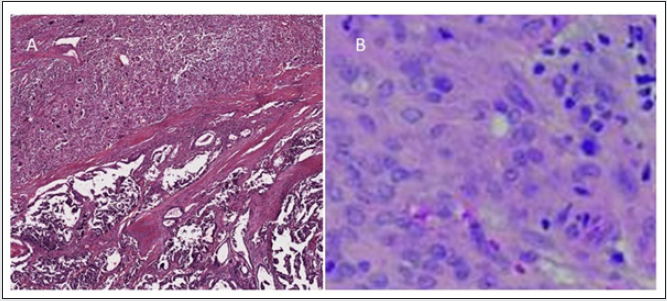
Patient was put on nasogastric tube feeds. Inspite of stimulated Tg being less (non-secretory status), only 0.04 ng/ml (Normal < 2 ng/ml) indicating a predominantly undifferentiated type of thyroid cancer; patient was scheduled for Residual thyroid and whole body I131 Scan (WBI). Images revealed focal I-131 uptake in right side of anterior neck. This is found to coincide with the histopathological report of a small papillary component that maybe contributing to low Tg secretion. Based on NIS expressing thyroid lesion on right side of neck, patient was considered suitable for high dose I 131 therapy as a therapeutic tool to target DTC part of thyroid mass. Patient was treated with 3367 MBq ( Mega Becqueral) of I131 via nasogastric tube as patient is unable to swallow liquids. Post therapy WBI scan was also performed (Figure 3). Comparing FDG PETCT and post therapy WBI scans, there is clear demarcation of the papillary ( I 131 avid) and undifferentiated component (FDG avid) of thyroid malignancy ( Figure 4). ( ‘Flip flop phenomena’). 2 months later, follow-up CT of neck showed significant reduction in tumour size in anterior neck. Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The procedures performed in this patient were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the imaging procedure, publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
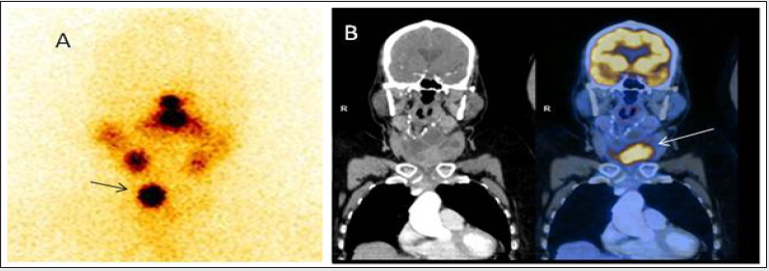
Figure 3: A: Diagnostic whole body I 131 scan.
B: Post therapy whole body I 131 scan in anterior and posterior projection. Arrow indicating the site of NIS expression involving
right lobe of thyroid gland. The aggressive component of neck mass which was FDG avid on PET scan is not amplified in I 131
scan due to the presence of highly dedifferentiated thyrocytes, confirmed with histology.
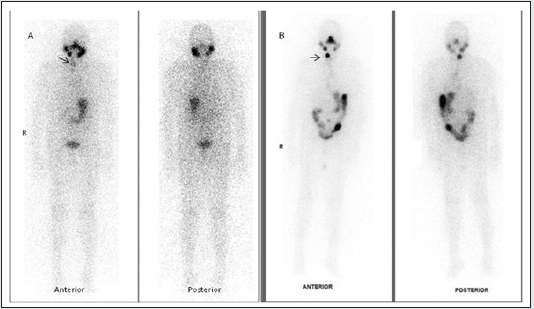
Figure 4: Depiction of Flip flop phenomenon. A. Post therapy I 131 thyroid scan in anterior projection highlighting the focal NIS expression in right lobe papillary component thyroid lesion (arrow), which is FDG non avid on FDG PET scan. B. Neck CT and Fused FDG PETCT image in coronal section showing the predominantly cystic with solid component FDG avid left lobe thyroid lesion with (Standard Uptake Value) SUV max 11.3 g/ml( I 131 negative).
Discussion
Both SCC and ATC occur in elderly population with a 2
: 1 female to male ratio. 50% of patients tend to have prior
multinodular goiter [3].The commonest presentation is a rapidly
growing neck mass with progressive pressure symptoms like
dysphagia, hoarseness, dyspnea, neck pain, sore throat, and cough.
30 - 40% of patients are found to have distant metastases (lung,
bone and brain). Extrathyroidal extension is seen in majority
of cases. Malignant tumours with dual pathology co existing in
thyroid gland are rare. This can be classified as collision tumour,
mixed or composite tumours [5]. Collision tumour is described
when there is presence of two adjacent but histologically distinct
and morphologically independent malignant tumours in the same
organ with no histological admixture. In contrast, the term mixed
tumour is used when there is a histological admixture of the two
tumours in the same organ with a common cell of origin [5]. The
term composite tumour, in turn, refers to the condition where a
tumour contains two discrete cell populations as with thyroglobulin
positive papillary carcinoma cells and calcitonin-positive medullary
carcinoma cells [6]. Collision tumours can occur in various organs
such as the ovaries, colon, lung, stomach, skin, and kidneys but are
extremely rare in the thyroid. The most common type described
is the presence of mixed histology consisting of papillary and
medullary carcinomas.
Here we report collision tumour of thyroid gland with a rare
combination of three different histological subtypes seen together
i.e., SCC, ATC (undifferentiated very rarely occurring thyroid
cancers along with papillary component of DTC. Theories have
been put forth to explain the onset of such collision tumours
in thyroid [6]. The first is an accidental union of two primary
tumours. Another hypothesis is the stem cell theory where cancer
stem cells differentiate and branch out as two different tumours.
The other theory is based on the alteration of tumour biology and
microenvironment by presence of the first the tumour facilitating
the development of the second primary tumour or seeding of
metastatic tumour cells [7]. Treatment for collision tumours
depends upon the combination of histological thyroid cancer
subtypes involved. Each component of the malignant cell lineage
should be treated like an independent primary malignancy. Both
SCC and ATC need multimodality therapy regimens like surgery,
radiation, or chemotherapy. In spite of multimodality management,
the therapeutic benefit derived is marginal given the aggressive
nature of the disease. In situations where only a single modality
is used for therapy, the local-regional disease recurrence is high and overall survival is poor. The case is different in DTC patients
and displays a good overall prognosis by I 131 therapy alone. The
incremental value of successful thyroid ablation in DTC is based
on the unique ability of thyroid follicular cells to trap and organify
iodide due to expression of NIS. NIS is an integral plasma membrane
glycoprotein that mediates active transport of iodide into thyroid
follicular cells [8]. This facilitates imaging as well as effective
therapy for DTC, thereby improving the prognosis of thyroid cancer
patients significantly. Papillary carcinomas arise from the thyroid
follicular cells and frequently harbor BRAF V600E mutations,
produce thyroglobulin, and express the NIS leading to I 131 uptake
in cancerous and normal thyrocytes expressing NIS gene. This
property is lost in undifferentiated thyroid cancers thus high dose I
131 therapy is not useful in treating this group of undifferentiated
and SCC thyroid malignancies.
Conclusion
This case highlights the incremental role of WBI scan signalling NIS expression and FDG PETCT in identifying the areas of aggressive thyroid tumours in a patient with triple tumour histologies. WBI scan has helped in the staging and prognosticating of the disease. Due to the NIS amplification, patient was offered the chance of deriving therapeutic benefit from yet another modality apart from surgery, radiotherapy, and chemotherapy. Although Tg level was very low, the objective evidence of focal I 131 concentration in right side of neck mass provided the desired benefit from high dose I 131 therapy with high reliability. In spite of the overall dismal prognosis of ATC and SCC, multimodality treatment significantly improved local control and appears to afford long-term survival.
Acknowledgement
Acknowledgement: Nil, Funding: None.
Conflict of Interest
Conflict of Interest: All authors have completed the ICMJE uniform disclosure form. The authors have no conflicts of interest to declare.”
References
- Ries LAG, Melbert D, Krapcho M, Stinchcomb DG, Howlader N, et al. (2018) SEER Cancer Statistics Review, 1975-2015, National Cancer Institute. Bethesda (Eds.), SEER data submission, posted to the SEER.
- Wang W, Ouyang Q, Meng C, Jing L, Li X (2019) Treatment optimization and prognostic considerations for primary squamous cell carcinoma of the thyroid. Gland Surg 8(6): 683-690.
- Ibrahim MI, Jusoh YR, Adam NN, Mohamad I (2018) Primary Squamous Cell Carcinoma of the Thyroid Gland. Iran J Otorhinolaryngol 30(96): 65-68.
- Hunt JL, Tometsko M, LiVolsi VA, Swalsky P, Finkelstein SD, et al. (2003) Molecular evidence of anaplastic transformation in coexisting well-differentiated and anaplastic carcinomas of the thyroid. Am J Surg Pathol 27(12): 1559-1564.
- Thomas VP, George R (2018) Collision tumours of the thyroid: Review of literature and report of a case of papillary-Follicular collision tumour. Thyroid Res Pract 15: 60-64.
- Gurkan E, Gurbuz Y, Tarkun I, Canturk Z, Cetinarsian B (2014) Mixed medullary-papillary carcinoma of the thyroid: Report of two cases and review of the literature. Indian J Pathol Microbiol 57: 598.
- Walvekar RR, Kane SV D'Cruz AK (2006) Collision tumor of the thyroid: follicular variant of papillary carcinoma and squamous carcinoma. World J Surg Onc 4: 65.
- Hingorani M, Spitzweg C, Vassaux G, Newbold K, Melcher A, et al. (2010) The biology of the sodium iodide symporter and its potential for targeted gene delivery. Curr Cancer Drug Targets 10(2): 242-267.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...