Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Research Article(ISSN: 2641-1709) 
Assessment of Changes in Eustachian Tube Functions before and after Septoplasty Volume 9 - Issue 3
Savaş Kırat1 and Berkay Arslan2*
- 1Departmnet of Audiology, Private Practice, Turkey
- 2Department of Audiology, Atilim University, Turkey
Received: November 08, 2022; Published: November 29, 2022
Corresponding author: Berkay Arslan, Department of Audiology, Atilim University, Turkey
DOI: 10.32474/SJO.2022.09.000315
Keywords: Cochlear implant; sensorineural hearing loss; stapedial reflex; sound stimuli; loudness; recruitment
Abbreviations: Eustachian Tube; NOSE: Nasal Obstruction Symptom Assessment; PTA: Pure Tone Audiometry; TTP: Tympanometric Peak Pressure
Introduction
The Eustachian Tube (ET) is 31-38 mm long and is localized at an angle of 450 to the horizontal plane, 1/3 of which is posterior bone and 2/3 is anterior cartilage. It is an ‘S’ shaped structure consisting of bone and cartilage between the middle ear cavity and the nasopharynx [1,2]. ET is closed at rest and opened in movements such as swallowing, yawning, and sneezing [3]. The primary function of ET is ventilation of the middle ear, [4]. Another function is protection. ET prevents materials from the nasopharynx from passing into the middle ear. The closest that the cartilage part of ET is closed plays an active role in the realization of protection. The length of the tube and pressure variations in the tube are important in maintaining it. In children, the length of the ET is shorter and straight. This makes ET more susceptible to infections. When it is opened by the contraction of the muscles, the fatty tissue limits the opening of the tube, providing continuation of aeration and protecting ET, [5]. Septoplasty with deviation of the septum; It is performed to preserve the functional and aesthetic structure of the septum. The septum also separates the nasal passages and acts as an absorbent in traumas to the anterior skull base. Septoplasty is the nasoseptal reconstruction surgery performed to correct the deviated septum. The main purpose of septoplasty is to make the quadrangular cartilage upright and straight. Septal deformities can be corrected with endonasal or external techniques [6-8]. One of the most important tasks of the nasal cavities is too warm and humidify the air in the nose. The Eustachian tube connecting the middle ear and the nasopharynx can respond to nasal cavity changes [5]. The goal of the current study was to compare the ET functions of patients before and after septoplasty.
Methods
Participants: The data for the study obtained from Kırat 2015 MSc thesis with the same name. The study was designed retrospectively. Patients who applied to a private university hospital with complaints of nasal obstruction in 2015 were included in the study.
Inclusion and exclusion criteria for the study as following:
Inclusion Criteria
a) Normal hearing (better than 20 dB SPL)
b) Unilateral nasal septum deviation c) Type a tympanogram
d) Nasal congestion complaint
e) Presence of upper airway infection during study
f) Tympanic membrane damage
Exclusion Criteria
a. Chronic rhinosinusitis
b. Nasal polyposis
c. Other intranasal pathologies
d. Hearing loss
e. Ear surgery history
f. Frequent otitis history
Procedure
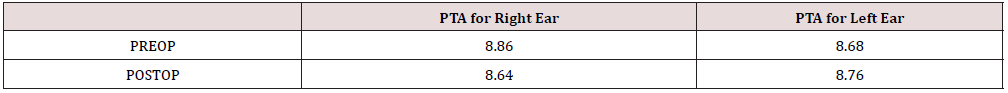
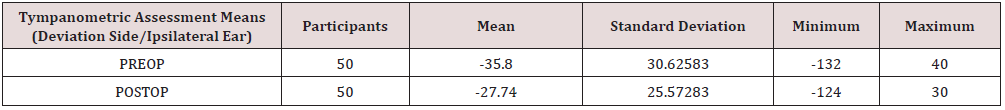
Between November 2014 and June 2015, 50 patients (22 women, 28 men) aged between 18-50 years (mean 32.9) who were diagnosed with isolated nasal septum deviation and had septoplasty operation were included in the study. Bilateral concha radiofrequency or electrocauterization was also applied to patients with turbinate hypertrophy. The surgeries were performed by two surgeons using the same surgical technique to ensure standardization, and an air-channel silicone nasal splint was used postoperatively, and the splints were removed at 48 hours. The nasal obstruction symptom assessment (NOSE) scale was used to evaluate surgical success. Eustachian tube functions were evaluated with Interacoustics AZ 26 (Interacoustics A/S, Assens, Denmark) tympanogram. The first evaluation was made on the morning of the operation and only patients with a type A tympanogram were included in the study. Then, the patients were re-measured by performing the Valsalva and Toynbee maneuvers to measure the Eustachian functions. Second measurements were made after 8 weeks postoperatively (Table 1). After Valsalva and Toynbee maneuver, Eustachian tube functionality was evaluated as good if the baseline and post-procedure tympanometric peak pressure (TTB) changed over 10 daPa, and bad if there was less change. Ears are classified as deviation side and opposite side of deviation and comparisons are made accordingly (Table 2).
Statistical Method: SPSS (IBM SPSS Statistics 24.0) program with the use of student’s t test was used to evaluate the pre and post results.
Results
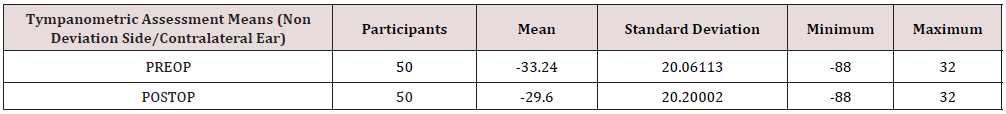
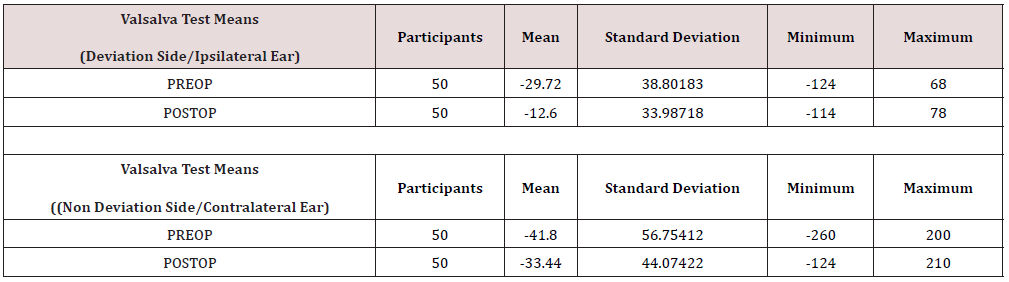
The mean NOSE scores were 12.48±4.78 preoperatively and 7.56±3.4 postoperatively. It was observed that the change in NOSE scores before and after 8 weeks was statistically significant (p=0.00). Detailed data can be seen in Graph 1. The mean pure tone audiometry results of participants for both right and left ear were assessed before and after surgery. The mean PTA for right ear 8.86 dB NHL for right ear before the surgery and 6.64 dB NHL after the surgery. The mean PTA for left ear 8.68 dB NHL before the surgery and 8.76 dB NHL after the surgery. There was no significant difference for PTA results, (p> 0, 005 for right and left ear). Tympanometric assessment means were assessed based on the deviation side and named as the contralateral ear and ipsilateral ear (Table 3). While the tympanometry means of the deviation side ear (ipsilateral) was -35.8 before the surgery, it was assessing and -27.74 after the surgery. A significant decrease was observed in patients after septoplasty, (p=0, 00). The tympanometry assessment means of the non-deviation side ear (contralateral) was -33.24 before the surgery, it was assessing and -29.6 after the surgery. A significant decrease was observed in patients after septoplasty, (p=0, 00). Measurements of Valsalva and Toynbee tests were also evaluated before and after septoplasty and assessed as deviation side and non-deviation side again. While the ipsilateral mean of Valsalva decreases significantly after septoplasty (p=0, 00), the difference in the contralateral side was not significant, (p=0, 12). The detailed data for Valsalva test can be seen in Table 4. When the Toynbee means were interpreted, there was no significant difference for either contralateral (p=0, 18) and ipsilateral ears (p=0, 19).
Table 4: Results of Valsalva Test before and after the Septoplasty for Ipsilateral and Contralateral ear.
Discussion
There are many studies examining the relationship between septoplasty and Eustachian tube in the field of audiology. Many studies have studied the Eustachian tube functions before and after the septoplasty operation. While some of the studies stated that septoplasty did not affect the Eustachian tube function, the opposite results were obtained in some studies. In the study, 70 patients were studied using the tympanometer for middle ear functions and Toynbee maneuvers for Eustachian tube functions before the operation and in the 3rd and 6th months of the operation both on the side of the deviation and on its contralateral side [9]. According to the results of the study, there is no statistical difference between the middle ear pressures on both the ipsi and contralateral sides. There was no difference in the ipsilateral and contralateral measurements of Eustachian tube functions. Eyigor et al. In a study conducted in 2013, they investigated the effect of surgical success on middle ear ventilation in 25 patients hospitalized for septoplasty operation. Although there was a significant decrease in NOSE scores before surgery and at the 3rd month, they did not detect a significant difference in tympanometry values.
At the same time, they did not find a statistically significant relationship between postoperative NOSE scores and middle ear pressure [10]. The study conducted by Şahin et al. in 2014 was conducted on twenty-three patients and 30 healthy volunteers. In the study, middle ear pressure and eustachian tube function of patients who underwent septoplasty operation were compared preoperatively and, in the 1st, and 3rd months of the operation. They measured nasal patency by rhinomanometry and found a significant decrease in total nasal resistance, but they did not detect any change in TTB or Eustachian tube functionality. According to their findings, they could not find a relationship between septoplasty and middle ear pressure and Eustachian tube function [11]. In addition, there are opinions reporting that septoplasty affects middle ear pressure and Eustachian tube function. Sereflican et al. 60 patients underwent septoplasty and acoustic impedance measurements of the patients were measured before the operation and on the 2nd and 5th days after the operation. According to the findings, while the internal nasal splints and tampons given to the patients for protection after the operation were not removed yet, the Eustachian tube function and middle ear pressure were different in the measurements made on the 2nd day.
According to the evaluations taken on the 5th day after the operation, there is no significant difference between the preoperative and postoperative 5th day impedance values [12]. The findings obtained in these studies show that nasal packings and internal nasal splints applied after the operation affect middle ear pressure and Eustachian tube function. Postoperative nasal packing was used in studies where septoplasty did not show any effect. In studies where septoplasty affected middle ear pressure and Eustachian tube function, internal nasal splints were applied to patients [12]. There are opinions in the literature that support this difference between the two applications. Yildirim et al. septoplasty was performed on 46 patients with normal middle ear functions [13]. While intranasal packing was applied to 26 patients, internal nasal splint was applied to 20 patients. While there was no difference between the groups in preoperative measurements, Eustachian tube dysfunction occurred in patients who used intranasal tampons on the 2nd and 5th postoperative days. No Eustachian tube dysfunction was observed in patients using internal nasal splints. Shaw proved that 50-68% of the cilia surface in the mucosa was lost due to intranasal buffering in his study in sheep in 2000 [14]. It has been supported by various studies that the use of intranasal packings after septoplasty operation causes Eustachian tube dysfunction [15,16].
Johannessen [17]. reported that there was no statistically significant difference in eustachian function on the first day in endonasal surgery cases with and without intranasal packing, and this difference developed due to mucosal edema, which was thought to develop later in cases where intranasal packing was used after the operation. Koch et al. [18] reported that negative pressure occurs in the middle ear of more than –300 dapa in 2/3 of the cases who underwent rhinoplasty, and the negative pressure equalizes after removing the tampon in most of the cases. reported to continue. Laszig [19], on the other hand, reported that 70% of septorhinoplasty cases had negative pressure in tympanometry measurements measured on the second day after surgery. In a study conducted by Low and Willatt [20], preoperative and postoperative middle ear pressures of 50 patients (6-10 months) were examined. Ipsilateral measurements were taken in the study. While the middle ear pressure measurements were -25.7±28.4 mm of water before the operation in the ear where the ipsilateral measurement was taken, it increased to -2.9±30.4 mm after the operation.
In Salvinelli et al. [21]. Eustachian tube function measurements of 40 patients before and after septum operation were measured with Tonybee and Valsalva maneuvers and tympanometric examination was performed. According to the pre- and post-operative results, tube functions increased from 46% to 90%. However, it took 1 month for middle ear pressure measurements to return to normal. In the study of Deron et al. investigating the relationship between septal surgery and tubal functions, they used the tubal compliance manometric test during the Valsalva maneuver. They found that there was an improvement in tubal opening pressure after septoplasty in both the deviation side and the contralateral side, in the early and late postoperative period [22]. According to the results of our study, nasal septum deviation adversely affects middle ear pressures and functions. It was concluded that the preoperative basal tympanometric peak pressures improved significantly after the operation, the eustachian functionality was significantly improved in both ears, but the improvement on the deviation side was much more pronounced. As a result, isolated nasal septal deviation negatively affects middle ear functions and special attention should be paid to nasal deviation in those who have frequent otological problems and candidates for otological surgery, and this problem should be solved first.
References
- Akyildiz AN (1998) Ear Diseases and Microsurgery. Skin 1, Ankara, Scientific Medicine Publishing House pp. 275-325.
- Bluestone CD (2004) Studies in otitis media: Children’s Hospital of Pittsburgh-University, Pittsburgh progress report-2004. Laryngoscope 114 (S105): 1-26.
- Bylander-Groth A, Stenstrom C (1998) Eustachian tube function and otitis media in children. Ear Nose Throat J 77(9): 762-764, 766,768.
- Kirat S (2015) Assessment of Changes in Eustachian Tube Functions Before and After Septoplasty, Unpublished Master of Thesis Turgut Özal university, Ankara, Turkey.
- Takasaki K,Sando I,Balaban CD, Miura M(2002) Functional anatomy of the tensor veli palatini muscle and Ostmann’s fatty tissue. Ann Otol Rhinol Laryngol 111(11): 1045-1049.
- Kridel RW, Kelly PE, Holzapfel MA (2010) The nasal septum. In: Cummingsn CW (ed). Otolaryngology Head and Neck Surgery (5th) ed. Mosby, NY, USA pp. 481-495.
- Marks SC (2000) Nasoseptal surgery. In: Nasal and Sinus surgery. WB Saunders, Philadelphia pp. 193-209.
- Park SS (2001) Treatment of the internal nasal valve 34(4): 805-821.
- Davari R, Behnoud F (2014) Study the Effect of Nasal Obstruction Surgery (Septoplasty) on Eustachian Tube Function and Middle Ear Pressure. J Ardabil Univ Med Sci 14(4): 322-330.
- Eyigör H, Osman Ü, Yilmaz MD, Aygezer N, Buyruk A (2013) Nazal septum deviasyonlu hastalarda ameliyat basarisinin orta kulak ventilasyonu üzerine etkisi. KBB Ihtisas Dergisi 23(1): 26-31
- Sahin MI, Güleç S, Perisan Ü, Külahli I (2014) Does septoplasty affect middle ear pressure and Eustachian tube functions? Erciyes Med J 36: 115-118.
- Sereflican M, Yurttas V, Oral M, Yilmaz B and Dagli M (2015) Is Middle Ear Pressure Effected by Nasal Packings after Septoplasty? J Int Adv Otol 11 (1): 63-65.
- Yildirim A, Yasar M, Bebek AI and Canbay E, Kunt T (2005) Nasal Septal Suture Technique versus Nasal Packing after Septoplasty. American Journal of Rhinology 19(6): 599-602.
- Shaw CL, Dymock RB, Cowin A, Wormald PJ (2000) Effect of packing on nasal mucosa of sheep. J Laryngol Otol 114(7): 506-509.
- Thompson AC, Crowther JA (1991) Effect of nasal packing on Eustachian tube function. The Journal of Laryngology & Otology 105(7): 539-540.
- McCurdy JA Jr (1977) Effects of nasal packing on eustachian tube function. Arch Otolaryngol 103(9): 521-523.
- Johannessen J, Poulsen P (1984) The influence of the anterior nasal packing on middle ear pressure. Acta Otolaryngol 97(3-4): 363-364.
- Koch U, et al. (1977) [Eustachian Tube Function and Middle Ear Pressure with Adhesive Tympanic Membrane (author's Transl)]. Laryngol Rhinol Otol 56(2): 156-159.
- Laszig R (1985) Development of pressure in the middle ear after nasal operations. HNO 33(44): 187-189.
- Low WK, Willatt DJ (1993) The relationship between middle ear pressure and deviated nasal septum. Clin Otolaryngol Allied Sci 18(4): 308-310.
- Salvinelli F, Casale M, Greco F, D'Ascanio L, Petitti T and Di Peco V (2005) Nasal surgery and eustachian tube function: effects on middle ear ventilation. Clin Otolaryngol 30(5): 409-413.
- Deron P, Clement PA and Derde MP (1995) Septal surgery and tubal function: early and late results. Rhinology 33(1): 7-9.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...