Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Case Report(ISSN: 2641-1709) 
Cervicofacial Herpes Zoster Complicating Ganglion- Pulmonary Tuberculosis: Case Report and Review of the Literature: A Case Report Volume 7 - Issue 1
Mohamed Ali Gliti1,3*, Houda Boudinar1,3, Sophia Nitassi2,3, Bencheikh Razika2,3, Benbouzid Mohamed Anas2,3, Abdelilah Oujilal2,3 and Leila Essakalli Houssyni2,3
- 1Resident Physician in Otorhinolaryngology, Department of Otorhinolaryngology, Head and Neck Surgery, Ibn Sina University Hospital, Morocco
- 2Professor of Otorhinolaryngology, Department of Otorhinolaryngology, Head and Neck Surgery, Ibn Sina University Hospital, Morocco
- 3Faculty of Medicine and Pharmacy of Rabat, Mohammed V University, Morocco.
Received:June 18, 2021; Published:June 29, 2021
Corresponding author: Mohamed Ali Gliti, Department of Otorhinolaryngology and Cervicofacial Surgery Specialty Hospital, Rabat, Morocco
DOI: 10.32474/SJO.2021.07.000252
Abstract
Tuberculosis is an infectious disease; it has a variable degree of presentation, most often pulmonary while the extrapulmonary location is dominated by lymph node involvement, especially cervical. On the other hand, herpes zoster results from the reactivation of the virus that causes varicella. Here, we report the case of cervicofacial herpes zoster complicating ganglion-pulmonary tuberculosis in a 19-year-old female patient with a history of varicella during childhood, who presents bilateral lymphadenopathy, the diagnosis of pulmonary and lymph node tuberculosis is confirmed by histology, she has treated with anti-tuberculosis drugs and the evolution was marked by the presence of lymphadenopathy and the appearance of cervicofacial herpes zoster.
Introduction
Tuberculosis remains a major infectious scourge, particularly in developing countries. In 25% of cases, the location of tuberculosis is extra-pulmonary, the cervical lymph node involvement of which is the most frequent. Tuberculous lymphadenopathy is most often unilateral, single, and isolated. Cervical localization is by far the most frequent [1-3]. Lymph node tuberculosis is an advanced form of tuberculosis, always preceded by a primary pulmonary infection. The causative bacterium is called Mycobacterium tuberculosis or Koch’s bacillus [1]. On the other hand, herpes zoster infection is a painful rash along a nerve or nerve ganglion. These rashes occur as a result of the reactivation of the virus that causes varicella [4]; the varicella-zoster virus (VZV) most often affects the chest or face. We report the case of ganglion-pulmonary tuberculosis complicated by cervicofacial herpes zoster.
Case Report
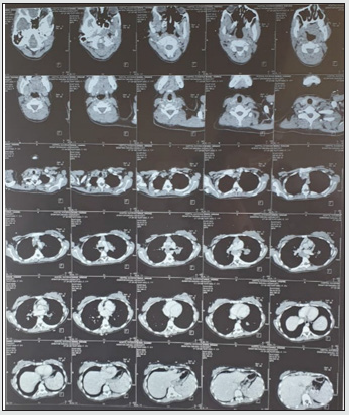
Four months ago, a 19-year-old patient with a history of normochromic normocytic anemia, varicella during childhood, suffers from dyspnea stage 3; productive cough, weight loss, night sweats, right and left submandibular swelling. On clinical examination, we find lymphadenopathy of the territory 2 and 3 bilateral, mobile to the two planes, painless, and the largest of which on the left measures nearly 2 cm. The rest of the clinical examination was unremarkable. Radiologically, the chest x-ray showing a left para-hilar opacity; Thoracic CT had demonstrated heterogeneous supra and subdiaphragmatic polyadenopathies with pulmonary parenchymal involvement and nodular splenomegaly, suggesting primarily granulomatous involvement with the cervical ultrasound showing bilateral polyadenopathy of territory 2 and 3. In addition, the search for BK in the sputum is positive. Histologically, a cervicotomy was performed, suggesting an inflammatory granulomatous necrotizing reaction compatible with a tuberculous origin. The diagnosis of pulmonary and lymph node tuberculosis was retained. The anti-tuberculosis treatment was started according to the 2RHZE and 7RH protocol. The evolution was marked by the persistence of the right and left cervical lymphadenopathies; a cervical-thoracic-abdominopelvic CT (Figure 1) for control showing supra and sub-diaphragmatic lymphadenopathy with hepatomegaly and nodular splenomegaly forming part of a granulomatous involvement, cervical ultrasound shows hypoechogenic globular polyadenopathies including only one partially calcified of the right basi-cervical site, and the appearance of vesicular lesions (Figure 2), suggesting primarily a right cervicofacial zoster on the same side lymphadenopathy.
Discussion
Infection of the human body with VZV consists of three phases starting with the primary infection where the virus enters the body through the lining of the upper airways (nasopharynx) and oropharynx. It multiplies and then spreads in the body by a first viremia. The virus replicates locally in the respiratory tract and the lymph nodes, then reaches the reticuloendothelial system. The specific immune response develops, a second viremia disseminates the virus in the whole organism and brings it to the level of the skin (vesicular lesion appears), the latency phase follows the recovery of varicella. It is characterized by the persistence of viruses in the sensory ganglia of certain spinal nerves and or cranial and settles in a quiescent state. The mechanism by which the virus remains in the latent state is very imperfectly known [5]. In this phase, there is no clinical manifestation. The virus reactivation phase occurring due to immune deficiency is common in elderly subjects and in pathological situations affecting the immune system [6,7], such as in our case, tuberculosis, which leads to a decrease of immunity. It is transmitted by the sensory nerve to the epidermis to give localized shingles infection. Concerning the relation between herpes zoster and tuberculosis, Arvid Wallgren concluded that tuberculosis in one way or another predisposes to herpes zoster by the action of its toxins on the spinal ganglia. In a group of 10 patients, 7 cases present with tuberculosis disease or infection, and the remaining 3 cases which were tested for tuberculin were not attempted [8]. The frequency of herpes zoster in tuberculosis patients was demonstrated in 21 autopsies. Head and Camlbell encountered 5 times extensive pulmonary tuberculosis and 5 times milder tuberculosis lesions [9]. ARNSTEIN finds that in half of the cases where the autopsy reveals an alteration of internal organs, there is a combination of herpes zoster with tuberculosis. He believes that the chronic irritation of the spinal ganglia by tuberculous toxins promotes the outbreak of disease [10]. MAGNUSSON, from Reykavik further expresses the opinion that tuberculosis or tuberculosis toxins can give rise to herpes zoster infection [11]; Furthermore, Arvid Walgren believes that the herpes zoster pattern corresponding to the location of the tuberculous lesions shows that the majority of his patients had the same site of herpes zoster as the tuberculous lesions.
Conclusion
The association of herpes zoster infection and tuberculosis has already been mentioned in some studies; moreover, its cervicofacial location and a lymph node form of tuberculosis have been reported in our case. Many studies have described Herpes zoster infection complicating tuberculosis. However, and to the best of our knowledge, an association of cervicofacial herpes zoster and lymph node form of tuberculosis hasn’t been reported yet in the literature, hence the rarity of our case.
References
- Zaatar R (2009) Tuberculos lymphonodale cervicale : prise en charge diagnostique et thé Annales d’otolaryngologie et chirurgie cervico-faciale 126: 250-255.
- Bennamane K (2014) La tuberculose ganglionnaire à propos de 20 cas. Aspect clinique, thérapeutique et é 18ème congrès de pneumologie de langue française-Marseille.
- llgazll A (2004) Extrapulmonary tuberculosis: Clinical and epidemiologic spectrum of 636 cases. Arch Med Respir 38: 435-441.
- Laurent R (2005) Varicelle-Zona. EMC-Médecine 2(3): 276-283.
- Rentier B, Sadzot-Delvaux C (2000) le virus de la varicelle et du zona dans le systéme nerveux : retraite silencieuse ou guérilla permanente ? Revue virologie 4(3) : 207-2016.
- Senneville E (1998) Infections à VZV :forme de l’adulte sain et de l’immunodéprimé. Méd Mal Infect pp. 791-799.
- Arvin AM (1996) Varicella-Zoster virus. Clin Microbiol Rev 9(3): 361-381.
- Arvid Wallgren (1929) Considérations cliniques sur quelques problémes que souléve l’herpés zoster. Zona et varicelle; Zona et tuberculose. Acta pediatrica 8(3): 241-276.
- Head Et campbell (1900) Brain. T 28 pp. 353.
- Arnstein (1922) wien. Arch f inn Med T 4. pp. 441.
- Magnusson (1925) Hospitalstidende. T 68 pp. 265.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...