Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Research Article(ISSN: 2641-1709) 
Does Lower Eyelid Full Thickness Reconstruction Always Need Local Flap Under the Cartilage Graft? Volume 8 - Issue 4
Javad Rahmati1,2 Shahriar Haddady Abianeh1,2 Hosseinali Abdolrazaghi3 and Hojjat Molaei1*
- 1Plastic & reconstructive surgery Department, Medicine school, Tehran University of Medical Sciences, Iran
- 2Plastic & reconstructive surgery Department, Razi Hospital, Tehran University of Medical Sciences, Iran
- 3Hand & reconstructive surgery Department, Sina Hospital, Tehran University of Medical Sciences, Iran
Received: July 19, 2022; Published: August 02, 2022
Corresponding author: Hojjat Molaei, Plastic & reconstructive surgery Department, Medicine school, Tehran University of Medical Sciences, Iran Vali-e-asr Hospital, IKHC, Bagherkhan St, Towhid Sq, Tehran, Iran
DOI: 10.32474/SJO.2022.08.000295
Abstract
Background: BCC and SCC are common eyelids skin cancers may need more consideration in full-thickness involvement. Incomplete reconstruction in depth or in width can result in loss of strong support and skin shrinkage, and lid retraction, respectively. Sandwich auricular graft between inner flap/graft and overlying skin flap is generally accepted by surgeon.
Patients and methods: 15 patients with BCC or SCC in lower eyelid region who expected to have full thickness defect during cancer surgery, entered a descriptive study. During procedure after tumor resection with safe margin reconstruction was done as harvesting concha cartilage and fixation to peripheral conjunctiva and coverage via regional skin flaps. Raw surface of cartilage was left intact to be re-epithelialized. Demographic and intra-operative evaluations were recorded and analyzed.
Results: 6 women and 9men underwent surgery. 3 SCC and 12 BCC were resected. tumors were mostly toward lateral cantus. The mean length of lining defect after tumor resection was 21 mm. reconstruction of skin defects were as different skin flaps over the cartilage.
Discussion: full thickness lower eyelid reconstruction demands well peripheral tissues to achieve long-term results. In primary cancers, there are numerous cutaneous and musculocutaneous flaps to transfer the defect area and cover the fixed cartilage as supporting structure. This well-nourished flap not only covers the skin defect, but also provide conditions that cause re-epithelialization over the cartilage without any complication.
Conclusion: full-thickness lower eyelid defects can be reconstructed with auricular autograft and then skin coverage by regional flaps without need to inner coverage under cartilage
Keywords: Skin cancer; auricular autograft; lower eyelid reconstruction, lid retraction, re-epithelialization
Introduction
Skin cancers especially BCC and SCC are commonly seen in various parts of the body, especially in face which encounters sun rays. Lower eyelids are not uncommon site for different presentations of such cancers. According to accepted protocols safe margin should be respected in surgeries which may be up to 4-6 mm in BCCs and 10 mm in SCCs [1]. Severe scarring and malposition of the lower eyelid following cancer surgery are usually challenging for surgeons to reach ideal aesthetic and functional results. This goal can be achieved via respecting to full thickness reconstruction [2]. Lower eyelid is less complex than upper lid with more laxity, though long-term morbidity makes it important to be corrected properly [3]. Full thickness defects of lower eyelid predispose eye to trauma and should be considered as soon as possible. Thus, numerous options introduced to improve results. Generally accepted solution is three-layer reconstruction. Cartilage graft-harvested from ear or ribs among other layers prevent subsequent contracture and provides structural support [4]. We tried to share our experiences in intraoperative approach to manage full thickness lower eyelid defects with only cartilage graft and overlying skin flap.
Patients and Methods
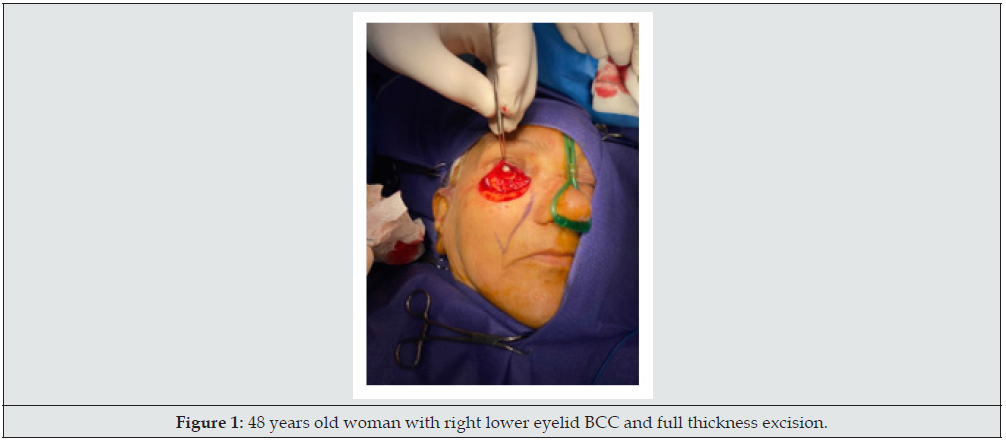
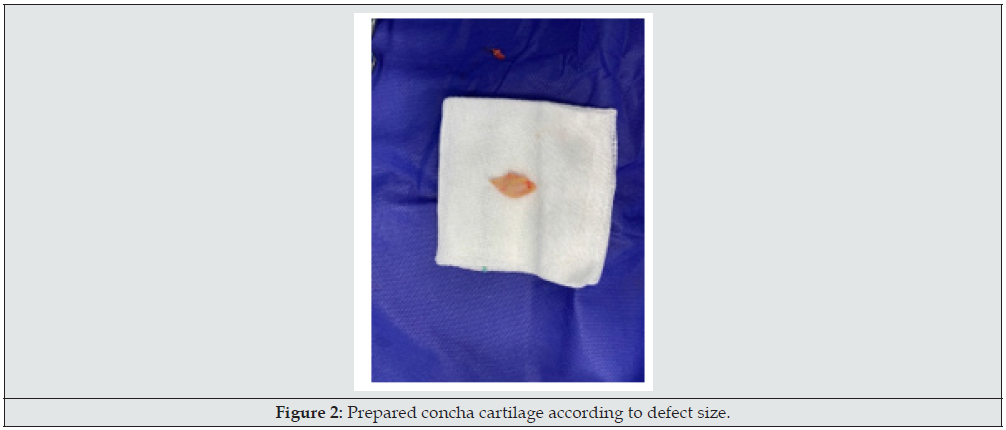
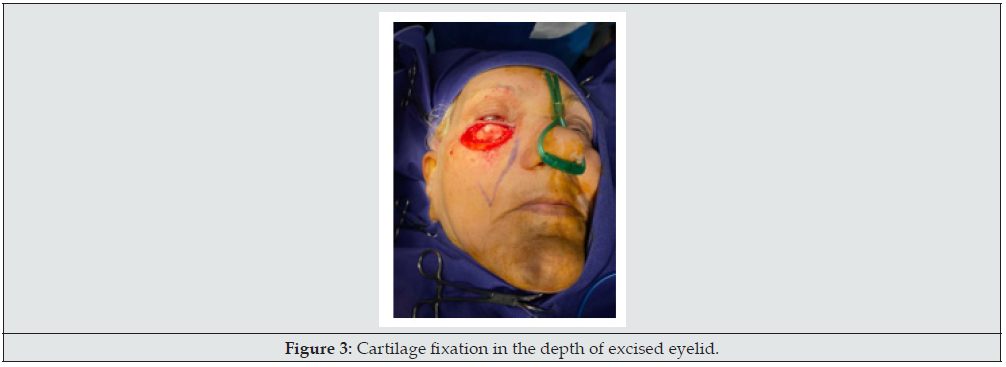
15 patients with skin cancer of lower eyelid who referred for oncoplastic surgery and had wide local tumor excision and full thickness defect, included in the study (Figure 1). Patients had signed informed consent and had received enough information about plans and ultimate outcome. Exclusion criteria included major comorbidities interfering with reconstruction, patient disagreement, and previous eye surgeries of cornea. In all patients after tumor resection and confirming safe margin by frozen tissue diagnosis, ipsilateral concha was harvested via lateral auricular incision and prepared to use (Figure 2). As the resulted defect had full-thickness 3 layers, at first, this cartilage block sutured to the borders of lining defect with fine absorbable sutures meticulously to cover inner layer defect (Figure 3). Upon satisfaction of internal repair and confirmation of negative margin by frozen section, according to patients` condition and defect size, a reconstructive regional or local flap was chosen, and ultimate coverage completed (Figure 4). In postoperative period, patients received artificial tear drops and topical ointments until gradually internal wounds healed without any difficulty or problems and superficial lining covered over the cartilage smoothly with no footprint. All the demographic and operative data gathered and recorded.
Results
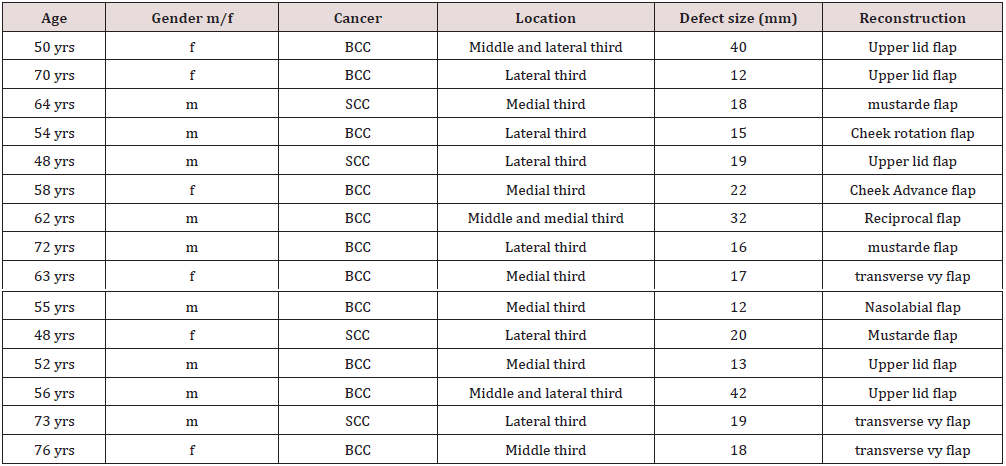
15 patients entered the study completed the questionnaire. 6 patients were women (40%), and mean age was 60.06 years old. Of 15 patients, 3 cases (20%) were SCC, and the others were BCC. As the lesions were categorized according to the medial, middle, and lateral thirds of lower lid, this distribution illustrated in Table 1. All the cartilages harvested from the ipsilateral concha according to the defect size. Overlying coverage completed by local and regional flaps demonstrated in Table 1. The mean size of resulted lining defect length after cancer surgery was 21 mm. according to that sizes cartilage was harvested. Reconstruction of skin defects planned according to general condition of patients and sizer of defect.
SCC: squamous cell cancer; BCC: basal cell cancer.
Discussion
Full-thickness defects following tumor excision of lower eyelid demands comprehensive approaches, as any underestimation in reconstruction may lead to long-term sequels. Skin flaps without structural support may loss its primary shape and contour. Providing all three layers has its own difficulties and failures. Our study illustrated experiences on gradually epithelialization over the grafted cartilage, which is covered with well-nourished skin flaps. This process did not need lining layer via graft or mucosal flaps- which mostly would be resorbed due to flap lossand cartilage survival was guaranteed under proper cutaneous or musculocutaneous flaps. Parodi et al. (2008) presented their experience with Matsuo`s technique on 23 patients with lower eyelid defects and they used remaining conjunctive to cover the cartilage and reported good results in their patients (4). We sutured the rim of remained conjunctiva to the margin of cartilage and let the surface free to be re-epithelialized gradually without complication.
Yamamoto et al. (2017) used oral mucosa and ear cartilage as internal support of lower eyelid reconstruction in 13 patients. After tumor resection, they harvested enough oral mucosa- primarily from inner side of lower lip- and sutured to the conjunctiva [5]. The other processes were the same us. They reported they had not corneal irritation or similar complication. This approach is standard and generally accepted by surgeons, but we omitted the first part of surgery and all conditions that promoted their graft survival, promoted re-epithelialization over our cartilages, too. As discussed by Alghoul et al. (2019) key point in reconstruction of preseptal defects is avoiding inferior vectors of pull, any try to reconstruction, would be less effective, if you do not mind it [6]. We considered that by applying regional skin flaps which diminished long-term retraction and ectropion. Matsuo technique to reconstruct lower lid defects, which had been used by Alves et al. (2012), is commonly accepted [7,8]. Though, chonderitis and conjunctivitis seem to be annoying, and in scare situations caused severe infections, our results again confirmed that providing well-nourished flaps over cartilage may protect it from inflammation and destruction and even sever cornea irritation. Surgeons who are familiar with periorbital skin flaps have proper options to consider during reconstruction, as mentioned by Griffin et al. [9], intact skin in lateral orbit bring you valuable musculocutaneous flaps that prevent future retraction and additional complications. we did accordingly and had the least wound dehiscence after repair. In a study by Liao et al. (2019) on long-term results of autologous auricular graft, they evaluated results in cartilage graft survival following lower fornix contracture reconstruction, and they demonstrated good results in recipient and donor sites [10]. Also, our outcomes were incompatible with their results, and we have not any donor site morbidity. In the conjunctiva we only had few small inflammation treated by local treatments or disappeared spontaneously without intervention.
Conclusion
Lower eyelid reconstruction following tumor excision is of clinical importance, especially in long-term complications. Fullthickness reconstruction as a rule, is generally accepted. Here, we supposed establishment of strong support of auricular cartilage with well- nourished skin flaps which cause good cartilage embedding and re-epithelialization without corneal irritation or sever complication.
Conflict of Interest
None of the authors has a financial interest in any of the products or drugs mentioned in this article.
References
- Quazi SJ, Aslam N, Saleem H, Rahman J, Khan S (2020) Surgical Margin of Excision in Basal Cell Carcinoma: A Systematic Review of Literature. Cureus 12(7): e9211.
- Roostaeian J, Kohan E, Tanna N, Tabit CJ, Kawamoto HK, et al. (2012) Staged reconstruction of the lower eyelid following tri-lamellar injury: a case series and anatomic study. J Plast Reconstr Aesthet Surg 65(1): 48-53.
- Malviya V, Goyal S, Bansal V (2022) Reconstruction of Lower Eyelid with Nasolabial Flap for Anterior Lamella and Turnover Flap for Posterior Lamella. Surg J NY 8(1): e56-e59.
- Parodi PC, Faini G, De Biasio F, Rampino Cordaro E, Guarneri GF, et al. (2008) Full-thickness lower eyelid reconstruction with a conchal chondro-perichondral graft and local coverage with Mio-cutaneous flaps--our divisional experience. J Oral Maxillofac Surg 66(9): 1826-1832.
- Yamamoto N, Ogi H, Yanagibayashi S, Yoshida R, Takikawa M, et al. (2017) Eyelid Reconstruction Using Oral Mucosa and Ear Cartilage Strips as Sandwich Grafting. Plast Reconstr Surg Glob Open 5(4): e1301.
- Alghoul MS, Kearney AM, Pacella SJ, Purnell CA (2019) Eyelid Reconstruction. Plast Reconstr Surg Glob Open 7(11): e2520.
- Matsuo K, Sakaguchi Y, Kiyono M, Hataya Y, Hirose T (1991) Lid margin reconstruction with an orbicularis oculi musculocutaneous advancement flap and a conchal cartilage graft. Plast Reconstr Surg 87(1): 142-145.
- Alves JCRR, Liu RP, Silva Filho AF, Pereira NA, Carvalho EES (2012) Eyelid repair using an autologous conchal cartilage graft. Bras. Cir. Plást 27(2): 243-248.
- Griffin LA, McIntyre BC (2019) Reconstruction of Combined Full-Thickness Defect of the Lateral Canthus and Lateral Upper and Lower Third Eyelids with an Extended Modification of the Fricke Flap, Periosteal Flap, and Conjunctival Flap. Plastic Surgery Case Studies.
- Liao YL, Wu SY, Tsai YJ (2019) Long-Term Results of Autologous Auricular Cartilage Graft Applied in Anophthalmic Orbits Unable to Wear Prosthesis. J Ophthalmol 2019: 7197063.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...