Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Case Report(ISSN: 2641-1709) 
Functional Preservation Resection Combined with Radiotherapy in the Treatment of Locally Advanced Malignant Maxillary Sinus Tumors: Our Experience in 6 Patients Volume 6 - Issue 5
Weihua Wang† Yujie Zhang†, Jiong Zheng and Zhaoxin Ma*
- Department of Otolaryngology Head and Neck Surgery, Shanghai East Hospital, School of Medicine, Tongji University, PR China
Received:June 08, 2021; Published:June 15, 2021
Corresponding author: Zhaoxin Ma, Department of Otolaryngology-Head and Neck Surgery, Shanghai East Hospital, Tongji University School of Medicine, 150 Jimo Road, Shanghai, 200120, PR China † These authors contributed equally to this work.
DOI: 10.32474/SJO.2021.06.000248
Abstract
Objective: The aim of this study was to explore the feasibility and efficacy of functional preservation surgery combined with radiotherapy in the treatment of malignant tumors of maxillary sinus.
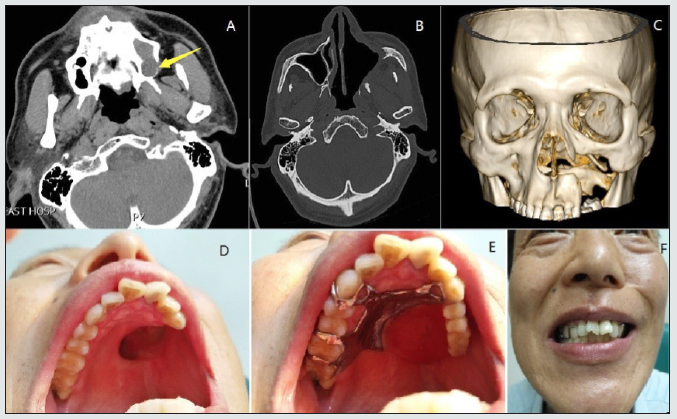
Materials and Methods: The authors retrospectively reviewed 6 cases of malignant tumors of maxillary sinus who had undergone functional preservation resection and were given radical radiotherapy 4 weeks after operation between January 2012 and May 2021. One case underwent radical maxillary sinus surgery, 4 cases lateral rhinotomy, and 1 case partial maxillectomy.
Results: The series included 6 male patients between 42 and 84 years old (average 58.7 years). Pathological types include squamous cell carcinomas (n=2; 1 case of well-differentiated squamous cell carcinomas), adenoid cystic carcinoma (n=2), small round cell malignant tumor with intrastriatal infiltration (n=1), and malignant transformation of inverted papilloma (n=1). Patients were clinically followed up for a median of 72 months (range 37-111 months), and all the 6 cases are alive with good quality of life.
Conclusions: In this single-center report from relatively small series of maxillary sinus malignant tumors, we demonstrate that functional preservative resection combined with radical radiotherapy is generally safe and effective for different types of maxillary sinus malignant lesions.
Keywords:Malignant tumor; radiotherapy; maxillary sinus; lateral rhinotomy; partial maxillectomy
Introduction
Malignant tumor of the paranasal sinus is relatively rare, accounting for less than 1% of the whole-body malignant tumor and about 3% of the head and neck malignant lesion, 80% of which occurs in the maxillary sinus [1-3]. However, due to the special anatomical site and few early symptoms, maxillary sinus tumor is not easy to be found and diagnosed. Thus, most of these tumors are advanced by the time they are diagnosed. Usually, extensive surgical resection is required to achieve maximum removal of the tumor. Maxillary sinus is adjacent to some critical organs and structures, therefore, extensive resection is still limited and challenging, and may result in various postoperative cosmetic and functional disabilities. The limited extent of surgery may have a significant impact on the treatment outcome. The majority of treatment failure in locally advanced maxillary sinus cancer was local recurrence [4,5]. In addition, the 5-year overall survival rate of surgical intervention alone is about 27% [6]. Functional preservation surgery can preserve more normal structures and function of maxilla. Combined with radiotherapy, multimodal approaches in the treatment of locally advanced maxillary sinus tumors can improve survival outcomes [4,7]. Currently, data regarding the functional preservation surgery combined with radiotherapy limited. The purpose of the present study is to explore the feasibility and efficacy of functional preservation surgery combined with radiotherapy in locally advanced malignant maxillary sinus tumors.
Materials and Methods
Ethical consideration
The present study was performed by reviewing the patients’ medical records and radiographic imaging data. The procedure and protocol were approved by the Ethics Committee of Shanghai East Hospital. Written informed consents were provided by all of the patients.
Patients
According to the American Joint Committee on Cancer Staging System for maxillary sinus tumors, 6 patients with locally advanced maxillary sinus tumors were analyzed in this study between January 2012 and May 2021. All patients underwent a complete history and physical examination with clinical staging, complete blood cell count, liver function tests, renal function tests, chest X-ray, and computed tomography (CT) scan and/or magnetic resonance imaging (MRI).
Methods
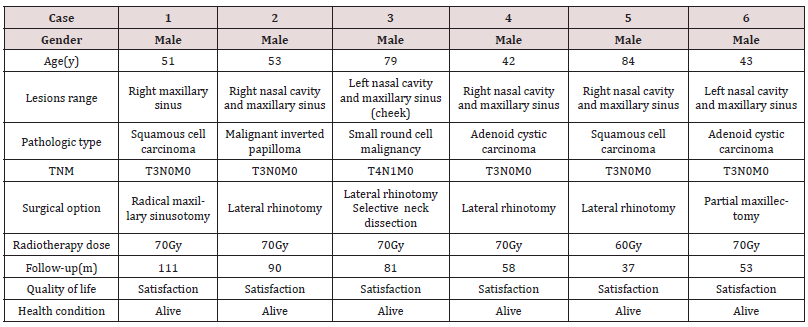
All patients underwent a planned functional preservation resection. The surgical types were decided according to the range of the lesions. Surgical options consisted of radical maxillary sinusotomy (namely Caldwell-Luc operation), lateral rhinotomy, partial maxillectomy, and selective neck dissection. Postoperative radical radiotherapy was given 4 weeks after operation. In case 1, CT scan showed that there was destruction and absorption of bone in the medial wall of maxillary sinus, and the tumor tissue was limited in the right maxillary sinus in MRI (Figure 1A). The patient underwent radical maxillary sinusotomy. In case 2-5, the tumor tissues of maxillary sinus protruded into the ipsilateral nasal cavitys. Figure 2A showed that the tumor tissue was full of the right nasal cavity and maxillary sinus with bone destruction and absorption of hard palate, and the tumor protruded into the mouth. The lesions were completely removed through lateral rhinotomy in these patients. Case 3 underwent selective neck dissection because of ipsilateral cervical lymph node metastasis. In case 6, CT scan showed bone destruction of alveolar process in the posterior inferior wall of the left maxillary sinus, and tumor tissue penetrated the maxillary sinus (Figure 3A). The patient underwent left partial maxillectomy. The defect of maxilla and hard palate after operation were shown in Figure 3C & 3D. One year after the operation, false tooth was made to repair the defect of upper alveolar bone and hard palate, correcting the mastication and pronunciation function. Postoperative radiotherapy to all patients was started within 4-5 weeks of primary surgery at a dose of 60-70 Gy in 30-35 sittings at 2 Gy/fraction, five days a week. In patient with cervical lymph node metastasis, the radiation field included the neck. The patients were followed closely by an otolaryngologist and radiation oncologist with physical examinations and CT scans or MRI every 3 to 6 months.
Figure 1: Squamous cell carcinoma in right maxillary sinus from Case 1. (A) Magnetic resonance imaging scan before radical maxillary sinus surgery. (B) Magnetic resonance imaging scan after surgery. (C) Endoscopic examination of the right nasal cavity after surgery. (D) Three-dimensional computed tomography reconstruction of craniofacial bone (anterior view).
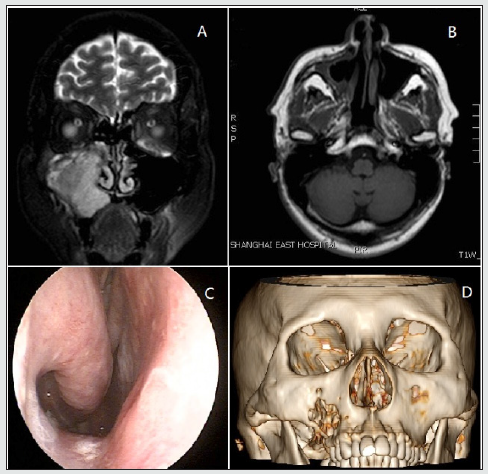
Figure 2: Squamous cell carcinoma in right nasal cavity and maxillary sinus from Case 5. (A) Magnetic resonance imaging scan before lateral rhinotomy. Bone destruction and absorption of hard palate (Red arrow). (B) Magnetic resonance imaging scan after surgery. (C) Three-dimensional computed tomography reconstruction of craniofacial bone (anterior view). (D) Threedimensional computed tomography reconstruction of craniofacial bone (inferior view). Partial bone defect of hard palate (Red arrow). (E) Photograph of the upper palate. (F) Frontal face photograph.
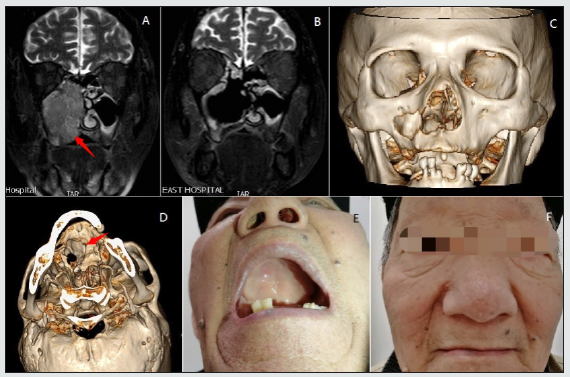
Figure 3: Adenoid cystic carcinoma in left nasal cavity and maxillary sinus from Case 6. (A) Computed tomography scan before partial maxillectomy. Bone destruction and absorption of the posterior lateral wall of left maxillary sinus (Yellow arrow). (B) Computed tomography scan after surgery. (C) Three-dimensional computed tomography reconstruction of craniofacial bone (anterior view). (D) Photograph of the upper palate showing hard palate defect. (E) Photograph of the upper palate with maxillary prosthesis. (F) Frontal face photograph.
RESULTS
Six patients with previously untreated locally advanced malignant maxillary sinus tumor were treated with the functional preservative resection combined with radical radiotherapy in this study (Table 1). The median age of the patients was 52 years (range 42 to 84 years). All patients were male and presented with advanced Stage III and IV. Pathological types include squamous cell carcinomas (n=2), adenoid cystic carcinoma (n=2), small round cell malignant tumor with intrastriatal infiltration (n=1), and malignant transformation of inverted papilloma (n=1). Patients were clinically followed up for a median of 72 months (range 37- 111 months). During the follow-up period, all patients had no tumor local recurrence or distant metastasis. No apparent facial deformities were observed. The patients had no impairment of chewing or pronunciation and were satisfied with the clinical effect and quality of life. Figure 1B & 1C showed the situation of right maxillary sinus and nasal cavity in Case 1 seven years after radical maxillary sinusotomy, and 3D reconstruction of maxilla showed no deformity (Figure 1D). The tumors in the maxillary sinus invaded the nasal cavity in Case 2-5, and the intraoperative and postoperative conditions after lateral rhinotomy were similar in these patients. Figure 2B & 2C showed the situation of right maxillary sinus 3 years after surgery in Case 5. Three-dimensional reconstruction of maxilla showed the hard palate defect caused by tumor (Figure 2D). The hard palate mucosa is intact (Figure 2E), and the facial morphology was normal (Figure 2F). Figure 3B & 3C showed the situation of left maxillary sinus 3 years after partial maxillectomy in Case 6. The left alveolar bone and the anterior wall of the maxillary sinus were missing (Figure 3D). After maxillary prosthesis, the patient had no obvious disturbance in eating and pronunciation (Figure 3E) and the quality of life was improved significantly. The patient’s appearance was normal (Figure 3F).
Discussion
The early stage of malignant maxillary sinus tumor can be asymptomatic, if present, they are nonspecific. It is difficult to distinguish with benign lesions and inflammation. The advanced malignant maxillary sinus tumors often invade the orbit, alveolar process, hard palate, facial skin, pterygopalatine fossa, skull base, and other areas. Extensive surgical resection is challenging for both the patients and the surgeons. Ideal goals for the treatment of malignant maxillary sinus tumors include preservation of mastication, vision, appearance, and oral communication as well as life [8]. Multimodality therapies have been recommended by many authors, including en bloc radical resection and perioperative irradiation [3]. The combined regimen enables the tumor to be removed as thoroughly as possible while retaining the function of the maxilla as much as possible. In recent years, due to the widespread application of CT scan, MRI, and other imaging methods, the early diagnosis rate of malignant maxillary sinus tumors has increased significantly. With the expansion of endoscopic sinus surgery and the promotion of precise radiotherapy, the prognosis of malignant tumors of maxillary sinus was improved obviously. Total endoscopic resection can achieve minimally invasive surgery, but the curative effect of endoscopic resection of malignant maxillary sinus tumors is usually lower than that of conventional extensive surgery. Therefore, we performed endoscopic assisted open pathway resection combined with radical radiotherapy in the treatment of patients with locally advanced malignant maxillary sinus tumors. The open surgery options we used included radical maxillary sinus surgery, lateral rhinotomy, and partial maxillectomy, allowing to remove large masses of tumor tissue under direct vision.
Combined with the advantages of wide-angle, clear field of vision and image magnification of nasal endoscopy, tumor tissue can be removed to the maximum extent while retaining the function of the maxilla as much as possible. In our 6 patients, 1 case underwent radical maxillary sinus surgery, 4 cases lateral rhinotomy, and 1 case partial maxillectomy. At the same time of resection of tumor tissue, the stent structure of maxilla was preserved. Thus, the facial shape and jaw function were preserved. With the advances in high precision radiotherapy techniques, the toxicities related to the radiotherapy have decreased and the ability of target coverage has increased. It is reported that high-dose radiotherapy resulted in excellent local control rates irrespective of the extent of surgery [9]. A retrospective analysis showed that the overall survival and local control with modern radiotherapy techniques were comparable with older studies in patients with paranasal sinus cancer, but the incidence of complications has significantly declined [10]. In this study, all patients were given 70 Gy radical radiotherapy, except Case 5 (60 Gy), and had better survival outcomes. In this single-center report from relatively small series of maxillary sinus malignant tumors, we demonstrate that functional preservative resection combined with radical radiotherapy is generally safe and effective for different types of malignant maxillary sinus lesions. Further studies with more patients and longer follow-up may confirm these results.
References
- Rinaldo A, Ferlito A, Shaha AR, Wei WI (2002) Is elective neck treatment indicated in patients with squamous cell carcinoma of the maxillary sinus? Acta Otolaryngol 122: 443-447.
- McMahon JD, Wong LS, Crowther J (2013) Patterns of local recurrence after primary resection of cancers that arise in the sinonasal region and the maxillary alveolus. Br J Oral Maxillofac Surg 51: 389-393.
- Lund VJ, Clarke PM, Swift AC (2016) Nose and paranasal sinus tumours: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol 130: S111-S118.
- Dulguerov P, Jacobsen MS, Allal AS (2001) Nasal and paranasal sinus carcinoma: are we making progress? A series of 220 patients and a systematic review. Cancer 92: 3012-3029.
- Ganly I, Patel SG, Singh B (2005) Craniofacial resection for malignant paranasal sinus tumors: Report of an International Collaborative Study. Head & neck 27: 575-584.
- Blanco AI, Chao KS, Ozyigit G (2004) Carcinoma of paranasal sinuses: long-term outcomes with radiotherapy. International Journal of Radiation Oncology, Biology, Physics 59: 51-58.
- Kim WT, Nam J, Ki YK (2013) Neoadjuvant intra-arterial chemotherapy combined with radiotherapy and surgery in patients with advanced maxillary sinus cancer. Radiat Oncol J 31: 118-124.
- Nishino H, Ichimura K, Tanaka H (2003) Results of orbital preservation for advanced malignant maxillary sinus tumors. The Laryngoscope 113: 1064-1069.
- Resto VA, Chan AW, Deschler DG, Lin DT (2008) Extent of surgery in the management of locally advanced sinonasal malignancies. Head & Neck 30: 222-229.
- Chen AM, Daly ME, Bucci MK (2007) Carcinomas of the paranasal sinuses and nasal cavity treated with radiotherapy at a single institution over five decades: are we making improvement? International Journal of Radiation Oncology, Biology, Physics 69: 141-147.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...