Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Mini Review(ISSN: 2641-1709) 
Middle Ear Cholesteatoma: About 15 Cases Volume 7 - Issue 5
Lekassa P1*, Miloundja J1, Ella Ondo T2, Manfoumbi Ngoma AB1, Nzenze SAM1, Atsame Gonzalves A1, Mwanyombet L3 and Nzouba L1
- 1Department of ENT & CCF, Omar Bongo Ondimba Army Instruction Hospital, Gabon
- 2Department of Medical Imaging, Omar Bongo Ondimba Army Instruction Hospital, Gabon
- 3Department of Neurosurgery, Omar Bongo Ondimba Army Instruction Hospital, Gabon
Received: November 22, 2021; Published: December 10, 2021
Corresponding author: Lekassa Pierrette, Department of ENT & CCF, Omar Bongo Ondimba Army Instruction Hospital, Gabon
DOI: 10.32474/SJO.2021.07.000272
Summary
Aim: Cholesteatoma of the middle ear is a particularly aggressive form of chronic otitis media. The objective of this work was to
study the diagnostic, therapeutic and evolutionary aspects.
Materials and Method: This were a retrospective descriptive study conducted out in the ENT and CCF department of the
HIAOBO from the files of patients hospitalized for surgery for middle ear cholesteatoma, between January 2006 and December
2019.
Results: Fifteen patients were selected, including 7 men (ratio = 0, 87). The average age was 28.53 years with the extremes of 8
and 77 years. There were 11 adults and 4 children. The circumstances of discovery were purulent otorrhea (7 cases), a complication
(9 cases) including mastoiditis (4 cases), facial palsy (2 cases), cerebral abscess (1 case) and extra-Dural empyema associated with a
cerebellar abscess (1 case). The interrogation found hypoacusis in all cases an earache (10 cases) and headache (4 cases). Otoscopy
showed scales (7 cases), ACE polyp (4 cases), otorrhea (3 cases) and tympanic perforation of the shrapnel (1 case). CT scans of
the rocks suggested the diagnosis in all patients. Tympanoplasty was performed using the closed (8 cases) and open (7 cases)
technique. The associated procedures were drainage of abscesses and empyema (2 cases) and Ossiculoplasty (2 cases). The course
was marked by the presence of a residual cholesteatoma (6 cases).
Conclusion: Cholesteatoma is a serious pathology that can engage the functional and vital prognosis. Its treatment is surgical.
Keywords: Cholesteatoma; middle ear; computed tomography; tympanoplasty
Introduction
Middle ear cholesteatoma is defined by the presence in the cavities of the middle ear of a keratinized squamous epithelium with the potential for desquamation, migration and erosion [1,2]. It is dangerous and serious because of its progressive and extensive risks and its complications which can be life-threatening [1,2]. A rock scan is the gold standard that shows the extent of the cholesteatoma and its possible complications. Magnetic resonance imaging (MRI), on the other hand, plays a key role in the detection of postoperative recurrences. The recent use of otendoscopy and MRI makes it possible to better identify the extensions of cholesteatoma before and after surgery. The objective of this work was to study the diagnostic, therapeutic and evolutionary aspects of chronic cholesteatomata’s otitis media.
Materials and Methods
This was a retrospective study of the records of patients hospitalized for the management of chronic cholesteatomatous otitis media, in the ENT and CCF department of the HIAOBO between January 2006 and December 2019. The data collection was carried out using an exploitation sheet or were reported the data, clinical, para-clinical including the audiogram, the tomodensitometry of the rocks, the imaging by magnetic resonance as well as therapeutic and evolutionary data. The parameters studied were age, sex, ontological history, clinical history, and clinical and paraclinical signs. We included the charts of patients with chronic cholesteatomatous otitis media and excluded chronic non-cholesteatomatous otitis media and cholesteatoma of the external auditory canal from this study.
Results
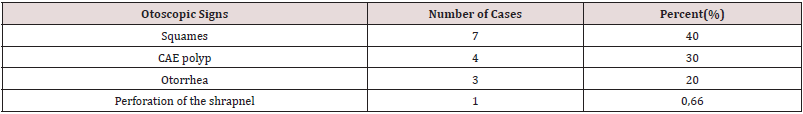
Fifteen patients were selected. These were 7 males and 8 females, with a sex-ratio of 0 87. The average age was 28.53 years with the extremes of 8 and 77 years. There were 11 adults and 4 children. The circumstances of discovery were purulent otorrhea in 7 cases, a complication in 9 cases including 6 extracranial complications including mastoiditis in 4 cases, facial palsy in 2 cases and 3 intracranial complications including a brain abscess (1 case), 1 Cerebellar abscess (1 case) associated with extra-dural empyema in 1 case. The history found was recurrent otitis in 7 cases, myringoplasty in 2 cases and trisomy 21 in 1 case. The functional signs were purulent fetid otorrhea associated with hypoacusis in all cases, earache in 10 cases (67%) and headache in 4 cases (26%). Otoscopic examination showed results reported in Table 1. The audiogram was performed preoperatively in all patients and demonstrated conductive hearing loss with a preoperative mean tonal threshold of 50 decibels and an average audiometric Rinne of 20 decibels.
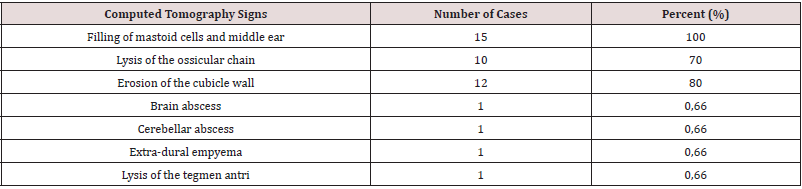
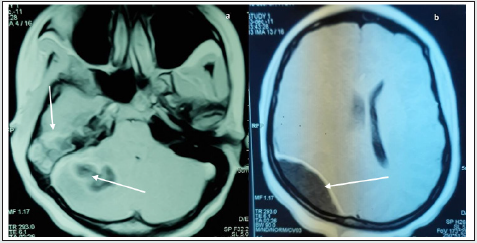
The computed tomography of the rocks carried out in all the patients preoperatively showed a filling of the middle ear and mastoid cells in all the patients, a partial or complete lysis of the ossicular chain in 10 cases (70%), an erosion of the wall cubicle in 12 cases (80%), a cerebral abscess in one case and a cerebellar abscess associated with an extradural empyema in one case, and lysis of the antri tegmen (Figure 1). The results of the tomodensitometry are reported in (Table 2). The contralateral ear was pathological in 3 cases with a type of tympanic perforation and normal in 12 cases. MRI was performed in 2 cases and confirmed the CT results by showing 1 brain abscess in 1 case and extra dural empyema associated with right cerebellar abscess in the other case (Figure 2). Tympanoplasty was performed in a closed technique in 8 patients (53%). It consisted of performing a masto-antroatticotomy with reconstruction of the eardrum and the atticotomy by the tragian cartilage. Open technique tympanoplasty with sacrifice of the bony ear canal with or without posterior filling was performed in 7 patients (47%). Trepanation followed by fine needle aspiration was performed for extra-dural empyema associated with cerebellar abscess and craniotomy for cerebral abscess. Broad-spectrum antibiotic therapy, corticosteroid therapy and an anticonvulsant have been combined. All of the pus samples were sterile, and the pathological examination of the tissues collected during the operation was in favor of cholesteatoma all patients. Postoperatively, an audiogram was performed in 11 cases (73%) and demonstrated conductive hearing loss with an average tonal threshold of 40 decibels and an average audiometric Rinne of 20 decibels. The evolution was marked by recurrence in 6 cases (40%), including 5 cases operated on by the open technique and 1 case operated on by the closed technique. Otoscopy showed a whitish bead on the hypotympanum in 5 cases operated on by the open technique and scales on the neotympanum in 1 case operated on the closed technique. CT of the rock was performed postoperatively in 8 patients (53%) within 12 to 18 months. It demonstrated total filling of the mastoid and nodular recess cavity of the attic and the mesotympanic membrane with bone lysis by cholesteatoma in 5 cases (Figure 3). All these patients were re-operated (2nd look) after 55 months with the extremes of 18 months and 7 years. Type II ossiculoplasty was performed in 2 cases operated in the closed technique, including 1 case using an anvil transposition but without improvement of hearing, and one case using cartilage, with improvement of l ‘hearing.
Figure 1: Coronal CT scan of the left rock: total filling of the eardrum and CAE with bluntness of the wall of the cubicle (arrow) analysis of the ossicles.
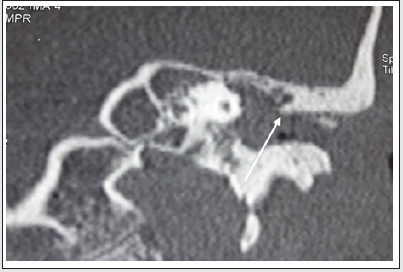
Figure 2: Axial T1- weighted brain MRI after gadolinium injection
a) Abscess of the right cerebellar hemisphere in T1 hypo-signal enhanced by peripheral cockade and right mastoid filling
(arrows)
b) Hypointense biconvex right extra-dural parieto-occipital empyema in T1 with peripheral enhancement (arrow).
Discussion
Middle ear cholesteatoma is a particularly aggressive chronic
otitis media, characterized by the presence in middle ear cavities
of a keratinizing squamous epithelium with a triple potential for
desquamation, migration and erosion. Its etiopathogenesis is poorly
understood. Two entities are described. Congenital or primary
cholesteatoma which is the prerogative of children, and which is
rarer. It corresponds to the absence of resorption of embryonic
epidermal cells and initially develops behind a normal eardrum.
The more common acquired cholesteatoma whose pathogenesis is
dominated by the theory of epidermal migration through the edges
of a marginal perforation or from a ruptured tympanic retraction
pocket, with the appearance of acute and chronic inflammatory
lesions [3]. The average age for some authors is between 35 and
43 years old [4,5]. In our study the mean age was 28.83 years,
our results are lower than those of Bouaty and Sethom [4,5]. The
distribution by sex is very variable [6,7]. However, in our study, the
female sex is slightly in the majority. The functional signs which are
also the most common reasons for consultation are fetid otorrhea
and hypoacusis [1,8]. Similar results are found in all the patients
in our study. Sometimes it is a complication such as dizziness,
facial paralysis, retroauricular skin fistulization or neurological
signs that reveal cholesteatoma [1,4]. Bouaity et al. report 20%
of complications comprising 20 cases (13.8%) of mastoiditis, 6
cases (4.1%) of facial paralysis and 3 cases (2%) of labyrinthitis
(2%) [4]. In our study, the complications that led to the diagnosis
of cholesteatoma were mastoiditis, facial palsy, brain abscess and
extra-dural empyema. Rarely, the finding is accidental during
otoscopic examination, medical imaging, or surgery on the middle
ear [5].
Cholesteatomatous otitis is often marked by a long history of
otitis and middle ear surgery. Dulos reports 89.6% respectively
[9], while Bouaity reports 18% of a history of ear infections also
tympanoplakia for cholesteatoma in 32 cases (22%) [4]. A history
of otitis and myringoplasty was found in our study in 47% and 13%
of cases. Trisomy 21 was found in 1 case. Otoscopic examination
is the key to diagnosis in the majority of cases [1]. It is performed
in our context under a microscope after aspiration, followed if
necessary by an otendoscopic examination. The diagnosis of
cholesteatoma is confirmed by the presence in the middle ear of
emerging epidermal scales, a marginal perforation or a pocket of
tympanic retraction. Bouaity et al. report marginal perforation in
(60%) of cases and attical perforation in 20.7% of cases [4]. Sethom
et al. report 8% of cases of external auditory canal polyp (EAC) [5]. Audiometry most often results in conductive hearing loss secondary
to the inflammatory reaction or tympano-ossicular destruction in
advanced forms [8,10]. It can also show mixed deafness or cophosis
[1]. Sometimes hearing is normal due to the columellar effect of the
cholesteatoma, who after having destroyed the ossicles replaces
them. In our study, the tonal audiogram performed preoperatively
showed conductive hearing loss of 50 decibels on average with an
audiometric Rinne of 25 decibels on average. Computed tomography
of rocks in bone windows is the gold standard for studying the
middle ear, especially in cholesteatomatous otitis before and after
surgery [2,11-14].
Preoperatively, this examination makes it possible to carry
out a precise lesion assessment, to look for certain complications
and to orient the operative strategy by highlighting the anatomical
particularities [1,3,11,13]. In rare cases, it can be used to confirm
the diagnosis when the otoscopy is not helpful in order to allow
a comparative analysis. This systematically recommended
examination was carried out in all the patients in our study on
the 2 ears in axial and coronal slices. The CT signs suggestive of
cholesteatoma are the presence of a tissue mass in the tympanomastoid
cavities and one or more areas of osteolysis, at the level
of the ossicular chain and the wall of the cubicle. The extension
of osteolysis to the tegmen, facial canal, labyrinth and lateral
semicircular canal is evidence of complications of cholesteatoma
[4,15]. Bouaity et al. report partial or total destruction of the
ossicular chain in 81% of cases and erosion of the cubicle wall in
62% of cases [4]. Sethom et al. report erosion of the cubicle wall in
62% of cases, filling of mastoid cells in 35% of cases and ossicular
lysis in 81% of cases [5]. Postoperatively, the scanner makes it
possible to identify recurrences. It is possibly supplemented by MRI
in late acquisitions after injection of gadolinium in T1-weighted
sequence supplemented by diffusion sequences to differentiate
between cholesteatomatous recurrence and residual inflammatory
change [16]. MRI is sometimes essential for the diagnosis of residual
in the case of a closed technique with cartilaginous eardrum and
the assessment of the extension of encephalic complications. The
treatment of cholesteatomatous otitis media is surgical. Its objective
is firstly to eradicate cholesteatoma and its matrix, secondly to
restore or improve hearing [4,17-19].
There are typically two types of interventions. The closed
technique tympanoplasty consists of a masto-antro-atticotomy
associated with a posterior and / or superior tympanotomy. It
preserves the facial wall, restores normal anatomy of the middle
ear and the external auditory canal. It preserves adequate hearing
and relieves post-operative care problems, but exposes the risk
of recurrence [9,18-20]. Duclos et al. report performing a closed
technique in 85% of cases [9]; Drahy et al. report 82% of cases
[19] and Touaty et al. perform it in all their patients [21]. In our
study this technique was used the most. Tympanoplasty in the open
technique, with or without posterior filling, makes it possible to
perform the removal of the cholesteatoma, to definitively exclude
the posterior mastoid cavities and the epitympanum by a muscle,
cartilage or bone filling and to perform a large meatoplasty to lead
to a functional petty cash and a stable ear [1]. It confers a new
anatomo-physiological status of the ear in order to modify the local
conditions, which gave rise to cholesteatoma [4]. It also allows
the creation of a large cavity and allows drying and stabilization
of unstable cavities. This open technique is indicated in cases of
small mastoid, low cellularity or meningeal prolapse. It is also
indicated when the “2nd look” is not possible and in the event of the
impossibility of a rigorous follow-up as in our study or in the event
of recurrence. However, it is complicated by otorrheic episodes
and makes fitting difficult. In many studies this technology is little
used [9,19-21]. Currently, the indication of a second operative
step is no longer systematic due firstly to the intraoperative use of
otovideo-endoscopy, which improves the vision and the quality of
the removal of the cholesteatoma or of a pocket. of retraction in
regions difficult to access, in particular the tympani sinus and the
anterior attic; and secondly, the advent of CT of rocks in millimeter
sections and diffusion MRI which allow quality radiological
monitoring [4,20,22]. When the 2nd look is indicated, it is done
between the 12th and 18th month. Duclos et al. achieved 75% of a
second look after 18 months of the initial procedure [9]. It makes
it possible to ensure the absence of recurrence and to perform a
possible ossiculoplasty [1]. In our study, this second operative step
was performed in 7 cases (46%) after 24 months.
The rehabilitation of hearing in cholesteatoma surgery, calls
upon the different types of ossiculoplasty, carried out from the first
operative stage if the mucosa is healthy, either using autologous
material (cartilage, anvil), or with the using ossicular prostheses.
Where appropriate, conventional or bone-anchored hearing aids
are used [4]. Drahy et al. report 86% of ossiculoplasty including
18% during the first phase and 61% by autologous materia l [19].
Bouhafs et al. report 26 type II ossiculoplasty in 30 patients in their
series [23]. In our experience, type II ossiculoplasty was performed
in 2 cases, including 1 case with the anvil and 1 case with anvil
cartilage and cartilage. Hearing was not improved in the first case,
possibly due to the presence of an inflammatory and scarring
process. The postoperative course is marked by the appearance of
residuals, which represent the real problem with cholesteatoma
surgery. In the studies by Duclos and Mutlu, the residual rates were
32% and 38% respectively [9,24]. Triglia et al. report 41% residual
during the 2nd look [8]. In our series, cholesteatoma was found in
40% of cases during the 2nd look, including 5 cases operated on
in the open technique and 1 case in the closed technique, unlike
Bouaity who reported 25% in patients operated on by the closed
technique and 13, 4% in patients operated on by the open technique
[4]. Long-term monitoring must be an integral part of therapeutic
management regardless of the technique chosen. It makes it
possible to detect residual cholesteatomas and recurrences.
Conclusion: Cholesteatoma of the middle ear is a fairly common
pathology in our context, but serious due to its complications.
The pre and post operative scanner is essential. Its treatment
is only surgical by tympanoplasty in closed or open technique.
Ossiculoplasty, when possible, improves hearing.
References
- Ayache D, Schmerber S, Laveieille JP, Roger G, Gratacap B (2006) Cholestéatome de l’oreille moyenne. Ann Otolaryngol Chir Cervicofac 123(3): 120-137.
- Zylberg F, Williams M, Ayache D, Piekarski JD (2000) Computed tomography of secondary cholesteatoma of the middle ear. Radiol leaflets 40(1): 48-57.
- Tran Ba Huy P (2005) Chronic otitis media, Elementary history and clinical forms. In. EMC-otorhinolaryngology 2(1): 1-25.
- Bouaity B, Chihani M, Nadour K, Moujahid M, Touati M, et al. (2014) Middle ear cholesteatoma. Retrospective study of 145 cases. Pan Afr Med J 17: 163.
- Sethom A, Akkari K, Dridi I, Tmimi S, Mardassi A, et al. (2011) Contribution of CT in the preoperative assessment of cholesteatomatous OMC: About 60 cases. Tunis med 89(3): 248-253.
- Gaillardin L, Lescanne E, Morinière S, Robier A (2012) Canal wall up tympanoplasty for middle ear cholesteatoma in adults: modeling cartilage. Eur Ann Otorynolaryngol Head Neck dis 129(2): 82-86.
- Tall A (2010) Medium-term follow-up of petromastoid cavities performed for cholesteatoma of the middle ear. Ann Fr Otorhinolaryngol Pathol Cervicofac 127: 97-148.
- Triglia JM, Gillot JC, Giovanni A, Cannoni M, Narcy P (1993) Cholesteatoma of the middle ear in children: about 80 observations and review of the literature. Ann Otolaryngol Chir Cervicofac 110(8): 437-443.
- El Jerrari A, Charles X, Gentine A, Contraux C (1995) Cholesteatoma in Children: Report of 110 Cases. Ann Otolaryngol Chir Cervicofac 112(6): 251-257.
- Duclos JY, Darrouzet V, Portmann D, Portman M, Bébéar JP (1999) Congenital middle ear cholesteatoma in children: Clinical, evolutionary and therapeutic analysis of a series of 34 cases. Ann Otolaryngol Chir Cervicofac 116: 218-227.
- Williams MT, Ayache D (2006) Imaging of chronic ear infections in adults. J Radiol 87: 1743-1755.
- Yates PD, Flood LM, Banerjee A (2002) CT scanning of middle ear cholesteatoma: what does the surgeon want to know? Br J Radiol 75: 847-852.
- Blevins NH, Carter BL (1998) Clinical forum-routine preoperative imaging in chronic ear surgery. Am J Otol 19: 527-538.
- Gerami H, Naghavi E, Wahabi-Moghadam M (2009) Comparison of preoperative computerized tomography scan of temporal bone with intra-operative findings in patients undergoing mastoidectomy. Saudi Med J 30: 104-108.
- Ayache D, Darrouzet V, Dubrulle F, Vincent C, Bobin S (2012) Imaging of unoperated cholesteatoma. Recommendation for clinical practice. Ann Fr Otorhinolaryngol Pathol Cervicofac 129: 177-181.
- De Foer B, Vercrysse JP, Pouillon M, Somers T, Casselman JW, et al. (2007) Value of high-resolution computed tomography and magnetic resonance imaging in the detection of residual cholesteatomas in primary bony obliterated mastoids. Am J Otolaryngol 28(4): 230-234.
- Matlu C, Khashaba A, Saheh E (1993) Surgical treatment of cholesteatoma in children. Otolaryngol Head Neck Surg 113(1): 56-60.
- Charachon R, Schemerber S, Lavieille JP. La chirurgie des cholestéatomes de l’oreille moyenne. Ann Otolaryngol Chir Cervicofac 1999; 116(6): 322-340.
- Nevoux J, Lenoir M, Roger G, Denoyelle F, et al. Le cholestéatome chez l’enfant. Ann Fr Otorhinolaryngol Pathol Cervicofac 2010; 127: 182-190.
- Drahy A, De Barros A, Lerosey Y, Choussy O, Dehesdin D, Marie JP. Cholestéatome acquis de l’enfant: stratégies et résultats à moyen terme. Ann Fr Otorhinolaryngol Pathol Cervicofac 2012; 129: 269-273.
- Touati M M, Darouassi Y, Chihani M, Bouaity B, Ammar H. L’otite moyenne chronique cholestéatomateuse de l’enfant: à propos de 30 cas. Pan Afr Med J 2015; 21: 24.
- Gaillardin L, Lescanne E, Morinière S, Cottier J P, Robier A. Le cholestéatome résiduel: prévalence, localisation. Stratégie de surveillance chez l’adulte. Ann Fr Otorhinolaryngol Pathol Cervicofac 2012; 129: 165-169.
- Bouhafs K, Lachkar A, Benallal A, Benfadil D, Ghailan MR. Ossiculoplastie: à propos de 30 cas et revue de la littérature. Pan Afr Méd J 2021; 38: 187.
- Mutlu C, Khashaba A, Saleh E et al. Surgical treatment of cholesteatoma in children. Otolaryngol Head Neck Surg 1995; 113: 56-60.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...