Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Case Report(ISSN: 2641-1709) 
Infected Lymphangioma Tongue Presenting as Macroglossia – A Case Report Volume 6 - Issue 4
Sumit Sharma1* and Suvarna Sharma2
- 1Associate Professor, Department of ENT, Mayo Institute of Medical Sciences, India
- 2III-year MBBS Student, KMC Manipal, India
Received: May 04, 2021 Published: May 18, 2021
Corresponding author: Associate Professor, Department of ENT, Mayo Institute of Medical Sciences, Barabanki, India
DOI: 10.32474/SJO.2021.06.000242
Introduction
Lymphangioma is a benign hamartomatous hyperplasia of lymphatic vessels, with three-fourths of all cases occurring in the head and neck region [1-4]. Lymphangioma was first described by Redenbacher in 1828 and Lymphangioma of the tongue was first described by Virchow in 1854 [2]. The onset of Lymphangioma is either at birth (60 to 70%) or up to two years of age (90%). It is rare in adults [3-6]. Lymphangioma represent about 6% of the total number of benign tumors of the smooth tissue in patients aged less than 20 years [7]. The oral localization of Lymphangioma is less usual, and the most common site in this case is the tongue, especially the anterior two anterior [8]. Lymphangioma usually affect the ventral part of the tongue and are solitaire or circumscribed. Occasionally, they are associated with Cystic Hygroma [9]. Rarely they are seen on the palate, gingiva, buccal mucosa, and lips. In children, intraoral lymphangioma, especially tongue lymphangioma leading to macroglossia, may cause speech disturbances, poor oral hygiene, mandibular prognathism, open bite, yawning, chewing difficulties, and maxillofacial deformities [6]. Therefore, appropriate and timely treatment is essential to avoid undesirable consequences, which in most cases are caused by macroglossia due to tongue tumors. Various modalities have been applied for treatment of lymphangioma of the tongue. Main aims of the treatment are to give symptomatic relief of pain, edema, lymph and blood leakage, and prevent super infections, as well as addressing cosmetic concerns. The ideal treatment is surgical excision; however, this cannot be applied in all cases and leaves a scar [10]. Other treatment modalities include cryotherapy, radiation therapy, steroid administration, Sclerotherapy, electrocautery, embolization, ligation, laser surgery, and radiofrequency tissue ablation. Successful treatment necessitates inclusion of a surrounding border of normal healthy tissue without damage of vital structures. The following case report is of a patient with Lymphangioma of the tongue and its management.
Case Report
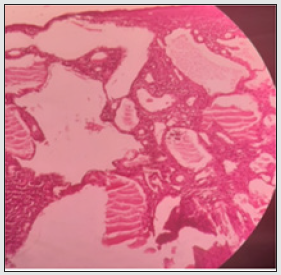
A young female of 20 years presented to the department of ENT at Mayo Institute of Medical Sciences, Barabanki with chief complaints of progressively increasing size of the tongue for the past few years with difficulty in swallowing and dribbling of saliva from the mouth. Recently she started developing difficulty in eating food and closing the mouth due to fullness. Her speech was also affected but her sensation of taste was intact. The patient also complained of bleeding from the lesion site on incurring trauma like mild injury tooth during mouth closure. She also complained of tongue bite during mastication. On inspection tongue was there was a reddish blue colored marked soft tissue swelling involving entire tongue with numerous papillary and vesicle- like projections which made it appear irregular and granular (Figure 1). On palpation, the swelling was soft, non-tender and pebbly. The surface was irregular. The mouth opening was normal and there was no restriction of functions of the tongue however slurring of speech was noted. On the basis of history and clinical features a provisional diagnosis of vascular anomaly of the tongue was made and the patient was subjected to Fine needle aspiration cytology of the tongue which was inconclusive hence later a small biopsy was done under local anesthesia which turned out to be Infected Lymphangioma Tongue (Figure 2). Her systemic examination did not reveal any other congenital anomaly. Since the lesion involved whole of the tongue (both anterior and posterior) hence we decided not to operate and go with Sclerotherapy of the lesion. Patient was admitted and properly investigated and taken up for the procedure after explaining the risks and expected response. 1 ml SETROL (Sodium Tetradecyl Sulphate) with dilution was used for each side of the tongue, the patient experienced swelling of the tongue in the evening which resolved by the morning and otherwise tolerated well. A total of 2 such injections were given at an interval of 1 month which resoled the lesion, her macroglossia got reduced and papilla on the dorsum of tongue reappeared and all other symptoms reduced significantly (Figure 3). She is in follow up for the last one year and is asymptomatic till now.
Discussion
Lymphangiomas are uncommon congenital hamartomas of the lymphatic system, usually diagnosed in infancy and early childhood as lobular masses or cystic lesions. They may be present anywhere on the skin and mucosa. The most usual locations are the head and neck, followed by the proximal extremities, buttocks and trunk. Sometimes they can be located at intestinal, pancreatic and mesenteric level. Lymphangioma rarely affect the oral cavity. Affected sites in the oral cavity may include the tongue, palate, gingival and oral mucosa, lips, and alveolar ridge of the mandible [8]. Two major theories have been proposed to explain the origin of lymphangiomas [11]. The first theory is that the lymphatic system develops from five primitive sacs arising from the venous system. Concerning the head and the neck, endothelial outpouchings from the jugular sac spread centrifugally to form the lymphatic system. Another theory proposes that the lymphatic system develops from mesenchymal clefts in the venous plexus reticulum and spread centripetally towards the jugular sac. Finally, lymphangioma develop from congenital obstruction or sequestration of the primitive lymphatic enlargement. Histopathological classification of lymphangioma is as follows:
a) Lymphangioma simplex, small thin-walled lymphatic vessels.
b) Cavernous lymphangioma, dilated lymphatic vessels with surrounding adventitia.
c) Cystic lymphangioma, large lymphatic spaces surrounded by fibrovascular tissue; and
d) Benign lymphangioendothelioma, lymphatic channels separated by collagen bundles [2].
These categories are somewhat artificial, and many lesions are combinations of categories. The differential diagnosis for lymphangioma includes Hemangioma, Amyloidosis, Congenital hypothyroidism, Neurofibromatosis, Mongolism, Primary muscular hypertrophy. Lymphangioma are known to be associated with Turner’s syndrome, Noonan’s syndrome, trisomies, cardiac anomalies, fetal hydrops, fetal alcohol syndrome, and Familial pterygium colli [6].
A classification of the lymphangioma of head and neck on the base of the spread the anatomical involvement had been proposed by De Serres LM [12]:
a. Stage/class I – Infrahyoid unilateral lesions.
b. Stage/class II – Suprahyoid Bilateral Lesions.
c. Stage/class III – Suprahyoid or Infrahyoid Unilateral Lesions.
d. Stage/class IV – Suprahyoid Bilateral Lesions.
e. Stage/class V – Suprahyoid or Infrahyoid Bilateral Lesions.
f. Stage/class IV – Infrahyoid Bilateral Lesions.
Ricciardelli LJ and Richardson MA [13] demonstrated that Suprahyoid lymphangiomas had a significantly higher rate of recurrence than Infrahyoid lymphangiomas [14]. The commonest complication of the lymphatic malformations is infection, associated with the growth of the lesion. Lymphocytopenia has been documented in all these patients, although a clear correlation with the infection risk must be established [14]. The rapid growth of Lymphangioma can be associated with hemorrhage or can lead to obstruction of the upper respiratory tract, 50% from the children with these lesions requiring tracheotomy [15]. For inexperienced clinicians or in lesions with atypical clinical features a definitive diagnosis should be made through biopsy and histopathological examination. Dental preventive programs must be performed especially for children with macroglossia until surgery is possible. The inability to perform normal dental hygiene activities increases the risk of caries and gingivitis. Adequate surgery helps patients to keep the tongue inside as a good cosmetic result and they also have less orthognathic deformities [8].
Conclusion
Oral Lymphangiomas are uncommon lesions occurring at the dorsal region of the tongue. Conventional treatment with surgical excision with sufficient depth and width is recommended but because recurrence is common and also not possible in all the cases hence other treatment modalities are also used like cryotherapy, laser therapy etc are also used; the later also can be used with superficial lesions. Knowledge for correct diagnosis is of fundamental importance and for proper therapeutic implications. Their early recognition allows proper initiation of treatment and prevents the occurrence of the complications.
References
- Rajendran R (2012) Benign and malignant tumors of the oral cavity. Rajendran R, Sivapathasundharam B (Eds.), Shafers textbook of oral pathology. 7th Ed Elsevier Press, India p. 81-222.
- Bhayya H, Pavani D, Avinash Tejasvi ML, Geetha P (2015) Oral lymphangioma: A rare case report. Contemp Clin Dent 6(4): 584-587.
- Rathan JJ, Vardhan BG, Muthu MS, Venkatachalapathy Saraswathy K, Sivakumar N (2005) Oral lymphangioma: a case report. J Indian Soc Pedod Prev Dent 23(4): 185-189.
- Goswami M, Singh S, Gokkulakrishnan S, Singh A (2011) Lymphangioma of the tongue. Natl J Maxillofac Surg 2(1): 86-88.
- Kayhan KB, Keskin Y, Kesimli MC, Ulusan M, Unür M (2014) Lymphangioma of the tongue: report of four cases with dental aspects. Kulak Burun Bogaz Ihtis Derg 24(3): 172-176.
- V Usha, Sivasankari T, Jeelani S, Asokan GS, Parthiban J (2014) Lymphangioma of the tongue - A case report and review of literature. J Clin Diagn Res 8(9): 12-4.
- Coffin CM, Dehner LP (1993) Vascular tumours in children and adolescents: a clinicopathologic study of 228 tumours in 222 patients. Pathol Annu 28(Pt 1): 97–120.
- Iamaroon A, Pongsiriwet S, Srisuwan S, Krisanaprakornkit S (2003) Lymphangiomas of the tongue. Int J Pediatric Dentistry 13: 62–63.
- Karmody CS, Fortson JK, Calcaterra VE (1982) Lymphangiomas of head and neck in adult. Otolaryngol Head Neck Surg 90(3 Pt 1): 283–288.
- İlknur T AS, Bıçak MÜ, Özer E, Fetil E (2012) A case of lymphangioma treated with pulsed dye laser. Türkderm 46(2): 107-109.
- Patel JN, Sciubba J (2003) Oral lesions in young children: Pediatric Clinics of North America 50(2): 469–486.
- De Serres LM, Sie KC, Richardson MA (1995) Lymphatic malformation of the head and neck: a proposal for staging, Arch Otolaryngol Head Neck Surg 121: 577–582.
- Ricciardelli LJ, Richardson MA (1991) Cervicofacial cystichygroma patterns of recurrence and management of the difficult case. Arch Otolaryngol Head Neck Surg 117: 546–553.
- Hartl DM, Roger G, Denoyelle F (2000) Extensively mphangioma presenting with upper airway obstruction. Arch Otolaryngol Head Neck Surg 126: 1378–1382.
- Alqahtani A, Nguyen LT, Flageole N (1999) 25 years’ experience with lymphangiomas in children, J Pediatr Surg 34(7): 114–118.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...