Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Research Article(ISSN: 2641-1709) 
Choanal Atresia Repair, A Comparison Between Transnasal Puncture With Dilatation And Stentless Endoscopic Transnasal Drilling Volume 7 - Issue 3
Salem Farhat1, Abdulbaset Naas1, Amal Abusreweel2 and Najwan Enbaya2
- 1Consultant Otolaryngologist, Tripoli Central Hospital, Libya
- 2ENT Consultant, Tripoli University Hospital, Libya
Received: November 03, 2021; Published: November 15, 2021
Corresponding author: Salem Farhat, Department Of Otolaryngology, Tripoli Central Hospital, Libya
DOI: 10.32474/SJO.2021.07.000266
Abstract
Background: in this study we present the outcome of surgical repair of choanal atresia of 33 patients underwent the surgery at
Tripoli University hospital and Tripoli central hospital
Objectives: The aim of this study to compare between two procedures used to repair choanal atresia. The first procedure is
perforation and dilatation with stenting and the second procedure is endoscopic drilling without stenting. The comparison looked
at the main complication which is restenosis of the choana.
Method: A review the medical notes of 33patients diagnosed with choanal atresia and subjected to surgical repair.
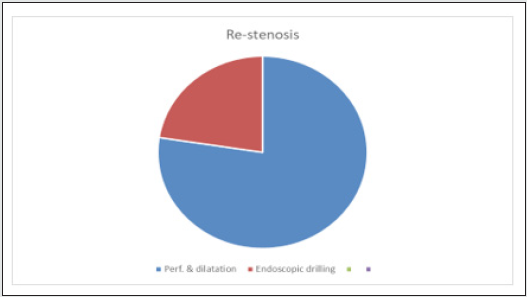
Results: 8 patients out of 13 developed restenosis after treatment with perforation and dilatation (61.5%), While 4 patients out
of 20 treated with trans-nasal endoscopic drilling without stenting (20 %)
Conclusion: The study showed that the risk of restenosis is significantly less in trans-nasal endoscopic drilling technique and
the result of this procedure is comparable to the published data
Keywords: Choanal atresia; endoscopic repair; perforation and dilatation; restenosis
Introduction
Choanal atresia is a rare congenital abnormality. It occurs in 1:5000 – 1:8000 births [1]. Bilateral choanal atresia is an emergency situation and the airway needs to be secured immediately to save the newborn baby+ life. Surgical repair should be planned as soon as possible [2]. Both genders are affected and male to female ratio is 1:2, with 29% of cases are bony and 71% are mixed bony and membranous [3]. Unilateral choanal atresia is more common than bilateral type ( 65-75% of patients have unilateral). Different approaches have been described in the literature. The trans-nasal approach (endoscopic, microscopic, or blind puncture). Curved and straight urethral sounds have been used for puncturing. Endoscopic technique (tans-nasal or trans-palatal) with or without powered instrument offers excellent visualization in removing bony choana [4]. Combined trans-oral trans-nasal is another technique that provides good alternative with easier four handed surgery to ensure adequate posterior choanal repair [5]. CO2 and KTP laser are quick and cause minimal discomfort for the patient and short hospitalization [6]. Vomer removal and use of mucoperiosteal flaps are the main elements for reducing post- operative re-stenosis, as a result of that neither stenting nor Mitomycin C was considered necessary [7]. There is a controversy about use of stenting as stenting can be associated with granulation formation and longer hospitalization. Some surgeons consider placement of stent in all neonates to prevent postoperative obstruction [8]. Carter et al. found that topical Mitomycin C to be efficacious adjuvant therapy in endoscopic choanal atresia repair and associated with reduction in formation of granulation tissue and rate of stenosis and number of surgeries [8]. Near total endoscopic removal of the bony septum provides long-term nasal patency for revision CA/stenosis repairs. The endoscopic ‘common choanae’ technique is aided by trans- nasal and transoral telescopic visualization with precise microbrewer removal of the bony septum [9]. No significant difference in surgical outcome as the rate of restenosis was 42.9% with stent and 47.4% without stent [10]. In Tripoli and until the year 2005, trans-nasal perforation and dilatation with stenting was the standard approach to treat choanal atresia. With the introduction of endoscopic sinus surgery by the end of 2005, the endoscopic approach started to take over. In this study we will review both approaches looking at the main complication which is restenosis of the choana after surgery.
Materials and Methods
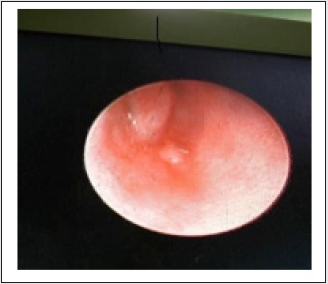
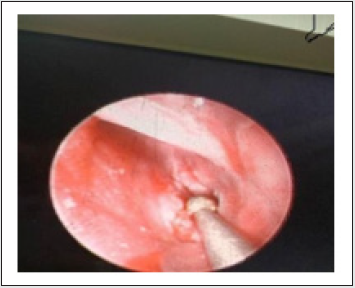
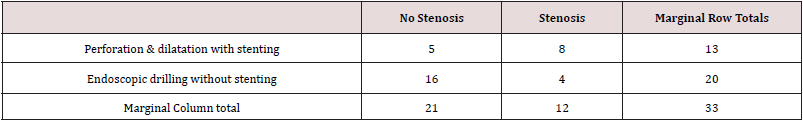
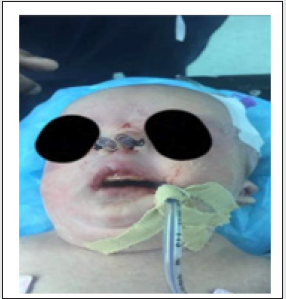
A total of 33 patients with choanal atresia were included in the study. They were treated surgically by either tans-nasal perforation and dilatation with stenting or trans-nasal endoscopic drilling without stenting. The age of the study group ranges from 3 days to 18 years. 8 patients were males (24%), and 25 patients were females with ratio of 1:3 respectively. 24 cases diagnosed with bilateral choanal atresia and 9 with unilateral. Diagnosis of choanal atresia was confirmed endoscopically and radiologically. All patients had a bony component of the atresia. The group of patients who underwent trans-nasal perforation & dilatation using a metallic perforator and urethral sounds are stented and the stent left in place for 6 weeks. They treated with saline irrigation and suction to keep them patent. In the trans-nasal endoscopic group. 2.7- and 4-mm kinescopes were used, and the nasal cavity was prepared with decongestant. The atretic plate is opened using a drill after elevating lateral based muco-periosteal flap. The posterior part of the septum was removed, and no stent inserted. Patients of both groups were discharged within 2-4 days. Follow up arranged every other day for one week, weekly for one month and monthly for one year. Bilateral choanal atresia patients were referred from paediatric department and underwent the surgical repair within few days after birth. Unilateral cases presented with nasal obstruction which is worse with upper respiratory tract infection. 10 years old boy presented with heavy snoring and obstructive sleep apnea confirmed by sleep study. The boy also developed cardiac symptoms, investigated and referred for surgery by paediatric cardiologist. He underwent a successful endoscopic repair of left choanal atresia and adenoidectomy. Postoperative sleep study showed normal result (Figures 1 & 2).
Complications
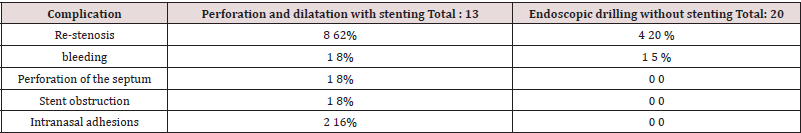
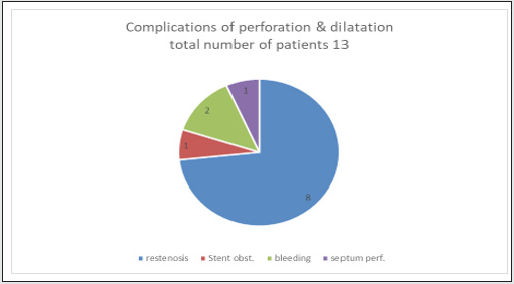
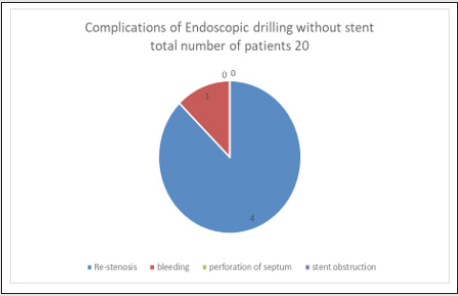
(Table 1) The aim of the surgery is to open the choana and keep it patent, hence restenosis is the most worrying complication. It occurred in 8 out 13 patients underwent trans-nasal perforation and dilatation (62%). 4 out of 20 patients underwent trans-nasal endoscopic drilling. All patients with re-stenosis required revision surgery. In trans-nasal perforation and dilatation group, only one patient (8%) had significant bleeding and treated conservatively. One patient (8%) developed septal perforation as a result of surgical repair (Figures 3-5). One patient (8%) had obstructed stent and treated conservatively. Two patients (16%) of this group had postoperative intranasal adhesion required surgical division. In the trans-nasal endoscopic drilling group, only one patient (5%) developed postoperative bleeding. No one had a perforated septum or intranasal adhesions.
Statistical analysis
Statistical analysis for restenosis as a complication of the two different procedures was carried out using Fisher exact test with a significant level of P < .05. The Fisher exact test statistic value: 0.0265. This indicates that there is a significant difference between the two procedures in terms of postoperative restenosis of the choana.
Easy Fisher exact test
The Fisher exact test statistic value: 0.0265. The result is significant at p < .05 (Table 2).
Discussion
Although choanal atresia is a rare abnormality but surgical intervention is always required in neonates with bilateral atresia. Unilateral cases usually present later in life. The success of surgical intervention is mainly measured by minimal or absent postoperative complications, namely lower incidence of restenosis [11]. Different techniques of repair have been described in literature with different outcome. Transnasal surgery involves using drill which can be controlled endoscopically in different ways , either using 0-degree alongside the instrument within the nose or using 120-degree through the mouth and looking at the nasopharynx [11]. KTP laser can be used but it has no clear advantage [12]. Restenosis is the most challenging complication of the repair. Repeated dilatation after surgery and for few weeks may help to achieve good results. Use of balloon for dilatation will give less shearing effect rather than use of urethral dilators [12]. Mithomycin C inhibits fibroblasts and may have a role in reducing fibrous tissue formation. The evidence of its efficacy is limited [12,13]. Whether stenting has any effect is still controversial [12]. Stents are very useful in providing guaranteed airway for infants during the obligate nasal breathing period, so it is reasonable to use them in infants with bilateral atresia for 6 – 8 weeks [14,15]. The transnasal perforation with stenting was the standard procedure in Tripoli hospitals until the year 2005 when endoscopic sinus surgery introduced. From that time transnasal endoscopic procedure started to take over. Now almost all the cases are carried out using transnasal Stentless endoscopic drilling with raising mucoperiosteal flap and excision of the posterior part of the nasal septum (Figure 6).
Conclusion
Stentless transnasal endoscopic drilling combined with resection of the posterior part of the septum has proven to be more efficient procedure, gives better visualization of the surgical field and less incidence of complications. Statistically, it is proven to cause less restenosis compared to transnasal perforation & dilatation.
Acknowledgement
None
Conflict of Interest
The authors confirm no conflict of interest.
References
- JD Ramsden, P Compisi, V forte (2009) Choanal atresia and Choanal stenosis. Otolaryngology Clinic of North America 42: 339–352.
- TN Reddy, SN Dutt, M Raza (1996) Emergency management of bilateral choanal atresia in newborn by endoscopic endonasal approach. Int Journal of paediatric Otolaryngology 38(1): 21-30.
- OE Brown, P Powell, SC Manning (1996) Choanal atresia: a new anatomic classification and clinical management applications. Laryngoscope 106: 97-101.
- Assanasen P, Metheetrairut C (2009) Choanal atresia. J Med Assoc Thai 92(5): 699-706.
- H Abolezz, T Yousef (2011) Combined trans-oral trans-nasal approach in the repair of posterior congenital choanal atresia, clinical experience. J Otolaryngology Head and Neck surgery 40(3): 271–276.
- Prasad M, Ward RF, April MM, Bent JP, Froehlich P (2002) Topical mitomycin as an adjunct to choanal atresia repair. Arch Otolaryngol Head Neck Surg 128(4): 398-400.
- Karligkiotis A, Farneti P, Gallo S (2017) An Italian multicentre experience in endoscopic endonasal treatment of congenital choanal atresia: Proposal for a novel classification system of surgical outcomes. J Craniomaxillofac Surg 45(6): 1018-1025.
- Carter JM, Lawlor C, Guarisco JL (2014) The efficacy of mitomycin and stenting in choanal atresia repair: a 20-year experience. Int J Pediatr Otorhinolaryngol 78(2): 307-311.
- Cedin AC, Fujita R, Cruz OL (2006) Endoscopic transeptal surgery for choanal atresia with a stentless folded-over-flap technique. Otolaryngol Head Neck Surg 135(5): 693-698.
- Kim H, Park JH, Chung H, KIM DY, Lee GH (2012) Clinical features and surgical outcome of congenital choanal atresia: factors influencing success from 20 years review in institute. Am J Otolaryngol 33: 308 – 312.
- Fredman NR, Michell RB, Baily CM, Albert DM (2000) Management and outcome of choanal atresia correction. International J of paediatric Otolaryngology 52(1): 45-51.
- Kubba H, Bennett A, Baily CM (2004) Un update of choanal atresia surgery at Great Ormond Street Hospital for Children: Preliminary results with Mithomycin C and LTP Laser. Int Paediatric Journal of Otolaryngology 68(7): 939-945.
- Corrales CE, Kotali PJ (2009) Choanal atresia, current concepts and controverses. Current opinion Otolaryngology and Head & Neck surgery 17(6 ): 466–470.
- Ibrahim AA, Magdy EA, Hassab HM (2010) Endoscopic Choanoplasty without stenting fo congenital choanal atresia repair. Int Journal of Paediatric Otolaryngology 74(2 ): 144–150.
- Teisser N, Kaguelidou F, Coubigher V, Francois M (2008) Predictive factors for success after transnasal endoscopic treatment of choanal atresia. Arch Otolaryngol Head Neck Surg 134(1): 57–61.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...