
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Research Article(ISSN: 2641-1709) 
Effect of Thermo-Electrical Stimulation Therapy on Exhaled Nitric Oxide Concentration: Potential of Biotherapy as a Treatment for Long COVID Volume 9 - Issue 4
Hirobumi Ito*, Miyuki Fujimatu and Emi Takahashi
- Department of ENT, Ito ENT Clinic, Japan
Received: December 14, 2022; Published: December 21, 2022
Corresponding author: Hirobumi Ito, Department of ENT, Ito ENT Clinic, Japan
DOI: 10.32474/SJO.2022.09.000316
Abstract
Thermo-electrical stimulation therapy (hereinafter referred to as biotherapy) is a combination of thermal and electrical stimulation therapies to relieve muscle tension and improve circulation in the head and neck regions. Biotherapy is postulated to have a similar mechanism of action to epipharyngeal abrasive therapy (EAT). Fractional exhaled nitric oxide (FeNO) levels were measured as a measure of efficacy. The results showed that FeNO levels significantly decreased following biotherapy treatment, suggesting a similar mechanism of action to that of EAT. The possibility of biotherapy as a treatment for long COVID (LC) is being discussed.
Keywords: Biotherapy; EAT; FeNO; Long COVID; Electroacupuncture
Abbreviations: EAT: Epipharyngeal Abrasive Therapy; FeNO: Fractional Exhaled Nitric Oxide; LC: Long COVID; rmANOVA: Repeated Measures Analysis of Variance; TES: Therapeutic Electrical Stimulation; FES: Functional Electrical Stimulation; rTMS: Repetitive Transcranial Magnetic Stimulation; tDCS: Transcranial Direct Current Stimulation
Introduction
Epipharyngeal abrasive therapy (EAT) is a treatment for chronic epipharyngitis [1]. The following are the mechanisms of EAT: local mucous membrane astringent, bactericidal, and anti-inflammatory effects of zinc chloride; improvement of local circulation and cerebral lymphatic function by phlebotomy; and autonomic nerve stimulation [2,3]. However, several aspects remain unknown. Uebaba highlighted a connection with the venous hub theory regarding the mechanism of action of EAT [4]. As for its mechanism of action, he speculated that EAT has a circulatory stimulating effect by promoting venous and cerebrospinal fluid lymphatic return, a parasympathetic stimulating effect by somatic-autonomic reflex caused by head and neck stimulation, and a stimulating effect on the autonomic nervous system by triggering the respiratory pump action (parasympathetic stimulation by expiration due to the Hering- Breuer reflex and sympathetic stimulation by inspiration) by changes in the chest cavity pressure [5,6]. The author speculates that the circulation-improving and autonomic nerve stimulating effects may play a significant role in the mechanism of immediate effects of EAT. Thermo-electrical stimulation therapy is a combination of thermal [7] and electrical stimulation therapy [8] and is called biotherapy. Ito reported that biotherapy has sympathomimetic effects [9]. The author speculated that biotherapy may have a similar mechanism of action to that of EAT. Conventionally, the effectiveness of EAT is frequently measured by the amount of local bleeding and the degree of improvement in subjective symptoms [10]. Mogitate reported that the concentration of fractional exhaled nitric oxide (FeNO) decreased with the effect of EAT treatment [11,12]. Therefore, the measurement of FeNO levels may be a biomarker for determining the therapeutic effect of EAT. In this study, we evaluated the effect of biotherapy on the airway epithelium by measuring the change in FeNO levels before and after biotherapy treatment. EAT is expected to be a treatment for long COVID (LC), and we hypothesize that biotherapy may have similar therapeutic effects.
Participants and Methods
The participants were 10 adults (mean age, 38.7 ± 13.5 years), 2 males (mean age,56.0 ± 8.5 years) and 8 females (mean age, 34.4 ± 10.8 years), who underwent biotherapy to relieve muscle tension and improve circulation at this hospital from June to September 2022. Thermotherapy was initially performed for approximately 30 min. The whole body was heated using DREAM UP®, a high-frequency heating device that uses electromagnetic waves in the radiofrequency range. Following this, electrical stimulation therapy was performed using the BBCP_BIO WAVE® with a weak current of 1 mA transcutaneously along the meridians and myofascial meridians for approximately 30 min. In this study, to examine the effect of biotherapy on FeNO, FeNO levels were measured before and after the treatment using a nitric oxide gas analyzer NO breath (measurement range, approximately 5-300 ppb). The FeNO level was measured on an empty stomach, and smokers and those taking anti- allergy medications were excluded. In this study, the FeNO level measured in the same participants without biotherapy was considered the control group, whereas the FeNO level measured following biotherapy was compared with that in the biotherapy group.
First, a t-test (paired t-test) was performed between the control and biotherapy groups, comparing the measured values before the start of treatment (0-min value) and at the end of treatment (60- min value) between the two groups.
Next, to examine changes over time, repeated measures analysis of variance (rmANOVA) was performed on the measurements available before the start of treatment (0-min value), at the end of the treatment (60-min value), 1 h after the end of treatment (120- min value), and 2 h after the end of treatment (180-min value). Multiple comparisons were made using the Bonferroni method. As there is individual variation in the measured values, the rate of change was determined based on the pretreatment values for each case. rmANOVA was performed by obtaining the rate of change at the end of the treatment (60-min value), 1 h after the end of the treatment (120-min value), and 2 h after the end of the treatment (180-min value). Multiple comparisons were performed using the Bonferroni method. Statistical analysis was performed using statistical software EZR version 2.6-2. A risk rate of <5% was considered statistically significant. Oral and written informed consent was obtained from all participants, and the study was conducted in compliance with the Declaration of Helsinki. When handling the data and other materials related to the study, great care was observed to protect the confidentiality of the participants. Furthermore, any information that could identify the participants was excluded when we published the study results. This is a retrospective observational study based on existing medical records, and no new samples or information were obtained.
Results
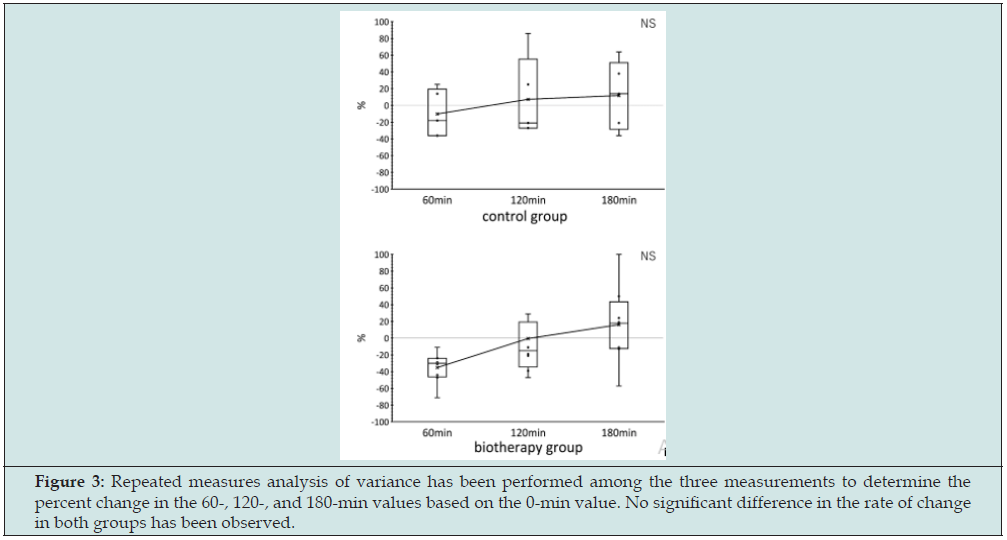
The FeNO levels of the participants (n=10) before (0-min value) and after (60-min value) treatment was compared using paired t-test. The control group had FeNO levels of 11.5 3.6 and 10.0 ± 3.2 before and after the treatment, respectively, with no significant difference noted (P=0.076). The biotherapy group had FeNO levels of 13.0 ± 5.3 and 8.5 ± 4.0 before and after the treatment, respectively, with no significant difference observed (P=0.001). The biotherapy group showed a significant decrease in FeNO levels before (13.0 ± 5.3) and after (8.5 ± 4.0) the treatment (p=0.001) (Figure 1). The control (n=5) and biotherapy (n=8) groups were able to take four measurements at 0, 60, 120, and 180 min. rmANOVA on the measurements of the two groups showed that the measurements fluctuated over time, with a significant difference between the 0- and 60-min measurements. A significant difference was observed between the 0- and 60-min values. The control group showed less fluctuation, whereas the biotherapy group showed greater fluctuation. The biotherapy group showed a greater decrease in 60-min values than the control group, indicating a tendency for FeNO (Figure 2). To exclude the variation of FeNO due to individual differences, rmANOVA was performed between the three measurements by determining the rate of change of the 60-, 120-, and 180-min values with the 0-min value as the reference. No significant difference was noted in the rate of change for both groups. Although no significant difference was noted, the biotherapy group showed a tendency to suppress the 60-min FeNO values compared with the control group (Figure 3).
Figure 1: Comparison of FeNO values before (0-min value) and after (60-min value) treatment in the control and biotherapy groups. The biotherapy group shows a significant decrease in the FeNO level after the treatment compared with that before the treatment.
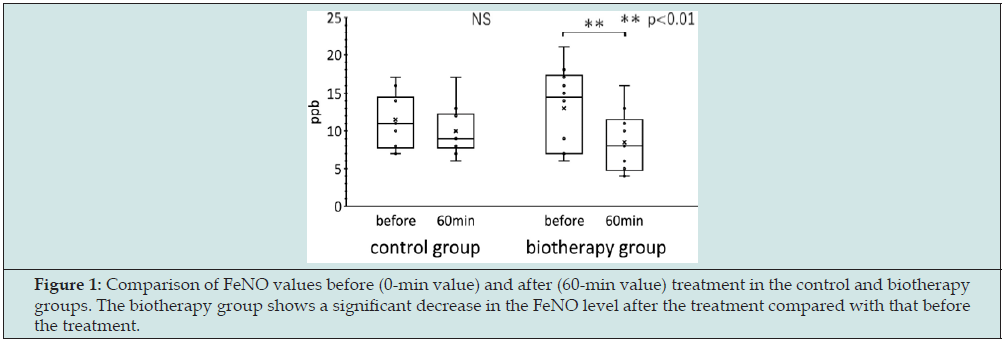
Figure 2: Repeated measures analysis of variance has been performed on measurements taken before the start of treatment (0-min values), at the end of treatment (60-min values), 1 h after the end of treatment (120-min values), and 2 h after the end of treatment (180-min values). Significant differences have been observed between the 0- and 60-min values, and recovery to the same level has been observed at the 120-min value.
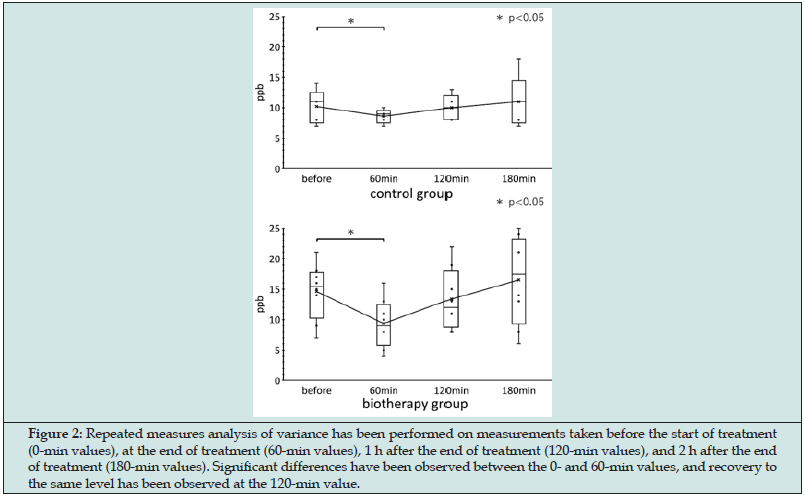
Figure 3: Repeated measures analysis of variance has been performed among the three measurements to determine the percent change in the 60-, 120-, and 180-min values based on the 0-min value. No significant difference in the rate of change in both groups has been observed.
Discussion
The results of this study showed that biotherapy suppressed FeNO levels immediately after the end of the treatment (60-min value). Since FeNO reflects the degree of type 2 inflammation in the lower airway, biotherapy may suppress type 2 inflammation in the airway epithelium. First, we would like to discuss the significance of biotherapy and its mechanism of action. Electrostimulation therapy, massage therapy, thermotherapy, acupuncture, and other physical stimulation therapies are called physical therapy; together with exercise therapy, they form the mainstay of rehabilitation medicine. Electrostimulation therapy is a therapeutic application of biological reactions caused by electrical energy and is applied in various fields, including analgesia, muscle tension relaxation, joint range of motion improvement, muscle strengthening, neuromuscular reeducation, atrophy prevention, circulation improvement, wound healing, and edema improvement [7]. Thermotherapy is one of the basic types of physical therapy, which involves temperature stimulation to heat or cool the body. The hyperthermia used in this study is deep hyperthermia, which uses electromagnetic waves in the radiofrequency range to generate Joule heat in the body’s tissues by vibrating the body’s cells at the molecular level and heating them from deep inside the body [8]. It has the effects of analgesia, circulation improvement, tissue heating, wound healing, immune activation, and relaxation through symptom relief.
Biotherapy is a combination of thermal and electrical stimulation therapies to achieve a synergistic effect. It has been reported that biotherapy promotes circulation in the human body through comprehensive action via massage and thermal effects, as well as promotes myofascial release and activates autonomic nervous system activity by energizing the fascia [9]. The subcutaneous tissue, fascia, and various diaphragms of the whole body are connected by a connective tissue called the fascia, which is mostly composed of collagen. Collagen is believed to be a piezoelectric element that generates piezoelectricity and may be involved in information transmission [13]. Based on the theory that the phenomenon of weak electricity flowing through the fascia is the meridian phenomenon [14], biotherapy was developed as a method for externally regulating the flow of electric current in the body. By monitoring how the participant feels and the state of muscle contraction and freely selecting the stimulation conditions and site, biotherapy can be adjusted to the participant’s needs. Furthermore, it is possible to stimulate the scalp and perform a head massage. An increase in theta waves is observed in the electroencephalogram when scalp stimulation is performed [5], and it is expected to be performed not only for the benefits of scalp massage but also for neuromodulation [15].
Conventional electrical stimulation therapy (electrical stimulation that stimulates the skin surface) is classified into therapeutic electrical stimulation (TES) and functional electrical stimulation (FES), depending on the treatment method and purpose. TES aims to elicit purposeful muscle activity through electrical stimulation, whereas FES is an electrical stimulation therapy that aims to compensate for lost body functions, including central paralysis. Microcurrent therapy, which uses microcurrent stimulation at the insensitive μA level, is also used. In addition to its pain-relieving effect, microcurrent therapy has been shown to promote the healing of damaged tissues [16]. Bioelectric current is believed to be approximately 50 μA and is generated mostly during signal transduction in cells [17]. Bio currents are generated during cell activity and injury; however, they are attenuated by aging, stress, and adverse events. It has been reported that the application of weak currents of 1 mA or less increases mitochondrial ATP synthesis capacity and activates cell functions [18,19]. The biotherapy performed in this study is expected to be as effective as TES, FES, and microcurrent stimulation therapy. Regarding safety, the biotherapy used in this study was designed for a maximum stimulation of 1 mA at level 8. This is the range from AC-1 to AC-2 according to the International Electrotechnical Commission; although involuntary muscle contraction occurs, there are typically no harmful electrophysiological effects. It is a safe treatment with no harmful electrophysiological effects on the human body regardless of the duration of energization [20].
A treatment method like biotherapy is electroacupuncture therapy, which combines electrostimulation therapy and acupuncture. Electroacupuncture therapy, wherein muscles are inserted with needles and stimulated, can directly stimulate muscles with low electrical resistance, thereby efficiently improving muscle blood circulation, efficiently stimulating afferent nerves to activate the analgesic system, and modulating autonomic nervous system functions through hormone secretion by reflex responses. Electrical stimulation and electroacupuncture are useful methods; however, they are considered to have the disadvantage of stimulating fixed sites. Biotherapy is a manual method of electrical stimulation, and its advantage is that the stimulation site can be freely selected and moved. Stimulation conditions can be adjusted in detail according to the purpose of stimulation while observing how the participant feels and the state of muscle contraction. Biotherapy does not cause any pain sensation, and by moving the stimulation along the meridians, polymodal receptors, which are believed to be present in several acupuncture points and deep tissues, can be efficiently stimulated. By providing line and surface stimulation along meridians, nerve, and muscle lines to improve flow, biotherapy can be used to efficiently stimulate a wide range of afferent nerves. The results of this study showed that biotherapy significantly decreased the FeNO level in the biotherapy group compared with that in the control group, suggesting that biotherapy suppresses type 2 inflammation in the airway epithelium and that the suppression of type 2 inflammation decreased inflammatory cytokine levels and normalized systemic cell functions. The comparison of the temporal changes in FeNO levels showed that the suppression of type 2 inflammation by biotherapy was maximal immediately after the treatment and returned to the original level over time.
Type 2 cytokines are produced mainly by type 2 innate lymphocytes in the intestinal tract, lung, skin, adipose tissue, and lymphoid tissue. Type 2 innate lymphocytes express β2-adrenergic receptors, and the response of type 2 innate lymphocytes is inhibitory, as regulated by β2-adrenergic receptors [21]. Therefore, by stimulating the β2-adrenergic receptors of type 2 innate lymphocytes, sympathetic nerve stimulation may suppress type 2 inflammation. It has been reported that sympathetic nerve stimulation induces the depolarization of the cell membrane of the stratum corneum, which is a site of reduced skin current resistance. This site often coincides with meridian points, and biotherapy stimulates meridian points along meridians, which is believed to stimulate sympathetic nerves and produce effects [22] more effectively. Ito H reported that biotherapy induced an overall calming of autonomic nervous activity; however, the sympathetic reflex tended to be stimulated [9]. This suppression of type 2 inflammation may result in a decrease in the levels of inflammatory cytokines and FeNO. Biotherapy may reduce inflammatory cytokine levels and improve vascular endothelial cell functions. To date, COVID-19 infection is prevalent, and symptoms, including respiratory distress, malaise, olfactory and taste disturbances, hair loss, headache, and poor concentration, may persist for several months or longer after COVID-19 infection. Moreover, these symptoms have been reported as sequelae of a new type of coronavirus infection, which is called LC [10]. Regarding the effect of EAT on LC, Imai K reported that symptoms, such as fatigue, headache, and attention disorder, were significantly improved [23]. Additionally, Ito H reported that LC often develops chronic epipharyngitis and that the treatment of chronic epipharyngitis with EAT significantly improved the subjective symptoms of LC. Nishi K reported that EAT suppressed IL-6 and TNFα production in the nasopharyngeal mucosa, and immunohistochemistry revealed a soothing effect of EAT on inflammation [24].
Mogitate M reported that EAT decreased FeNO levels, considering that the improvement of epipharyngitis by EAT suppressed FeNO levels [11,12]. COVID- 19 is involved in systemic endotheliitis, that is, endothelial cell inflammation via ACE2 receptors all over the body, including the heart, brain, lung, kidney, and intestinal tract, and LC is believed to be caused by vascular endothelial cell damage [25]. Inflammation in the brain due to brain microglial activation has been highlighted as a cause of symptoms, including body malaise, fatigue, weakness, and impaired thinking, in myalgic encephalomyelitis/ chronic fatigue syndrome [26]. Noninvasive electrical stimulation, such as repetitive transcranial magnetic stimulation (rTMS) [27] and transcranial direct current stimulation (tDCS) [28], have been reported to be useful as a treatment method. Microglial activation in the brain has also been reported in the sequelae of new-type coronavirus infection (LC); symptoms, including body malaise and brain fog, have become challenging. Moreover, rTMS and tDCS are used as treatment methods for these symptoms. These electrical stimulation methods are believed to normalize arteriovenous blood flow and restore sensory neurons and cognitive functions that have been inactivated by the coronavirus. rTMS has been used as a treatment for depression [27]and brain fog due to LC. Furthermore, microcurrent stimulation of the brain’s active neuronal functions [29] is effective as a treatment for brain fog, and EEG changes were observed with scalp stimulation using biotherapy, suggesting that biotherapy may also be effective as a treatment for brain fog. Additionally, biotherapy may be effective as a treatment for brain fog. These reports suggest that biotherapy, such as EAT, has anti-inflammatory effects and that noninvasive electric stimulation of the scalp may improve LC-induced symptoms. Although this study did not evaluate biotherapy as a treatment for LC, its mechanism of action suggests that biotherapy may be effective for the treatment of various symptoms of LC.
Lázaro A reported that electroacupuncture stimulation of the vastus medialis muscle in rats causes arteriolar dilation and increased blood flow because of muscle contraction. The electroacupuncture stimulation-induced passive muscle contraction activates vascular endothelial cell function, which produces and releases NO, thereby dilating blood vessels and increasing blood flow [30]. Although the results of animal studies suggest that electrostimulation therapy improves vascular endothelial function, biotherapy has similar effects to electroacupuncture stimulation and may be effective for LC by improving vascular endothelial function. However, the long-term effects of biotherapy have not been verified, and further studies are needed. However, considering the current lack of established treatment for LC, it is an urgent issue to establish an effective evaluation and treatment method. This is the reason for the present study.
Conclusion
The results of this study showed that biotherapy suppressed FeNO levels immediately after the treatment (60-min value). The effect was maximal immediately after the treatment and recovered to the same level as that before the treatment 120 min after the treatment, suggesting that biotherapy suppresses type 2 inflammation by stimulating sympathetic β2-adrenergic receptors. Biotherapy is expected to have not only anti-inflammatory effects but also improve head and neck circulation and brain function. It is expected that biotherapy, such as EAT, will be effective in the treatment of LC.
Acknowledgments
I would like to thank Dr. Kazuo Uebaba, Professor at Hollywood Graduate University and Visiting Professor at Teikyo Heisei University Institute of Oriental Medicine, and Dr. Suwan Kim, Total Medical Beauty Institute, for taking time out of their busy schedules to provide guidance on biotherapy. I would like to express my sincere gratitude to Dr. Mogitate Manabu, Director, Mogitate Otolaryngology, for his guidance in the FeNO measurement.
References
- Hotta O, Tanaka A, Tani S (2016) The importance of epipharyngeal procedures in internal medicine: now, another breakthrough is expected. Somata-Pharyngeal 29(1): 99-106.
- Hotta O, Nagano T (2018) Considerations on a variety of conditions suggested to be associated with chronic epipharyngitis and epipharyngeal abrasive therapy. Somata-Pharyngeal 31(1): 69-75.
- Ito H (2022) Heart rate variability analysis of autonomic nerve reflex in epipharyngeal abrasive therapy (EAT). The Autonomic Nervous System 59(3): 320-326.
- Uebaba K (2017) Epipharyngeal abrasive therapy and venous hub theory. The 5th Annual Meeting of the Japanese Society for Lesions and Diseases, Tokyo 2017-9-2.
- Uebaba K, Nishikawa M (2017) New Edition of Indian Life Science - Ayurveda. Rural Cultural Association, Tokyo pp. 100-101.
- Uebaba K (2017) Considerations on the Mechanism of Action of Stinging Therapy Part 1: The “Venous Circulatory System Hub Hypothesis” and the “Venous Congestive Pain Hypothesis. Eastern Medicine 33(1): 63-77.
- Shomoto Y (2017) Physical Therapy occupational visual text. Yodosha, Tokyo pp.55-67.
- Torino D (2004) High-voltage pulse current therapy. Progress in Physical Therapy 15(1): 27-40.
- Ito H, Takahashi E, Fujimatu M (2021) Statistical study of the effects of hyperthermia and electrical stimulation therapy on autonomic nervous activity. Eastern Medicine 37(1): 3-25.
- Ito H (2022) Effect of epipharyngeal abrasive therapy on long Covid with chronic epipharyngitis. Scholarly Journal of Otolaryngology 8(5): 860-864.
- Mogitate M (2022) Effectiveness of epipharyngeal abrasive therapy on chronic epipharyngitis and the exhaled nitric oxide levels. Internal medicine Tokyo, Japan.
- Mogitate M (2022) Exhaled nitric oxide levels are associated with the severity of chronic epipharyngitis and decreased via epipharyngeal abrasion. Auris Nasus Larynx 49(6).
- Kimura T (1982) Dialectical interpretation of qi pathology - hypothesis that qi is a bioelectric current. Practica Oto-Rhinol. Laryngologia 75(2): 751-755.
- Lesondak D, Superviso KT (2020) Fascia: its existence and unknown role. Ijido no Nihonsha, Yokosuka
- Ito H (2022) Effects of biotherapy on EEG. Presentation at the 29th Biotherapy conference. Tokyo, Japan pp. 10-13.
- Yamada K (2015) Practice of microcurrent therapy. Nagoya Chubu Nihon Kyoiku Bunka Kai Co.
- Nagao T (1973) Safety measures between hospitals and ME equipment. Medical Electronics and Biomedical Engineering. 11(3): 61-68.
- Cheng N, Van Hoof H, Bockx E (1982) The effects of electric currents on ATP generation, protein synthesis and membrane transport in rat skin. Clinical Orthopaedics and Related Research 171: 264-272.
- Fujitani H (2018) Microcurrent stimulation therapy in sports. Journal of St. Marianna University School of Medicine 45: 265-269.
- Ichikawa K (2009) Trends in electric shock hazards and hazard limits of electric shock. Safety Engineering 48(6): 407-412.
- Moriyama S, Brestoff J R, Flamar A-L (2018) β2-adrenergic receptor- mediated negative regulation of group 2 innate lymphoid cell responses. Science. 359(6379): 1056-1061.
- Kimura K (2019) The influence of acupuncture treatment on peripheral circulation and its mechanism of action-A study from basic research. Autonomic Nervous System 56: 146-149.
- Imai K, Yamano T, Nishi S (2022) Epipharyngeal abrasive therapy (EAT) has potential as a novel method for long COVID treatment. Viruses 14(5): 907.
- Nishi K, Yoshimoto S, Nishi S (2022)epipharyngeal abrasive therapy (EAT) reduces the mRNA expression of major proinflammatory cytokine IL-6 in chronic epipharyngitis. International Journal of Molecular Sciences 23(16): 9205.
- Varga Z, Flammer A J, Steiger P (2020) Endothelial cell infection and endotheliitis in COVID-19. Lancet 395(10234): 1417-1418.
- Kuratsune H (2021) Myalgic encephalomyeritis/chronic fatigue syndrome (ME/CFS)-Recent aspects-Neurotherapy 38: 164-169.
- Inoue Y (2016) Repetitive transcranial magnetic stimulation therapy. Neurotherapy 33(2): 228-233.
- Ogata K, Tobimatu S (2015) Fundamentals and clinical applications of transcranial direct current stimulation (tDCS). Measurement and Control 54(2): 106-113.
- Sabel BA, Zhou W, Huber F (2021) Non-invasive brain microcurrent stimulation therapy of long-COVID-19 reduces vascular dysregulation and improves visual and cognitive impairment. Restorative Neurology and Neuroscience 39(6): 393-408.
- Loaiza L A, Yamaguchi S, Ito M, Ohshima N (2002) Electro-acupuncture stimulation to muscle afferents in anesthetized rats modulates the blood flow to the knee joint through autonomic reflexes and nitric oxide. Autonomic Neuroscience: Basic and Clinical 97(2): 103-109.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




