Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Case Report(ISSN: 2690-5752) 
Isolated Sphenoidal Aspergillosis: Case report and review of literature Volume 9 - Issue 5
Mohamed Ali Gliti1,3*, Niema Benkhraba1,3, Zainab Benyahia1,3, Razika Bencheikh2,3, Mohamed Anas Benbouzid2,3, Abdelilah Oujilal2,3 and Leila Essakalli Houssyni2,3
- 1Resident physician in Otolaryngology, Department of Otolaryngology, Head and Neck Surgery, Ibn Sina University Hospital, Rabat, Morocco
- 2Professor of otolaryngology, Department of Otolaryngology, Head and Neck Surgery, Ibn Sina University Hospital, Rabat, Morocco
- 3Faculty of Medicine and Pharmacy of Rabat, Mohamed V University, Rabat, Morocco
Received: April 14, 2023; Published: April 27, 2023
Corresponding author: Mohamed Ali Gliti, ENT Department, Rabat Specially Hospital, Ibn Sina University Hospital, Hafiane cherkaoui Avenue, 10100 Rabat, Morocco
DOI: 10.32474/JAAS.2023.10.000327
Abstract
Sphenoidal aspergillosis is a rare condition whose diagnosis is not always obvious. The clinician should always bear this diagnosis in mind in patients with chronic sinusitis avoiding invasive and fulminant forms which could be life-threatening. In fact, this work focused on the description of the clinical features of this entity as well as its management by presenting a case report and reviewing literature. by performing tympanoplasty contributes to lessening the infectious risk among these patients. Tympanoplasty is one of the most commonly performed procedures by Otolaryngologists. There are variations of the types of grafts used as well as different techniques.
Keywords: Tympanic membrane perforation; tympanoplasty; scuba diving
Introduction
Sphenoidal aspergillosis is a rare disease whose incidence is estimated at 1.2 % per year [1]. This incidence has undergone an increase in the last decade, due to an epidemiological shift towards fungal infections, and this, in front of the use of antibiotics, corticosteroids, and the development of diagnostic means [2]. Besides, this entity could be probably underestimated due to the lack of systematic mycological sampling and anatomopathological study [3]. Mycotic infection is serious, fatal and its prognosis depends closely on the treatment delay. Diagnosis is usually delayed in the absence of specific clinical signs. Clinician must keep this rare entity in mind, in order to avoid the progression into invasive forms, prognosis of this latest is poorer even with a fatal outcome, and since surgery won’t be curable, thus urgent antifungal treatment will be required.
Case Report
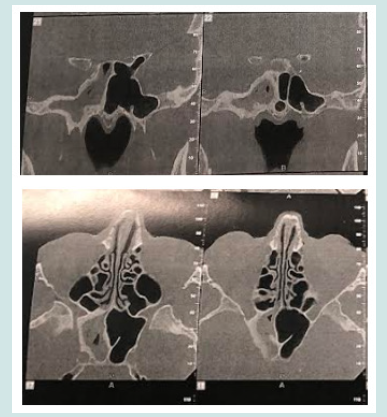
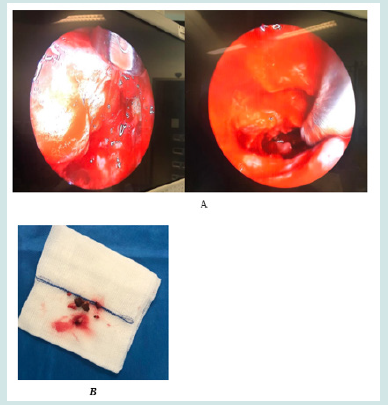
This is a 72-year-old patient, who for several years had chronic headaches, most often on the right, associated with posterior purulent rhinorrhea. The sinus CT scan showed an opacity of the right sphenoid sinus suggestive of aspergillosis (Figure 1). The patient benefited from endoscopic sphenoidotmia with evacuation of purulent intrasinus contents and excision of the pathological mucosa (Figure 2). The pathological study confirms the diagnosis of aspergillosis. The postoperative results were good.
Discussion
Aspergillosis is known as a fungal infection caused by a ubiquitous germ of the genus Aspergillus with a prevalence of fumigatus and flavus species [5]; Aspergillosis commonly involve the maxillary and frontal sinuses. The sphenoidal site, however, is exceptional [3]. Different forms of sphenoidal aspergillosis were described: the noninvasive form, the invasive form that includes chronic invasive sinusitis and fulminant sinusitis that may have serious consequences [6]. Typically, fungal sphenoid sinusitis occurs in immuno compromised subjects and without having any nasal complaints. In fact, cases of sphenoid sinus fungal infection, reported in the literature, without immunocompromise are very common [7], and seems to be related to the chronic noninvasive forms described in the current investigation. On the other hand, many authors have identified a set of risk factors and predisposing medical disease which associated to developing sphenoid aspergillosis more than others, such as patients having allergy, alcoholism, long-term corticosteroid therapy, diabetes, AIDS, the use of anti-tuberculosis drugs or following solid organ transplantation [2,3]. Hypercoticism also has been associated with an increased incidence of aspergillosis [3].
Usually the complications are inaugural of the infection when the invasion hits the structures adjacent to the sinus. The clinical presentation can be neurological, rhinological or even ophthalmological. The sphenoidal location of aspergillosis and the proximity of the neuro-vascular structures are a source of ophthalmological and endocranial complications. These phenomena are explained by mycelial growth and production of cytotoxic metabolites responsible for soft tissue and bone destruction [6]. Intracranial complications involve skull base osteomyelitis, meningitis, meningoencephalitis, brain abscess, and cavernous sinus thrombosis, involvement of orbital apex, infarcts, and rarely mycotic anevrysm [7]. Starting with neurological signs, headache represents one of the most common signs of sphenoidal aspergillosis reported between 67% and 85 % according to different studies [1]; its main characteristics are being retro-orbital or occipital, most often unilateral and often resistant to usual analgesic treatments. These characteristics are explained by the innervation of the sphenoid sinus, which is derived from both cranial nerves V1 and afferent fibers, via the sphenopalatine ganglion [8].
As for ophthalmological signs, mainly explained by orbital extension and cavernous sinus invasion, they are often observed in association with invasive forms [2,3]. They are reported to be the second most common complex symptom in sphenoid diseases. The patients may complain from diplopia often subjective or more commonly secondary to ophthalmoplegia due to multiple nerve palsy [9]. Ptosis was reported in up to 46 % of published cases [10], exophthalmos, ophthalmoplegia or loss of visual acuity ranging from mild to total blindness [8]. The rhinological signs are dominated by anterior and/or posterior purulent rhinorrhea and nasal obstruction, which are very nonspecific. However blood-streaked nasal discharge to be much more specific [1]. Irritation of the sinus mucosa by the aspergilloma or, at a more advanced stage, bone destruction of the sinus wall can explain this bleeding [1]. Radiologically, the standard images appear normal they are currently neglected in terms of invasive sinusitis [2]. Indeed CT scan and MRI represent the most sensitive diagnostic means to highlight an Aspergillus sinusitis by demonstrating ferromagnetic substances [10]. Actually, CT scan is known to be more specific in detecting bone lesions [11]. The most characteristic aspect is the presence of a total filling of the sinus by dense, non-raising material after injection of iodine and comprising a calcium or metal density image corresponding to calcium salts and other heavy metals (lead, copper, iron, manganese) produced by mycosis [2,7].
As for the MRI, it is rather specific for the detection of an extra sinus extension outside the sinus, it is known for its superiority in detecting and evaluating ophthalmological or intracranial extension of the disease [2,3,11]. It appears as a heterogeneous lesion on T1-weighted sequences and T2 not enhanced after injection of gadolinium, including a very hypo-intense zone on the T1-weighted sequences and T2 [11,2]. Despite the technical and diagnostic advances in imaging, the diagnosis is still made during surgery or postoperatively. The confirmation is essentially based on the mycological study of the Aspergillus pus and the anatomopathological examination [12]. Histological examination using Grocott-Gomori stain demonstrated fungal filaments with the conidial head of Aspergillus. The surgery approach is an endoscopic sphenoidotomy which allows evacuation of intrasinus purulent fluid with macroscopic removal of the disease with a generous margin of healthy tissue to ensure resumption of sinus ventilation [3,8]. A complete excision and debridement that allow a radical removal of the diseased tissue determines the prognosis and helps to avoid residual tissue and recurrences [13]. External approach has also a place but, according to some authors, only in particular situations especially when orbits are included [7]. This option is figured out essentially when it is an invasive form. Then surgery become more extensive and could lead to complications such as inadvertent injury to the internal carotid artery, cranial nerves and cavernous sinus. Besides, sometimes we are faced to decide of an exenteration if the lesions reach posterior orbital structures (retro bulbar, apical).
Actually, the suitable treatment for noninvasive chronic aspergillosis is surgery with extrusion of the fungal mass [13]. Regarding antifungal treatment it is not well defined because some authors administrate it to improve the surgical outcome while others admit that a surgery considered radical spares a complementary post-operative treatment [7]. Besides, administration of intravenous antifungal treatment for immunocompetent patients is not consensual [7]. When it is about the invasive form of sphenoidal aspergillosis, surgery should be followed by antifungal treatment [13]. The antifungal compromises triazole (itraconazole, voriconazole, posaconazzole), and polyenes (amphotericin and its lipid formulations) [8]. Amphotericin B has a broad spectrum. However, some authors have described a successful use of voriconazole in combination with a sphenoidotomy that preserves the mucosa as an effective treatment in cases with invasive sphenoidal aspergillosis and was better tolerated than amphotericin B in a recent study [13]. Amphotericin B, not being available for oral application, is associated with a high rate of nephrotoxicity and infusion reactions. Voriconazole, in contrast, is generally well tolerated and distributes well into all tissues including brain and bone, with tissue concentrations that may exceed plasma concentration [14]. This property is important in the treatment of invasive sphenoidal aspergillosis, which often erodes bone and may invade both meningeal and brain. For the treatment of invasive aspergillosis in hematopoietic cancer pa tients, voriconazole was even shown to have superior efficacy and survival rates compared to amphotericin B [15]. According to the literature, mortality is essentially associated with invasive forms, which is observed in 50 % of cases. A regular follow up is recommended to avoid recurrences.
Conclusion
Chronic noninvasive sphenoid sinus aspergillosis appears to be a benign disease, essentially affecting women and patients over the age of 50 years. The symptoms are fairly non-specific. Imaging and histological examination are essential for management. The invasive form is a serious disease requiring rapid, multidisciplinary management.
References
- Thery A, Espitalier F, Cassagnau E, Durand N, Malard O (2012) Clinical features and outcome of sphenoid sinus aspergillosis: a retrospective series of 15 cases. Eur. Ann. Otorhinolaryngol. Head Neck Dis. Août 129(4): 179-184.
- Kamaoui I (2007) Aspergillose sphénoïdale révélée par des signes neuro-ophtalmologiques: à propos d’un cas. J Radiol 88(6): 901-903.
- Zainine R, Hachicha A, Gamra SB, Beltaief N, Sahtout S, et al. (2011) Aspergillose sphénoïdale chez deux patients immunocompé J Mycol Med 21(2): 142-145.
- Agha RA (2020) The SCARE 2020 guideline: updating Consensus Surgical case report (SCARE) Guidelines. Int J Surg déc 84: 226-230.
- Shams MG, Motamedi MHK (2003) Aspergilloma of the maxillary sinus complicating an oroantral fistula. Oral Surg. Oral Med. Oral Pathol. Oral Radiol Endod 96(1): 3-5.
- A Devèze, F Facon, G Latil, G Moulin, H Payan-Cassin, et al. (2005) Cavernous Sinus Thrombosis Secondary to Non-invasive Sphenoid Aspergillosis 43(2): 15-155.
- Jain A, Goyal K, Meher R, Passey JC (2019) Internal carotid artery bleed: a rare complication of invasive sphenoidal aspergillosis. World Neurosurg 129: 292-294.
- Chopra H, Dua K, Malhotra V, Gupta RP, Puri H (2006) Invasive fungal sinusitis of isolated sphenoid sinus in immunocompetent subjects. Mycoses 49(1): 30-36.
- Lee DH, Yoon TM, Lee JK, Joo YE, Park KH, et al. (2014) Invasive fungal sinusitis of the sphenoid sinus. Clin. Exp. Otorhinolaryngol 7(3): 181.
- Boutarbouch M, Arkha Y, El Ouahabi A, Derraz S, El Khamlichi A (2009) Sphenoid sinus aspergillosis simulating pituitary tumor in immunocompetent patient. J Clin Neurosci 16(6): 840-841.
- Aribandi M, McCoy VA, Bazan C (2007) Imaging features of invasive and noninvasive fungal sinusitis: a review. Radio Graphics 27(5): 1283-1296.
- Klossek JM, Kauffman Lacroix C, Dufour X (2005) Agent fongique et pathologie rhinosinusienne. Rev Fr Allergologie Immunol Clin 45(1): 25-28.
- Baumann A, Zimmerli S, Häusler R, Caversaccio M (2007) Invasive sphenoidal aspergillosis: successful treatment with sphenoidotomy and voriconazole. ORL 69(2): 121-126.
- Klastersky J (2004) Empirical antifungal therapy. Int J Antimicrob Agents Févr 23(2): 105-112.
- Denning DW (2002) Efficacy and safety of voriconazole in the treatment of acute invasive aspergillosis. Clin Infect Dis Mars 34(5): 563-571.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...