Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Research Article(ISSN: 2641-1709) 
Lingual Thyroid Gland: As A Rare Case Presentation Volume 8 - Issue 1
Khaled Mohamed Bofares*
- Professor, Department of Otorhinolaryngology, Omar Almoukhtar University, Libya
Received: March 15, 2022; Published: March 24, 2022
Corresponding author: Khaled Mohamed Bofares, Professor, Department of Otorhinolaryngology, Omar Almoukhtar University, Elbyda, Libya
DOI: 10.32474/SJO.2022.08.000280
Abstract
Lingual thyroid (LT) gland is a rare clinical entity which was found to occur due to the failure of the thyroid gland to descend to its normal cervical location during embryogenesis. The presence of an ectopic thyroid gland located at the base of the tongue may present with symptoms like dysphagia, dysphonia, upper airway obstruction or even hemorrhage at any time from infancy through adulthood.
Keywords: Lingual thyroid; ectopic thyroid
Introduction
The thyroid gland is one of the largest endocrine glands in the body, it lies approximately the same level as the cricoid cartilage [1,2]. Ectopic thyroid tissue has been found from the tongue to the diaphragm. Ninety percent of the reported cases of ectopic thyroid are found in the base of the tongue [3,4] .Lingual thyroid is a rare developmental thyroid anomaly, caused by the failure of the gland to descend from its anlage, early in the course of embryogenesis. It generally originates from epithelial tissue of nonobliterated thyroglossal duct [5-9]. Prevalence rates of LT vary from 1 in 100,000 to 1 in 300,000, with females to male ratio ranging from 4:1 to 7:1 [10-12]. Ectopic thyroid is a rare embryological aberration which can occur in any moment of the migration of the thyroid resulting in lingual (at tongue base), sublingual (below the tongue), prelaryngeal (in front of the larynx), and substernal (in the mediastinum) ectopy. Dual ectopic thyroid has been described [1- 10], even with the thyroid gland in a normal location [11]. It occurs more frequently in females, with a female to male ratio 4:1; ectopic thyroid is seen at any age but more commonly during childhood, adolescence and around menopause. This probably occurs when demands for thyroid hormones increase, causing the increase in circulating TSH levels with growth of the ectopic thyroid tissue [6-12]. About 33-62% of all patients with ectopic thyroid showed hypothyroidism with increased levels of TSH [5-13].
Most ectopic thyroids are asymptomatic, and no therapy is necessary. Symptoms are related to the growth of the thyroid tissue, causing dysphagia, dysphonia with stomatolalia, bleeding or dyspnoea 4– 14– 15. The enlarged lingual thyroid has been described as a cause of difficult intubation during induction of anaesthesia, especially for bleeding [10–14]. Clinically, lingual thyroid presents as a mass at the base of the tongue, pink and firm. The most important diagnostic tool is thyroid scan with technetium Tc-99m sodium, but use of CT and magnetic resonance imaging (MRI) may help in defining the extension and location of the ectopic thyroid gland. Thyroid scan can also reveal whether there are other sites of thyroid tissue; in approximately 75% of patients the ectopic tissue is the only functioning thyroid tissue in the body [15,16]. Therefore, it is important to observe the patient at follow-up, being aware of the risk of post-operative hypothyroidism. Differential diagnosis includes lymphangioma, minor salivary gland tumours, midline branchial cysts, thyroglossal duct cysts, epidermal and sebaceous cysts, angioma, adenoma, fibroma and lipoma [5-10]. Management of lingual thyroid is still controversial. No treatment is required when the lingual thyroid is asymptomatic, and the patient is in an euthyroid state; the patient has to be followed to be aware of development of complications. Malignant transformation has been described [17-24] and, for this reason, some Authors consider complete surgical removal of the gland as appropriate treatment 17 24. For patients with no, or only mild, clinical symptoms and elevated TSH concentration, substitutive therapy with thyroid hormone may be successful, producing a slow reduction of the mass.
Ablative radioiodine therapy is an alternative approach recommended in older patients or patients who are deemed unfit for surgery. This treatment should be avoided in children and young adults since the systemic doses required have potentially damaging effects on the gonads or other organs [25-28]. Moreover, the thyroid tissue is often hypoactive, and the dose of radioiodine required is generally high [26-28]. When medical therapy fails, and in symptomatic or complicated cases, surgery is the treatment of choice. In the literature, several surgical approaches have been described, including surgical removal of the mass with external approaches, such as by trans-hyoid or lateral pharyngotomy, or performing trans-oral ablation of the mass. The trans-oral approach seems to avoid injury to the deep neck structures with possible complications (such as injury of the lingual nerve, fistula formation, deep cervical infection and visible scar) and should be considered as possible treatment for a small mass, while external approaches with temporary tracheotomy can probably better control bleeding and are recommended for bulky masses.
For the trans-oral approach, cold instruments with mono-polar coagulation and laser CO2 have been used and laser diode can also be useful. The possibility that the ectopic thyroid tissue could be the only functioning tissue must be considered; in those cases, some Authors recommend transplantation of the excised ectopic tissue [26-28], in order to avoid permanent hypothyroidism [4].
In alternative, substitutive hormone treatment could be started to preserve the euthyroid state. Transplantation is not necessary in cases of partial surgical eradication, while substitutive therapy could be necessary to preserve euthyroid state and avoid recurrence of the mass. In our opinion, the general conditions of the patient, the size of the lesion and presence of local symptoms or complications, such as haemorrhage, cystic degeneration or malignancies, are the most important conditions for planning the choice of treatment. In symptomatic, older patients, unfit to undergo more aggressive surgical approaches, or in small and anterior lesions, partial trans-oral ablation could be recommended; the partial trans-oral approach is less aggressive but cannot prevent malignant transformation and possible relapse, moreover, allows less control as far as concerns bleeding during surgery. In younger patients, or in the case of large lesions, or lesions deeply located in the caudal part of the base of the tongue, total ablation could be the most appropriate choice: in this case, transplantation of the thyroid tissue is, in our opinion, not necessary while substitutive hormone treatment is recommended as following other radical surgical approaches for normal thyroid gland. Special care should be taken to ensure airway patency; this can usually be achieved by temporary tracheostomy or maintaining the naso-tracheal tube for the first 24 hours after surgery. Tracheostomy or intubation should not be removed until haemostasis and airway patency have been confirmed. In trans-oral approaches, soft diet is usually tolerated sooner than in external approaches [1, 4,14].
Case Presentation
Case history
44 years female Libyan patient from DARNA city- Libya presented to ENT OPD with history of mass at posterior part of tongue since childhood. The mass was very slowly progressing in size. Recently with big sized mass the patient started to C\O frequent attacks of dysphagia as well as air-way obstruction particularly when the patient lying down during deep sleep. On 1989 (at age 18 years), the patient under-went punch biopsy from the mass under general anesthesia (GA) at AL-HAWARI hospital- Benghazi city- Libya and the histopathology confirmed the results as thyroid tissue. From that time, the excisional biopsy was postponed because of three reasons:
a) The patient proved that had no evidence of cervical thyroid tissue and only the acting thyroid tissue is that lingual one,
b) The mass was not of big size that may cause related symptomology, and
c) The patient was eu-thyroid.
The patient had not another significant history apart of the documents from TUNISIA which shown by the patient and were including iodine isotope scanning which elucidated that the mass was active thyroid tissue.
On examination
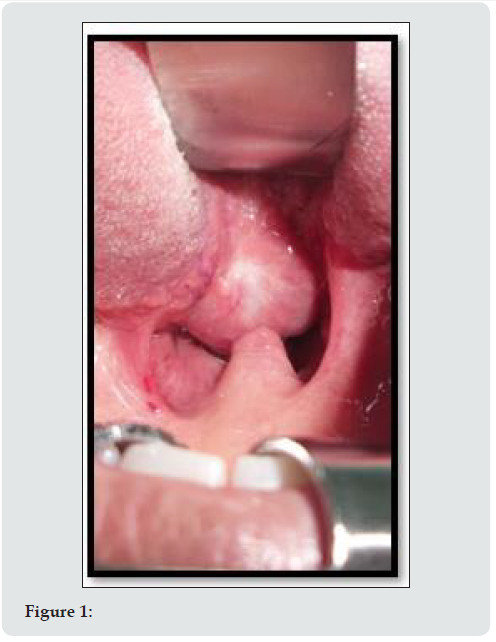
There was evidence of big lump (3cm×4cm) oval in shape, raised from posterior third of tongue and occupying partially the oropharynx, the palatine tonsils, posterior pillars, as well as posterior pharyngeal wall cannot completely be seen. The mass is flashy in its appearance with prominence of high vascularity, and it has smooth surface with obvious capsule which can be differentiated from lingual tissue.
Investigations
a) Thyroid function test (TFT) was normal.
b) USS neck confirmed absence of thyroid tissue.
c) MRI neck confirmed the origin and extension of the mass up to area of the valeculae. In addition to the absence of cervical thyroid tissue.
d) S.Ca and S.Mg was normal.
Further
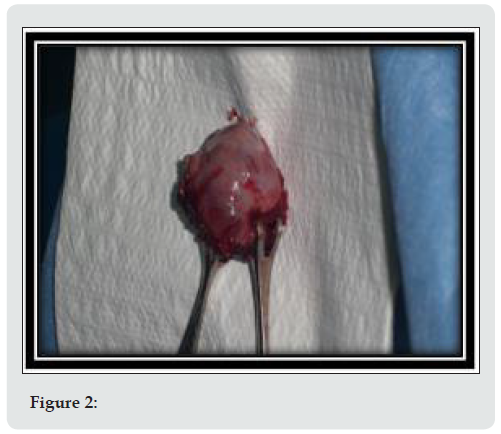
Patient decided for excision of mass which done on 7\May\ 2015 under G.A and NTI performing the excision using electrodiathermy dissection. The specimen sent for histopathological evaluation (H\P). Patient discharged at third postoperative day (POD) in good conditions on L-thyroxine 100mg once a day and advised for follow-up which done after one week from discharge (10th POD) and she was well. The H\P results came and confirm the finding of active follicular thyroid tissue. Patient advised for repeating TFT after 6 weeks.
Discussion
Lingual thyroid is a rare developmental anomaly originating from aberrant embryogenesis during the passage of the thyroid gland through the neck. Embryonic development begins about 24 days after fertilization in the floor of the primitive hypopharynx from median endodermal thickening, then the primitive gland descends closely related to the hyoid bone and laryngeal cartilages [20-28]. The thyroglossal duct is a narrow tube connecting the developing thyroid gland to the tongue and it usually involutes at the sixth or eighth week. The foramen caecum is the opening of the thyroglossal duct in the tongue. The thyroid gland then descends to meet the lateral ultimo-branchial bodies; the fusion of these elements leads to the formation of the functional and mature thyroid gland by the third foetal month [1-28]. Lingual thyroid is the most frequent ectopic location of the thyroid gland, although its prevalence varies between 1:100000 and 1:300000 and its clinical incidence is reported to range from 1:4000 to 1:10000. The true incidence is probably underestimated: some Authors reported having found ectopic lingual tissue in 10% of 200 consecutive necropsies [20-28]. In the literature, approximately 400 cases of symptomatic patients have been reported [10-28].
Ectopic thyroid tissue can also occur between the genio-hyoid and mylohyoid muscles (sublingual thyroid), above the hyoid bone (pre-laryngeal thyroid) and in other rare sites such as the mediastinum, precardial sac, heart, breast, pharynx, oesophagus, trachea, lung, duodenum and mesentery of the small intestine, adrenal gland [10-28]. Hickmann recorded the first case of lingual thyroid in 1869. Montgomery stressed that for a condition to be branded as lingual thyroid, thyroid follicles should be demonstrated histopathologically in tissues sampled from the lesion [4]. A brief discussion of embryology of thyroid gland would ensure better understanding of the pathophysiology involved in the formation of ectopic thyroid gland. Early in embryogenesis, thyroid gland appears as proliferation of endodermal tissue in the floor of the pharynx between tuberculum impar and hypobranchial eminence (this area is the later foramen caecum) [1-28]. Normally thyroid gland descends along a path from foramen cecum in the tongue, passes the hyoid bone, to the final position in front and lateral to the second, third, and fourth tracheal rings by 7 weeks gestation. During this descent thyroid tissue retains its communication with foramen cecum. This communication is known as thyroglossal duct. Once the thyroid reaches its final destination, the thyroglossal duct degenerate [1-28]. Persistence of thyroglossal duct even after birth leads to the formation of thyroglossal cyst. These cysts usually arise from the remnants of thyroglossal duct and can be found anywhere along the migration site of thyroid gland. This descent may arrest anywhere along this path and this condition may remain unnoticed until puberty. Any functioning thyroid tissue found outside of the normal thyroid location is termed ectopic thyroid tissue [10-28]. Although it is usually found along the normal path of development, ectopic tissue has also been noted in the mediastinum, heart, esophagus, and diaphragm. Lingual thyroid is the result of failure of descent of the thyroid anlage from the foramen cecum of the tongue. The reasons for the failure of descent are unknown [26-28].
The incidence of LT is reported as 1:100,000. It is 7 times higher in females [10]. Clinical presentations are varied, most of them related to oropharyngeal obstruction, and may include dysphagia (mild or severe), dyspnea and dysphonia, fullness in the throat, sleep apnoea. Stridor is most common in neonates [26-28]. About 33% of the patients show hypothyroidism findings [26-28]. Bleeding is rarely described. The clinical presentation of LT could be classified into two groups according to the appearance of the symptoms: infants and young children whose lingual thyroid is detected via routine screening may suffer from failure to thrive and mental retardation, or even severe respiratory distress, resulting in a medical emergency [26-28]. Other cases may present with onset of slowly progressing dysphagia and symptoms of oropharyngeal obstruction before or during puberty. This occurs as a response to the increased demand for thyroid hormone in these hyper-metabolic states. Similar response is also encountered during other metabolic stress conditions like pregnancy, infections, trauma, menopause, etc. [28]. LT usually presents itself as a midline, nodular mass in the base of the tongue [28]. The surface of the lesion is usually smooth, and vascularity can be seen. This was the case in our patient. Thorough head and neck examination with special attention to the base of the tongue is mandatory. Palpation of the neck is extremely essential, in order to check the presence or the absence of the thyroid gland in its normal position. Investigations include thyroid function tests (often demonstrate normal gland functions). Technetium scanning confirms the presence of ectopic thyroid tissue at the base of tongue. There was no normal thyroid gland on scintigraphy and radiological examinations in our case. Histologically, on FNA, LT resembles normal thyroid tissue. Unless emergency surgery is indicated, suppressive therapy with exogenous thyroid hormone should be tried first in order to decrease the size of the gland. This was the case in our patient and elective surgery following the suppression therapy was planned. Additionally, levothyroxine therapy should be initiated after surgical excision as the lingual thyroid is the only functioning thyroid tissue found in 70% of these patients [28].
Conclusion
Lingual thyroid is a rare anomaly representing faulty migration of normal thyroid gland. The exact pathogenesis of this ectopic is not known. It is 7 times higher in females. Lingual ectopic thyroid is a rare developmental anomaly, the treatment of which is still controversial because of the rarity of the condition. Treatment could be conservative with substitutive hormone treatment in patients with mild symptoms, while surgery is recommended in cases with airway obstruction. Evaluation of thyroid function is recommended before and after surgery due to the risk of postoperative hypothyroidism. Dysphagia and dysphonia are common presenting symptoms. Thorough head and neck examination with special attention to base of tongue is essential. Investigation includes thyroid function tests, neck ultrasound scan, Technetium scanning and C.T scan. FNAC is not preferred by some authors as it would cause unnecessary bleeding. Although different types of surgical access have been described, the transoral approach provides good exposure and is less traumatic for the patient, with better postoperative recovery. When complications such as dysphagia or dyspnea occur, surgery is necessary: the trans-oral approach can be useful, in selected cases (older patients or anterior and small masses), while in younger patients, usually the external approach is the best choice due to the risk of malignant transformation, relapse and for better bleeding control. Transplantation is not recommended, but substitutive hormone treatment is often needed. Follow-up is recommended to monitor possible recurrence or complications.
References
- Ulug T, Ulubil SA, Alagol F (2003) Dual ectopic thyroid: report of a case. J Laryngol Otol 117: 574-576.
- Chanin LR, Greenberg LM (1988) Pediatric upper airway obstruction due to ectopic thyroid: classification and case reports. Laryngoscope 98: 422-427.
- Sauk JJ (1970) Ectopic lingual thyroid. J Pathol 102: 239-243.
- Gallo A, Leonetti F, Torri E, Manciocco V, Simonelli M, et al. (2001) Ectopic lingual thyroid as unusual cause of severe dysphagia. Dysphagia 16: 220-223.
- Di Benedetto V (1997) Ectopic thyroid gland in the submandibular region simulating a thyroglossal duct cyst: a case report. J Pediatr Surg 32: 1745-1746.
- Kumar R, Sharma S, Marwah A, Moorthy D, Dhanwal D, et al. (2001) Ectopic goiter masquerading as submandibular gland swelling: a case report and review of the literature. Clin Nucl Med 26: 306-309.
- Pollice L, Caruso G (1986) Struma cordis. Ectopic thyroid goiter in the right ventricle. Arch Pathol Lab Med 110: 452-453.
- Porqueddu M, Antona C, Polvani G, Cavoretto D, Pompilio G, et al. (1995) Ectopic thyroid tissue in the ventricular outflow tract: embryologic implications. Cardiology 86: 524-526.
- Ferlito A, Giarelli L, Silvestri F (1988) Intratracheal thyroid. J Laryngol Otol 102: 95-96.
- Hazarika P, Siddiqui SA, Pujary K, Shah P, Nayak DR, et al. (1998) Dual ectopic thyroid: a report of two cases. J Laryngol Otol 112: 393-395.
- Huang TS, Chen HY (2007) Dual thyroid ectopia with a normally located pretracheal thyroid gland: case report and literature review. Head Neck 29: 885-888.
- Steinwald OP Jr, Muehrcke RC, Economou SG (1970) Surgical correction of complete lingual ectopia of the thyroid gland. Surg Clin North Am 50: 1177-1186.
- Yoon JS, Won KC, Cho IH, Lee JT, Lee HW (2007) Clinical characteristics of ectopic thyroid in Korea. Thyroid 17: 1117-1121.
- Hafidh MA, Sheahan P, Khan NA, Colreavy M, Timon C (2004) Role of CO2 laser in the management of obstructive ectopic lingual thyroids. J Laryngol Otol 118: 807-809.
- Mussak EN, Kacker A (2007) Surgical and medical management of midline ectopic thyroid. Otolaryngol Head Neck Surg 136: 870-872.
- Baik SH, Choi JH, Lee HM (2002) Dual ectopic thyroid. Eur Arch Otorhinolaryngol 259: 105-107.
- Galizia G, Lieto E, Ferrara A, Castellano P, Pelosio L, et al. (2001) Ectopic thyroid: report of a case. G Chir 22: 85-88.
- Falvo L, Berni A, Catania A, D’Andrea V, Palermo S, et al. (2005) Sclerosing papillary carcinoma arising in a lingual thyroid: report of a case. Surg Today 35: 304-308.
- Perez JS, Munoz M, Naval L, Blasco A, Diaz FJ (2003) Papillary carcinoma arising in lingual thyroid. J Craniomaxillofac Surg 31: 179-182.
- Goldstein B, Westra WH, Califano J (2002) Multifocal papillary thyroid carcinoma arising in a lingual thyroid: a case report. Arch Otolaryngol Head Neck Surg 128: 1198-1200.
- Casella A, Pisano R, Navarro Cuellar C, Llopis P, Mallagray R, et al. (1999) Papillary carcinoma of the base of the tongue. Case clinic. Minerva Stomatol 48: 535-538.
- Paludetti G, Galli J, Almadori G, Ottaviani F, d’Alatri L, et al. (1991) Ectopic thyroid gland. Acta Otorhinolaryngol Ital 11: 117-133.
- Zink A, Raue F, Hoffmann R, Ziegler R (1991) Papillary carcinoma in an ectopic thyroid. Horm Res 35: 86-88.
- Shah BC, Ravichand CS, Juluri S, Agarwal A, Pramesh CS, et al. (2007) Ectopic thyroid cancer. Ann Thorac Cardiovasc Surg 13: 122-124.
- Alderson DJ, Lannigan FJ (1994) Lingual thyroid presenting after previous thyroglossal cyst excision. J Laryngol Otol 108: 341-343.
- Weider DJ, Parker W (1977) Lingual thyroid: review, case reports, and therapeutic guidelines. Ann Otol Rhinol Laryngol 86: 841-848.
- Puxeddu R, Pelagatti CL, Nicolai P (1998) Lingual thyroid: endoscopic management with CO2 laser. Am J Otolaryngol 19: 136-139.
- Bassem Amr, Sharif Monib (2011) Lingual thyroid: A case report. Int J Surg Case Rep 2(8): 313-315.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...