Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Case Report(ISSN: 2641-1709) 
Auditory Training for Post lingually Deafened Adults Cochlear Implant Users Volume 5 - Issue 5
Paula Saidi* and Nerea Ortega Castro
- Department of Audiology, Master of Clinical Audiology and Hearing Therapy, University of Isabel I, Spain
Received: January 21, 2021 Published: February 03, 2021
Corresponding author: Paula Saidi, Department of Audiology, Master of Clinical Audiology and Hearing Therapy, University of Isabel I, Spain
DOI: 10.32474/SJO.2021.05.000225
Abstract
Difficulty in speech discrimination is a major complaint among post lingually deafened adults, which are cochlear implant (CI) users. Consequently, it is important to study the factors that offer positive post-operative outcomes in order to get the most out of this technology. Thus, many clinicians tend to orient the implanted toward the auditory training program with the aim of teaching them to make perceptual distinctions about sounds that are presented systematically. Therefore, a systematic review was performed to examine the influence of aural rehabilitation on post lingually deafened cochlear implant users’ speech recognition with an eye towards reaching its full potential. A total of 20 articles was used in this review, chosen from PubMed, Science Direct, semantic scholar, international journal of audiology, and journal of speech, language, and hearing research. It was therefore concluded from the analysis of the previous studies that the auditory training may be advantageous when it considers the individual’s own characteristics towards designing a proper auditory training program while tracking his/her progress throughout this period. Furthermore, choosing between clinician-directed training and computer-based home training or a combination of both is essential, considering the patient and the clinician’s preferences. Not to mention the high importance of choosing a processing strategy that helps differentiate between the sound cues. It may also be beneficial to train the cochlear implant users on environmental sound identification as well as speech recognition or speech tracking to recognize them better. Auditory rehabilitation could be more valuable when provided in the long-term and when conducted in more realistic situations that resemble real-life environments. In order to achieve the desired results, future studies should focus on sample size adjustments, including less heterogeneity among the participants, while conducting long-term training suitable for each patient along with the proper processing strategy.
Abbreviations:CI: Cochlear Implant; HINT: Hearing in Noise Test; SPIN: Speech in Noise; GBI: Glasgow Benefit Inventory; BKB: Bamford-Kowal-Bench; SNR: Signal-to-Noise Ratio; VDS: Visual Digit Span; ADS: Auditory Digit Span; VER: Vocation Emotion Recognition; MCI: Melodic Contour Identification; FEST: Familiar Environmental Sound Test; CNC: Consonant-Nucleus-Consonant; NNSE: Neural Network based Speech Enhancement
Introduction
Cochlear implantation has been an enormous breakthrough in treating severe to profound hearing loss in patients that cannot benefit from conventional hearing aids [1]. The cochlear implant is an electronic device that bypasses the normal hearing pathway and the damaged cochlea and directly stimulates the auditory nerve of a hard-of-hearing patient [2]. A strong commitment to rehabilitation therapy is needed for the purpose of hearing impairments treatment since the cochlear implant is not by itself sufficient nor efficient for complete recovery [3]. Therefore, auditory training is indispensable for this purpose; it is mainly employed in order to enhance the listener’s ability to focus and distinguish sounds, especially against background noise. It is important to initiate such training immediately after the fitting of the implant, which will include a series of exercises. The aim of this intervention technique is to train the mind on sound perception and uses and to provide awareness and recognition techniques for the brain’s auditory neurons as well as improving the listening skills. Hence, repetitive exercises and continuous training are needed so that the employed auditory training shall achieve their purposes and goals for the sake of the listener’s proper and organized hearing. As mentioned, it is preferable to initiate the training after the patient has acquired the implant, which will help him maximize its benefits, enhance his understanding of speech, and develop the needed skills to differentiate and recognize different sounds. The auditory rehabilitation also has several other benefits, such as empowering the patient’s social skills through communication enhancement and allowing the patient to relate sound to their social and convenient meaning [4].
Despite extensive research on the importance of auditory training after the implants, the percentage of referred patients to the training or to listening therapy remains relatively low. These patients are rather left on their own to adapt and acquire the necessary skills to support the implant’s benefits. Obviously, every patient, following his cochlear implant, will be needing different types of aural rehabilitation as well as different intensities and a number of sessions for ultimate results [4]. For this purpose, it is necessary for the audiologist to determine the skills already existent for the patient, and then plan, accordingly, the number and types of sessions needed to assist the patient. When highlighting the importance of auditory training, it is worth mentioning that the implant serves the patient in treating his hearing impairment, and not his communication skills and social adaptability. In other words, the purpose of cochlear implants is the restoration of audibility, leaving the patient unsatisfied with his inability to engage and communicate properly in his social environment. Several studies have shown that, as cochlear implants improve the auditory experience of the patient, it failed to restore speech recognition, especially in complex auditory contexts. Therefore, the implant is the first initiative towards a cascade of steps and activities to reach desirable results, where the patient does not only detect sounds, but he also organizes them, prioritizes them, and recognizes them. This process renders the patient able to perform adequate and efficient communication, not only hearing, with his surroundings. All light must be shed on the importance of efficient auditory rehabilitation in helping patients acquire social and communication skills [5].
Hearing impairments and difficulties are major contributors to physical and psychological deterioration represented by social isolation, depression, and brain atrophy. Those who are not able to properly communicate and express themselves in society will suffer not only from their physiological barrier but will also perceive themselves as an excluded individual in social events, gatherings, and even throughout their professional lives. Successful communication is one of the factors that designates the success of auditory training and highlights its necessity and impact on the patient’s life. Consequently, extensive, and further research is needed to present evidence-based conclusions showing the impact and efficacy of auditory training not only in physiological auditory terms, but also in social and psychological contexts. This paper depicts a systematic review based on previous studies discussing different types of auditory trainings, their impact on physiological and social skills, and their advantages, as well as their limitations, for the post lingually deafened adults cochlear implant users. Post lingually deafened cochlear implant users are patients who lost their hearing after language acquisition, showing no benefit from hearing aid usage [1].
Objectives
The objective of this study is to examine the positive outcomes of aural rehabilitation among adult post lingually cochlear implant users for the sake of maximizing the device’s performance. The latter serves the patient not only in physical aspects, but it also improves his/her communication capacities, with as minimal limitations as possible.
Methodology
A literature review was conducted in order to study the effects of auditory training in enhancing and improving speech perception in noisy environments upon post lingually deafened adult cochlear implant users. A systematic approach was adopted to select reliable and convenient resources for appropriate results. At first, the keywords used to initiate research on the mentioned topic were the following: “Auditory training”, “cochlear implant” and “adult” using the following platforms: PubMed, Science Direct, semantic scholar, international journal of audiology and journal of speech, language, and hearing research. Accordingly, a significantly high number of articles was found. Using PubMed, 430 articles were found, whereas using Science Direct, 1,569 articles were obtained. Using semantic scholar, a number of 2,060 articles were found. Searching via the international journal of audiology, 220 articles were found, and 290 articles with the journal of speech, language, and hearing research. Overall, a total of 4,569 articles was found from all the platforms used. Accordingly, inclusion and exclusion criteria were set in order to either select or exclude articles based on relevant information for the specific research. First of all, it was found more convenient to study articles with the most recent findings and methodologies since the field of auditory training is highly evolving. Therefore, articles that were published since 2005 were selected. In other words, articles dating back before 2005 were excluded from the study. Second of all, in order to ensure the adequacy of the information provided and its significance to the literature review, few authors were selected upon their credibility according to credentials and related achievements. For example, authors who were most directly related to the audiology field in general and experienced in auditory rehabilitation in specific were selected. Moreover, a more detailed approach was used in order to select articles not based only on external factors such as dates, authors, and peer review, but more importantly on the content of the article (strategy of the methodology used) as well as its relevance to the objectives of the study and the outcomes expected. Hence, a total of 20 articles were found to follow the same clinical strategies represented by:
a) Phase 1: Pretraining of the selected population (adults with cochlear implants).
b) Phase 2: Performance of auditory training for the sample.
c) Phase 3: Testing of outcomes (post-training phase).
The process of review of articles selection is detailed in Figure 1. Other articles were selected to ensure reliability and credibility: Six literature review articles, one article that followed a survey on 230 cochlear implant audiologists to investigate the efficiency of the adopted auditory training practices and to evaluate its outcomes, and one article that conducted auditory training on one patient over an extended period of time while measuring the outcomes. All articles were carefully reviewed and analyzed based on concluded results, adopted study designs, indicated protocols, and relevant findings to the review. Finally, 20 articles were actually studied to reach the goal of the study and investigate the effects of auditory training in the improvement of listening skills, recognition, interpretation of speech sounds, as well as the selection of acquired speech in noisy environments among cochlear implanted users in the post lingually deafened adult population.
Results
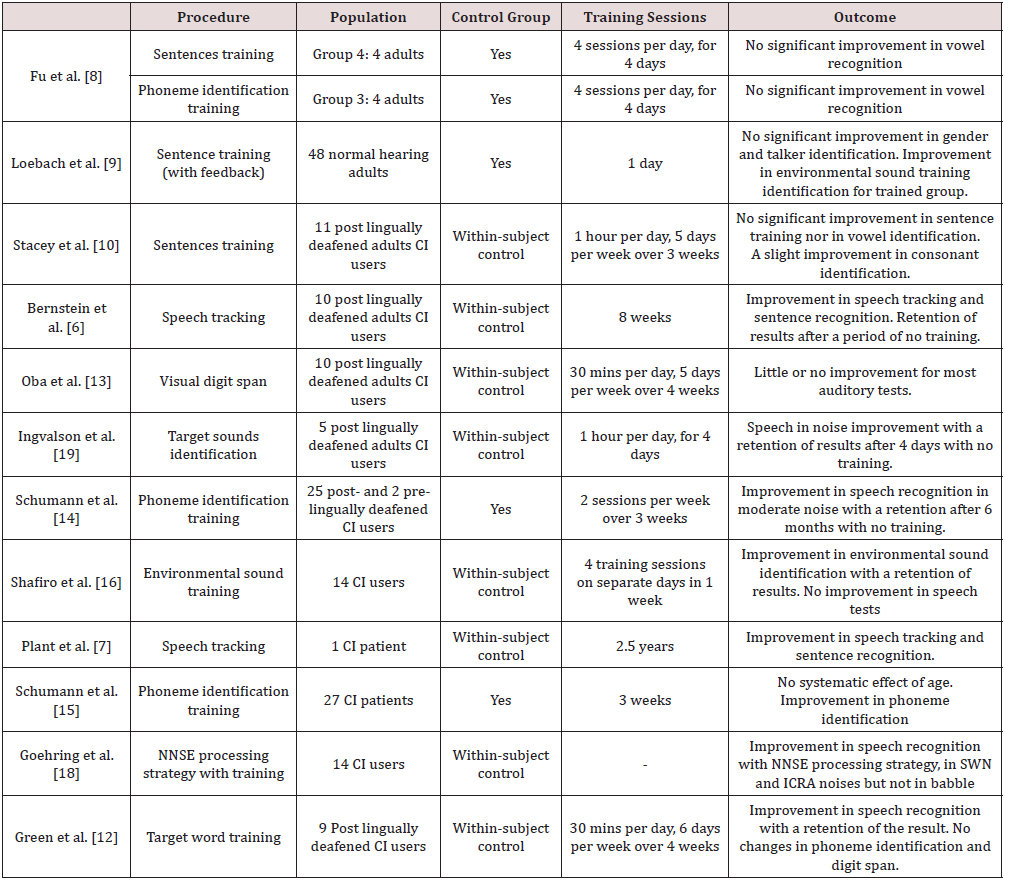
Different training techniques were used in previous studies. The following paragraphs present each training method with the results obtained after its completion (Table 1), a method of training selection (the listening cube), as well as the differences of results observed with computer-based home training and cliniciandirected clinical training.
Speech tracking
Bernstein et al. [6] investigated post-training outcomes for a group of ten post lingually cochlear implant adults after four weeks of speech tracking training and eight weeks after training completion, using sentence recognition tests, and tracking rate measurement. In addition, Plant, Bernstein, and Levitt [7] used the KTH speech tracking method for a 51-year-old woman for 2.5 years. In both experiments, a significant improvement for both tracking rate and speech recognition was observed.
Sentences training
Fu, et al. [8], Loebach, et al. [9], and Stacey et al. [10] trained the participants in their studies using Hearing in Noise Test (HINT) sentences, Harvard (IEEE) sentences, and low predictability speech in noise (SPIN) sentences. The participants were asked to identify specific keywords in the sentences acoustically presented. Fu, Galvin, et al. [11] in group number 4 that includes four normal-hearing adults, used modified connected discourse sentence training using HINT sentences by a single-talker, presented with spectrally shifted speech, same as for a cochlear implant patient having a limited number of electrode with a small length of electrode array. This training aims to imitate normal daily listening situations. The participants’ speech recognition was tested before the training, after each training session, and after finishing the training sessions (day 5) using multi-talker vowel and consonants recognition, processed with eight channels, shifted and unshifted. There was no significant improvement in the spectrally shifted speech recognition in this group after the sentences training. As for Loebach et al. [9], training was conducted on 48 normal-hearing adults divided in two: 24 in the control group using unprocessed version of IEEE sentences with no feedback after the response, and 24 patients in the experimental group using processed sentences with a presentation of feedback after their response. The performance in the posttest using the sentences with no feedback nor repetition, and the environmental sound identification for both groups was improved, better for the trained group than for the control group. However, the training did not improve the participants’ ability of gender identification and talker discrimination. Conducting experiments on 11 post lingually deafened adults with the cochlear implant, Stacey et al. [10] performed training using IEEE sentences, low predictability speech-in-noise (SPIN) sentences as well as word training task. A within-subject control procedure was used starting with baseline testing, one week on training followed by testing and Glasgow Benefit Inventory (GBI) questionnaire for a duration of three weeks.
Testing and training were performed at home. The testing was conducted using the IEEE sentences test, vowel and consonant identification, Bamford-Kowal-Bench (BKB) sentences test, and GBI questionnaire. After three weeks of auditory rehabilitation, a significant improvement in consonant identification was observed, which is not the case for the IEEE sentences test, BKB sentences test, and vowel identification. Moreover, Green, Faulkner, and Rosen [12], in their experiment trained nine post lingually deafened adults with a cochlear implant, using home training 30 mins per day, and six days per week for a duration of four weeks. Three training texts were utilized, each one divided into phrases of two to ten words, containing one to four target words to identify in 20-talker babble. The testing was represented by sentence recognition in babble using BKB sentences and IEEE sentences at a different signal-tonoise ratio (SNR), modified according to the answer, vowel and consonant identification in noise and memory span for digits forward and backward. Four pretests over three sessions took place (one in quiet and three in noise), followed by home training with a total of 12 hours training at different SNR based on the performance, then post-training testing in noise after the last day of training with final testing in noise four weeks later. A significant improvement in sentence recognition in noise was obtained, which was absent in phoneme discrimination and in forward and backward digit span. In addition, the speech recognition threshold was lower in post-training than the one obtained in the pre-training, and it was maintained or improved four weeks after finishing the training.
Visual digit span training
Oba, et al. [13] carried out their experiment using visual digit span training with feedback presentation, a non-auditory training method, to study its effect on auditory perception for ten post lingually deafened adults with cochlear implants. A within the subject control procedure was done, represented by a baseline testing prior training, home training for 30 minutes per day, five days per week for a period of four weeks, and post training measurements within the training period, after five training hours and ten training hours, and after one-month post-training. Visual digit span (VDS), auditory digit span (ADS), speech recognition in quiet (vowel and consonant identification), speech recognition in noise (HINT sentences in steady noise, HINT sentences in babble, digits in steady noise, and digits in babble), vocation emotion recognition (VER) and melodic contour identification (MCI) were the tests performed in free field with 65 dB loudspeaker. The results obtained show no improvement for ADS, phoneme recognition in quiet, HINT sentences recognition, and digits recognition in noise. However, there are small improvements for VER and MCI only.
Phoneme identification training
Fu, et al. [8], Schumann, et al. [14]; Schumann, et al. [15] trained their participants in their experiments using phoneme identification task. Fu, et al. [11] carried out vowel contrast training in monosyllabic words for group 3 (four normal-hearing adults) in their experiment, starting with baseline testing, five days of training, each session followed by vowel identification test, and posttest using vowel and consonant recognition testing with eight channels spectrally shifted and unshifted speech. The stimuli and the talkers were different between the testing and the training. Subjects in this training did benefit from this procedure, showing an increase in their overall phoneme recognition ability. On the other hand, Schumann et al. [14] and Schumann et al. [15] conducted their experiment on 27 adult cochlear implant users, divided into training group (15 patients) and control group (12 patients). The training group procedure starts with a pretest session, six training sessions, and a post-training test followed by a follow up after six months. However, the control group was exposed to a test-only procedure, pretest, and posttest, with a four-week interval. For the training, they used target sounds using non-sense syllables in a quiet room. The testing sessions included evaluations of sentence recognition in two conditions: with moderate noise (SNR: +5db) and in a difficult, noisy environment (SNR: 0dB). No significant improvement for the control group between pre and posttest in sentence recognition. However, the training group showed a significant amelioration in post-training only at the level of +5dB SNR that was improved after six months from the completion of the training. Vowel and consonant identification improved with better improvement for consonants.
Environmental sound training
Shafiro, et al. [16] studied the effectiveness of home-based computerized environmental sound training on environmental sound and speech perception in 14 cochlear implant users. Two pretesting sessions were performed in the laboratory prior to any training (within the subject control). After finishing the pretest, four sessions of computer-based training, along a period of one week, was conducted by the patients at home. The training stimulus was presented based on the patient’s performance in the pretest. A posttest in the laboratory was conducted after training completion, followed by a retention session one week after (no training). To evaluate the patient’s performance before training, in pretest 1, BKB-SIN test (sentence perception at a varying signal to noise ratios), familiar environmental sound test (FEST), consonantnucleus- consonant (CNC) monosyllabic word recognition test, and speech in noise (SPIN-R) sentence test were performed for all the participants. In pretest 2, post-training test and retention, the same tests were performed as in pretest 1, except for the BKB-SIN test that was only conducted in pretest 1. After training, FEST scores improved significantly and was maintained after one week of training completion. Moreover, an improvement in tokens not used in training was also obtained with no improvement for either of the two speech tests.
Listening cube training
De Raeve et al. [17] explained a three-dimensional auditory training program developed during the clinical practice at the KIDS Royal Institute for the Deaf in Belgium for children and adults with cochlear implants. In this article, they did not conduct an experiment on patients, but they gathered reports from many institutes using the listening cube training to study its efficiency. This tool helps the therapist plan and structure an effective yet adequate auditory training regimen specific to each individual’s needs. It is a three dimensional training due to the fact that it includes the level of perception, the practice materials, and the practice conditions. The therapists using the listening cube training tool provided positive feedback showing successful results after using this method.
Sentence keyword training with an integration of the NNSE algorithm
The integration of Neural Network based Speech Enhancement (NNSE) algorithm in the cochlear implant speech processing strategy was performed along with the training. It aims to improve speech perception in noisy environment for cochlear implant users. Goehring et al. [18] performed their study on 14 Dutch speaking cochlear implant users (ACE strategy). Each patient serves his own control. The training is a group of sentences from LISTm corpus, presented in quiet and in noise until obtaining the most comfortable level to be fixed for the patient during the procedure. Speech in noise test was measured using three different background noises (Speech-weighted noise SWN, speech-like modulated noise with silent intervals limited to 250ms ICRA5-250 and babble) in three processing conditions (unprocessed condition: ACE strategy, NNSE-single-talker ST: same single-talker in test and training, and NNSE-multi-talker MT: multiple talkers excluding the target speaker), so each patient is tested in nine conditions. The SRT for the unprocessed condition was higher than the other conditions for all of the three types of noises. However, NNSE-ST provided the lowest SRT for all of the three noises.
Computerized home-based training vs clinician-directed training
Ingvalson, et al. [19] and Green et al. [12] investigated the effectiveness of home-based training using a computer. There was an improvement following the training, which is dependent on the training used. Zhang, et al. [20] investigated nine computerized home-based auditory training programs. Their research highlighted the efficiency of those trainings, especially for recipients who cannot afford clinician-directed training. It is also more convenient for the clinician because it requires a high number of sessions over an extended period of time. Völter, et al. [21] examined the efficiency of different computer-based home training programs. The result suggested that it can provide positive outcomes for cochlear implant users. However, Bernstein et al. [6] and Plant et al. [7] conducted their experiment using clinician-direct training. A significant improvement in both studies was obtained, highlighting the importance of face-to-face interaction to avoid boredom as well as the effect of positive affirmations and feedback along with the encouragement given by the clinician to the patient.
Discussion
The aim of this systematic review was to test the hypothesis which states that aural rehabilitation is an effective procedure to assist post lingually deafened adults, cochlear implant users, developing the ability to associate the sounds received by the processor with their corresponding meanings, especially within noisy environments. A huge uncertainty is still in existence regarding the most effective type of training, the adequate number of sessions, and the appropriate general duration of the program.
Designing an auditory training program
Many training methods used in the analyzed articles provided, to some extent, a significant improvement in the speech in noise perception. However, the amount and time course of development differed among patients. Therefore, it is required to develop a suitable training plan specific to each individual, considering his computer education, personality, motivation, linguistic knowledge, processor characteristics, financial status, age, family support, medical condition, duration of deafness, duration of the implant as well as his level of performance, while adapting the training’s difficulty level accordingly. Based on those criteria and once the areas of difficulty are found, the patient will be given an adequate training procedure, computer-based home training or cliniciandirected, or a combination of both. Note that for elderly patients, it is recommended to test their cognitive function, and if declined, it can impede the success of auditory training [4].
Clinical-directed training or computer-based home training.
For an adult with less experience with computer devices, it is easier to conduct the training with the clinician. Moreover, it is less boring due to the interaction with the therapist as well as the encouragement and immediate feedback that enhances the patient’s motivation [7]. One pitfall of clinician-directed training is its high cost compared to computer-based home training. In addition, when training at home, the patient has the luxury to train at his convenience. The best-case scenario may be not to substitute one training with the other, but to use the computer-based home training as a complementary tool beside the auditory rehabilitation given by the therapist in the clinic. To avoid boredom in home training, especially for adults, it is convenient to perform the training task with the help of a partner.
Processing strategy
As specialists, we have to make sure that the processing strategy used is as convenient as possible to better access the spectro-temporal cues. Goehring et al. [18] used the NNSE processing strategy to enhance the speech perception of cochlear implant users in difficult, noisy environments by giving a more detailed frequency signal. It is better to provide this combination of improved processing strategy and aural rehabilitation to ameliorate the patient’s hearing experience with the cochlear implant and access full benefit.
Time of onset of auditory training
When counseling with the patient prior to the implant, it is mandatory to highlight the importance of starting auditory training immediately after programming the processor with the first MAP because the cochlear implant alone is not sufficient especially in complicated listening situations. The patient should understand that hearing with a cochlear implant is not the same as for hearing aids or normal hearing; learning to hear with a cochlear implant is provided via auditory training so as to achieve better speech perception and differentiation.
Choosing the auditory training method
Many training tasks were used in previous research, including speech tracking, sentence identification, phoneme identification, environmental sound training, listening cube, etc. Each task produced an enhancement for a given number of participants. In addition, as known, each patient with hearing loss, whether he/ she has hearing aids or cochlear implants, benefits differently and has different hearing preferences, along with the dissimilarities in personality, intellect, environment, etc. [4]. Accordingly, it is probable that all of these characteristics are influencing the perception of sound for each individual. For this purpose, it is recommended that the specialist develop a proper training procedure for each patient, while considering his/her cognitive (attention, memory…), linguistic, social, and intellectual skills and communication needs. In general, the available studies reveal that there are no simple auditory training procedures that can be used for everyone, which highlights the necessity to compare all these approaches then choosing the appropriate one for each patient. De Raeve et al. [17] explained that the listening cube approach is currently used in many countries to plan auditory training sessions using the patient’s initial capabilities as a starting point. Moving forward, we will need to test this planning strategy in order to study its efficiency. Shafiro et al. [16] trained their participants using environmental sound training, and the subjects benefit from it. Conversely, in other research, the focus was on training the patient on phoneme identification [15], or on speech tracking method [7]. In both training procedures, there was an improvement in speech perception. For this reason, it may be beneficial to use environmental sound training along with speech identification training or speech tracking towards the development of the patient’s ability to identify both sounds, learn the differences between them, and learn to focus on speech in noisy environments. The speech tracking method contributes to a significant improvement when used by Bernstein et al. [6] and Plant et al. [7]. The subjects showed an increase in both tracking rate and speech recognition. It may be a beneficial method for training adults with cochlear implants.
Generalization of the results
In all the training methods illustrated in previous studies, it was difficult to obtain a reliable interpretation of the possibility of generalization of the results to real-life situations. To optimize the benefits of training to everyday situations, it may be better to conduct the experiment in more realistic environments, resembling everyday listening situations encountered by the patient in order to maximize the gain from the training. Besides that, using different stimuli in testing and training helps to detect the specific effectiveness of the training [3] while making sure that the patient is not showing advancement only from the repetition.
Tracking the improvement
Additionally, it is important to test the patient’s improvements over the course of the training to avoid proceeding with the program when the patient is not benefitting. In this case, the training tasks or the difficulty level will be adjusted, or the duration increased, according to each situation.
Duration of auditory training
Concerning the duration of the training, the majority of the previous findings conducted trainings for a short period of time; five days of training for participants in the study of Fu, et al. [11], six weeks of training in the research performed by Miller, et al. [22] and four weeks of training with Ingvalson et al. [19]. However, Plant et al. [7] studied the effect of speech tracking clinician-based training over a period of three years. The patient’s monitored indicators significantly improved over this period in both tracking rate and speech recognition. Therefore, it may be convenient to provide the patient with a long-term auditory rehabilitation regimen; however, the duration should depend on the degree of improvement, hence the importance of tracking the patient’s advancement in parallel with the training.
Participants selection
Last but not least, training normal-hearing listeners with a shifted speech may not be a suitable way because the training could have positive outcomes for those participants, while it could not be generalized to cochlear implant patients especially for patients with an extended period of deafness.
Previous studies limitations
Some of the most witnessed limitations in previous studies were the small sample size adopted, as well as the heterogeneity between the participants. For this reason, a task for future work will be to conduct a cohort study with an increased sample size like in the case of Fu, et al. [3] with the least heterogeneity possible between the participants, to assess the actual benefit of auditory training in a limited subset of population. In addition, as was mentioned before, the training should be conducted in more realistic real-life situations for better generalization of results. A period without intervention should also be integrated, and then the patient is tested to see the possibility of retention of the improvements. Finally, limited research investigated the different training protocols, which is an important task for future works [4].
Conclusion
In summary, the findings from this systematic review provide promising outcomes for the future of auditory training for cochlear implant users. Although less benefit was obtained from some training strategies compared to others, it is believed that auditory training, when chosen specifically according to each patient’s needs, can enhance speech understanding for adult cochlear implant users. From the analysis of the previous studies, the characteristics underlying the success of auditory training may be an extended training period adequate for each implanted, training in more realistic situations while tracking the improvement, and the training duration with a combination of clinician-directed training and computer-based home training if possible. Thus, with practice and consistency, auditory training might be a crucial step to take full advantage of the implant in preparation for a hearing experience with the least limitation possible.
References
- Waltzman SB, Roland JT (2006) Cochlear implants. Thieme.
- Stach B (2008) Clinical audiology: An introduction. Nelson Education.
- Fu QJ, Galvin III JJ (2007) Perceptual learning and auditory training in cochlear implant recipients. Trends in Amplification 11(3): 193-205.
- Bieber RE, Gordon-Salant S (2020) Improving older adults' understanding of challenging speech: Auditory training, rapid adaptation, and perceptual learning. Hear Res pp. 108054.
- Bess FH, Humes L (2003) Audiology: the fundamentals: Lippincott Williams & Wilkins, USA.
- Bernstein C, Bakke M, Mazevski A, Blake-Rahter P, Presley R, et al. (2012) Benefits of speech tracking training on sentence recognition, tracking rate, and self-assessed communication function in adult cochlear implant users. J Acad Rehab Audiol 45: 11-39.
- Plant G, Bernstein CM, Levitt H (2015) Optimizing Performance in Adult Cochlear Implant Users through Clinician Directed Auditory Training. Semin Hear 36(4): 296-310.
- Fu QJ, Galvin J, Wang X, Nogaki G (2005) Moderate auditory training can improve speech performance of adult cochlear implant patients. Acoustics Research Letters Online 6(3): 106-111.
- Loebach JL, Pisoni DB, Svirsky MA (2009) Transfer of auditory perceptual learning with spectrally reduced speech to speech and nonspeech tasks: implications for cochlear implants. Ear Hear 30(6): 662-674.
- Stacey PC, Raine CH, ODonoghue GM, Tapper L, Twomey T, et al. (2010) Effectiveness of computer-based auditory training for adult users of cochlear implants. International Journal of Audiology 49(5): 347-356.
- Fu QJ, Nogaki G, Galvin JJ (2005) Auditory training with spectrally shifted speech: implications for cochlear implant patient auditory rehabilitation. J Assoc Res Otolaryngol 6(2): 180-189.
- Green T, Faulkner A, Rosen S (2019) Computer-Based Connected-Text Training of Speech-in-Noise Perception for Cochlear Implant Users. Trends Hear 23: 2331216519843878.
- Oba SI, Galvin JJ, Fu QJ (2013) Minimal effects of visual memory training on auditory performance of adult cochlear implant users. J Rehabil Res Dev 50(1): 99-110.
- Schumann A, Hast A, Hoppe U (2014) Speech performance and training effects in the cochlear implant elderly. Audiology and Neurotology 19(Suppl 1): 45-48.
- Schumann A, Serman M, Gefeller O, Hoppe U (2015) Computer-based auditory phoneme discrimination training improves speech recognition in noise in experienced adult cochlear implant listeners. International Journal of Audiology 54(3): 190-198.
- Shafiro V, Sheft S, Kuvadia S, Gygi B (2015) Environmental sound training in cochlear implant users. Journal of Speech, Language, and Hearing Research 58(2): 509-519.
- De Raeve L, Anderson I, Bammens M, Jans J, Haesevoets M, et al. (2012) The listening cube: a three-dimensional auditory training program. Clin Exp Otorhinolaryngol 5 Suppl 1(Suppl 1): 1-5.
- Goehring T, Bolner F, Monaghan JJ, Van Dijk B, Zarowski A, et al. (2017) Speech enhancement based on neural networks improves speech intelligibility in noise for cochlear implant users. Hearing research 344: 183-194.
- Ingvalson EM, Lee B, Fiebig P, Wong PC (2013) The effects of short-term computerized speech-in-noise training on postlingually deafened adult cochlear implant recipients. J Speech Lang Hear Res 56(1): 81-88.
- Zhang M, Miller A, Campbell MM (2014) Overview of nine computerized, home-based auditory-training programs for adult cochlear implant recipients. Journal of the American Academy of Audiology 25(4): 405-413.
- Völter C, Schirmer C, Stöckmann C, Dazert S (2020) Computerbasiertes Hörtraining in der Hörrehabilitation Erwachsener nach Cochleaimplantation. HNO p. 1-11.
- Miller JD, Watson CS, Kistler DJ, Wightman FL, Preminger JE (2008) Preliminary evaluation of the speech perception assessment and training system (SPATS) with hearing-aid and cochlear-implant users. Proc Meet Acoust 2(1): 1-9.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...