Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Research Article(ISSN: 2641-1709) 
Nasolabial Cysts: International and Multicentric Series Volume 9 - Issue 1
Vansteelant G1*, De Dorlodot Cl1, Hox V2, Riahi I3, Lahlimi Hamza4 and Eloy Ph1
- 1Department of ENT & HNS, CHU UCL Namur, Belgium
- 2Department of ENT & HNS, Saint Luc UCL Brussels, Belgium
- 3Department of ENT, CHU Charles Nicolle, Tunisia
- 4Department of ENT, CHU Hassan II, Route Sidi Harazem, FEZ, Morocco
Received: September 14, 2022; Published: September 26, 2022
Corresponding author: Géraldine Vansteelant, Department of ENT & HNS, CHU UCL Namur, Saint Luc UCL Brussels, Belgium
DOI: 10.32474/SJO.2022.09.000304
Abstract
Introduction: Nasolabial cysts, also known as nasoalveolar cysts are benign, non-odontogenic, soft tissue cysts located in the nasolabial fold. The cysts occur unilateral or rarely bilateral and have been found to be most prevalent amongst middle-aged women of Asian or African American descent.
Methods and Results: We report a retrospective study on 27 patients presenting a nasolabial cyst, diagnosed and treated between 2010 and 2022. The case series includes 20 women and 7 men (mean age was 45) from 3 different countries: Belgium, Tunisia and Morocco.
The reported symptoms were alar deformity in 24 cases, nasal obstruction in 6 cases and recurrent infection in 15 cases. 4 patients were treated with oral antibiotics alone whereas 23 patients underwent surgery. The surgery consisted of external sublabial excision in 19 cases or assisted endoscopic endonasal marsupialization in 4 cases. There was no recurrence of the cyst upon a minimum follow-up of more than 6 months except for in one patient who underwent revision surgery.
Conclusion: Nasolabial cysts are located in the premaxillary region. They are particularly rare in Belgium and seem to be more common in North African countries. There is a female preponderance. The diagnosis is made by clinical examination and imaging. CT scan is the most common imaging modality because of its availability in many countries and lower cost than MRI. However, MRI is the best imaging modality to diagnose small lesions. Surgery is usually required. Two main treatment procedures are reported: limited intraoral sublabial surgery or endoscopic transnasal marsupialization, both surgery modalities have positive outcomes.
Keywords: Nasolabial cyst; Endonasal surgery; Nasal; Cyst; CT; MRI; Sublabial approach
Introduction
Nasolabial cysts, also known as nasoalveolar cysts are benign cysts. They were first described by Zuckerkandl in 1882 [1]. The cysts are soft tissue, non-odontogenic cysts located in the nasolabial fold. They have an incidence of 0.7% among all cysts in the maxillofacial region and 2.5% among non-odontogenic cysts. There is different hypothesis about the embryological origin of nasolabial cysts, the cyst is either formed by detention of cells either from the maxilla medial and lateral nasal wall, or by detention of cells from the inferior nasolacrimal channel [2]. The differential diagnosis must be made with odontogenic or periapical cysts, cysts of maxilla, central line cysts, epidermal inclusion cyst, periapical granulomas and finally neoplastic lesions [3]. The cysts are unilateral and affect middle-aged (40–50-year-old) women [4]. These lesions can expand into the anterior nasal floor but remain submucosal and extraosseous. When the cysts are symptomatic, surgery is the treatment of choice and there are 2 main surgical methods: the sublabial or endonasal approach [5]. According to the current literature, no expansive case series have been reported from North Africa and Europe.
Patients and Methods
This retrospective study includes 27 patients presenting a nasolabial cyst diagnosed and treated between 2010 and 2022. The patients were diagnosed at the Department of Ear, Nose and Throat of 3 different ENT centres in Belgium, Tunisia and Morocco. General clinical characteristics were retrieved from medical files, including the data about the clinical presentation, preoperative investigations, treatment, complications and finally the outcome.
Results
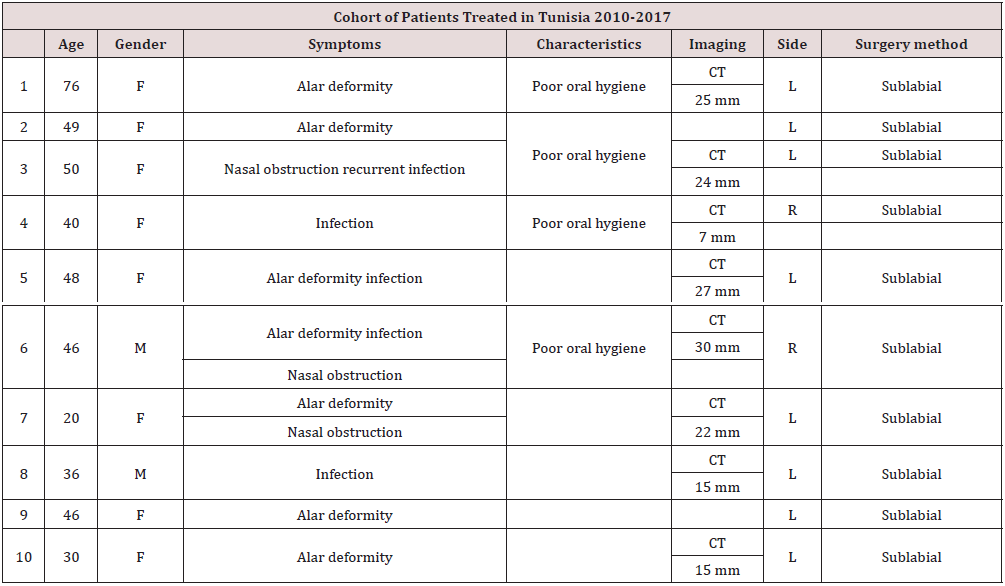
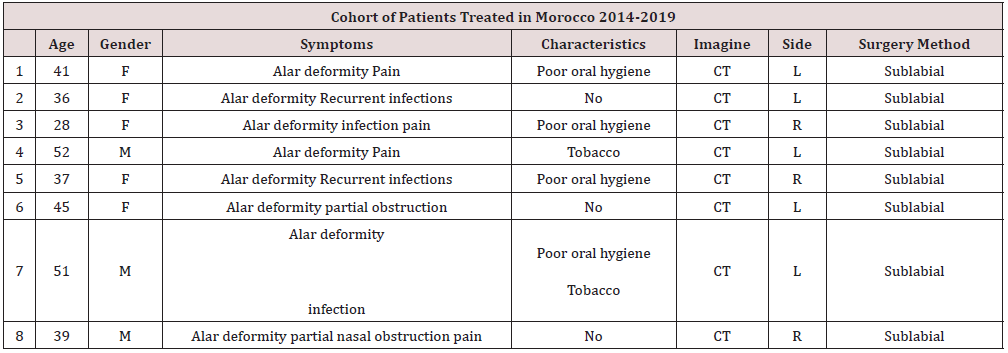
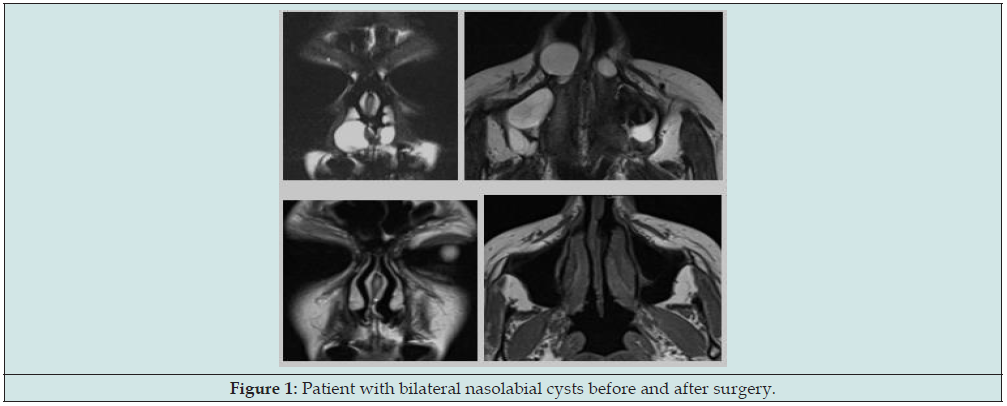
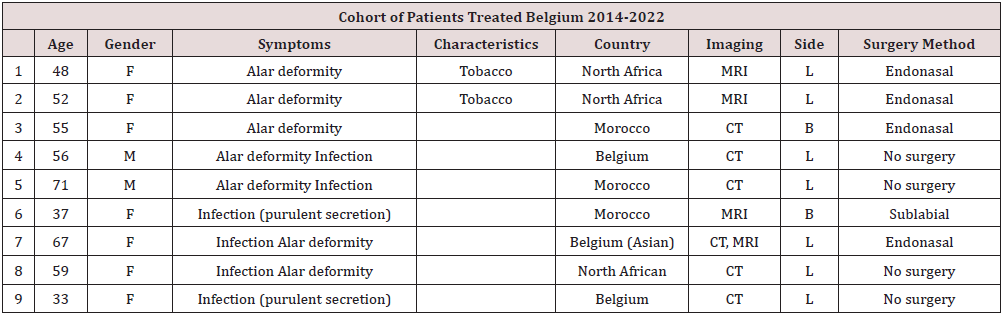
The case series includes 20 women and 7 men, the mean age at diagnosis was 44.7 with a range from 20 to 76 years old. Most patients are originally from North African countries, only 2 patients were Caucasian patients, and one patient was from Asian origin. The lesions were unilateral in 25 patients (19 left-sided; 6 rightsided) whereas 2 patients had bilateral cysts (Figure 1). Tobacco use and poor oral hygiene were recurrent characteristics in at least 10 patients (Tables 1-3). The diagnosis was made by both clinical examination and imaging; computed tomography (CT) was performed in 22 patients and magnetic resonance imaging (MRI) in 4 patients. Typically, alar deformity was noticed in 24 patients, with nasal obstruction being noticed in 6 of them and recurrent infections observed in 15 patients. In 4 cases the cysts were symptomatic due to bacterial infection and were asymptomatic after administration of systemic oral broad-spectrum antibiotics, these patients were monitored in consultation and no surgery was required. Surgery was performed via limited intraoral sublabial approach in 19 patients. Endoscopic transnasal marsupialization was performed in 4 patients in Belgium, 3 of these patients were operated transnasally with the microdebrider (Medtronic – tricut blade). All patients were asymptomatic upon a minimum follow-up at 6 months. Only one patient required additional surgery after 14 months.
Table 1: Cohort of patients treated in Belgium 2014-2022. (L=left, R=right, B=Bilateral, M=male, F=female, CT=computed tomography, MRI=magnetic resonance imaging.
Discussion
Nasolabial cysts also known as Klestadt’s cysts, are characterised by a respiratory epithelium and pseudostratified ciliated columnar epithelium with goblet cells [4]. Recently, a systematic review has been published and showed that nasolabial cysts occur most frequently in women (female to male ratio of 3.6:1), with a mean age of 41.8 years. In our series we found similar findings regarding epidemiologie [4]. According to our study, the most encountered symptoms were alar deformity and recurrent infections. However nasal obstruction was reported only in 6 patients. Our findings are consistent with the systematic review published in 2015, where the most common symptom mentioned was facial swelling, seen in 70% of the cases, and particularly nasolabial, alar and/or lip deformity. Another frequently encountered symptom is nasal obstruction. Recurrent infections of the cysts can occur; however, it is less common than facial swelling or nasal obstruction. Pain is not often associated with nasolabial cysts, nevertheless, the presence of pain could be a sign of infection [4]. In our series we noticed that almost half of the patients were heavy smokers and had poor oral hygiene, further studies are needed to show if these findings are associated with the development of nasolabial cysts. In our study, most of the patients presented their cysts on the left side, but some occurred bilaterally, as has been described in literature [4].
Nasolabial cysts are more prevalent amongst Asian and African American population [4], however our series shows a predominance among North African population. There is no clear explanation for this prevalence, however it is possible that the selection of patients is biased. There are different treatment methods described in the literature. As our case series shows, infected cysts can resolve after administration of systemic oral antibiotics. However, most of the cysts need a surgical treatment. The 2 most used surgical treatments are the sublabial approach and the transnasal approach. The sublabial approach is the most common which complete excision of the cysts is possible. However, most patients complain of facial swelling, tootache and facial numbness postoperatively. It can be performed under local or general Anesthesia. The recurrence of the cyst is rare with this technique [6]. The second most used treatment modality is the trans nasal marsupialization [5]. It is a faster and easier technique than the sublabial approach. The technique consists of marsupializing the cyst after incision of the cyst in the nasal cavity. Lee et al. compared the the sublabial and trans nasal approach and concluded that the transnasal approach is faster, has lower rates of pain and facial swelling and has in general lower complication rates [6]. It is characterized by less postoperative pain and a quicker rehabilitation immediately after the surgery. Futhermore, there is a lower complication rate with this approach. Therefore, the hospital stay is reduced [6]. However, the systematic review showed that both techniques have the same outcome and the recurrence after surgery is very low [4].
There are several tools you can use for the transnasal endoscopic approach. The technique in the Belgian Ear Nose and Throat departments is the microbrewer with the tricot blade (Medtronic) and has not been described yet in the literature. It consists of marsupial zing the cyst, opening the cyst in order to have a direct link with the nasal cavity and finally flattening the sides of the cysts to inhibit a possible recurrence (Figures 2 & 3). All patients underwent this surgery under general anesthesia. Until now, no complications or recurrence have been reported with this surgical technique. Recently, Zhang et al. presented a new technique in a prospective study which is the transnasal endoscopic marsupialization through Nd: YAG laser. The study shows that this method is effective and can be done under local anaesthesia [7].
Figure 2: Transnasal approach: debridement of the cyst after incision of the cyst with the Medtronic microbrewer.

Conclusion
Nasolabial cysts are non-odontogenic soft tissue masses located in the premaxillary region and which develop sub labially. They are particularly rare in Belgium and seem to be more common in North African countries. There is a female predominance. The diagnosis is made firstly by clinical examination, where symptoms such as facial swelling and alar deformity are the most prevalent symptoms, and secondly by imaging, where both CT and MRI are recommended. Two main treatment procedures are reported: the first and most common one is limited sublabial surgery, the second surgery modality is endoscopic transnasal marsupialization.
Acknowledgements
The authors declared no conflict of potential conflicts of interest with respect to the research, authorship, and publication of this article.
References
- Yuen HW, Julian CY, Samuel CL, (2007) Nasolabial cysts: clinical features, diagnosis, and treatment. Br J Oral Maxillofac Surg, 45(4): 293-297.
- Sahin C (2009) Nasolabial cyst. Case Rep Med 2009: 586201.
- Choi JH, Cho JH, Kang HJ, Chae SW, Lee SH, Hwang SJ, et al. (2002) Nasolabial cyst: a retrospective analysis of 18 cases. Ear Nose Throat J 81(2): 94-96.
- Sheikh AB, Chin OY, Fang CH, Liu JK, Baredes S, Eloy JA. (2016) Nasolabial cysts: A systematic review of 311 cases. Laryngoscope 126(1): 60-66.
- Su CY, Chien CY, Hwang CF. (1999) A new transnasal approach to endoscopic marsupialization of the nasolabial cyst. Laryngoscope 109(7 Pt 1): 1116-1118.
- Lee DH, Yoon TM, Lee JK, Lim SC (2020) Surgical treatment of nasolabial cysts in a single institute. J Laryngol Otol p. 1-4.
- Zhang J, Wu X, Ma J (2022) A new transnasal approach of Nd: YAG laser treating nasolabial cysts. Lasers Med Sci 37(2): 1321-1324.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...