Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Research Article(ISSN: 2641-1709) 
Cervicofacial Cellulitis at the Omar Bongo Ondimba Army Training Hospital Volume 9 - Issue 3
Lekassa P1* , Atanga LC1 , Miloundja J1 , Manfoumbi Ngoma AB2, Koumba JS2 and Nzouba L1
- 1Departmnet of ENT and CCF, Omar Bongo Ondimba Army Training Hospital, Libreville, Gabon
- 2Stomatology Service Omar Bongo Ondimba Army Training Hospital, Libreville, Gabon
Received:August 23, 2023; Published:September 05, 2023
Corresponding author:Lekassa Pierrette, Departmnet of ENT and CCF, Omar Bongo Ondimba Army Training Hospital, Libreville,Gabon
DOI: 10.32474/SJO.2023.10.000335
Cervicofacial cellulitis are infections of the cellulo-adipose tissues of the face and neck, with extensive potential towards the mediastinum, which can be serious and life-threatening.
Objective: To describe the epidemiological, etiological, diagnostic, therapeutic and evolutionary aspects.
Patients and Methods: This was a retrospective study conducted in the ENT and CCF department of HIAOBO, on the files of
patients hospitalized for cervico-facial cellulitis between January 2016 and December 2019.
Results: There were 64 patients including 30 men (47%) and 34 women (53%), with a sex ratio of 0.88. The average age was
30 years and the extremes of 3 and 74 years. The portal of entry was dental in 75% of cases, tonsillar in 11% and skin in 8% of
cases. The notion of taking anti-inflammatories and immunosuppression was found respectively in 77% and 12.5% of cases. These
cellulitis were circumscribed in 46 cases (72%) and diffuse in 18 cases (28%) including 3 with mediastinal involvement. They
were serous in 13 cases (20%) and collected in 51 cases (80%). Bacteriological analysis of pus was positive in 50% of cases. The
treatment was medico-surgical. The evolution was favorable in 59 cases and death was reported in 2 cases following septic shock.
Conclusion: Cervicofacial cellulitis remains a low incidence condition in our context. Their treatment is medico-surgical.
Mortality can be reduced with early diagnosis and immediate treatment.
Keywords:Cervicofacial cellulitis; predisposing factors; medico-surgical treatment
Introduction
Cervicofacial cellulitis are poly-microbial inflammatory conditions, developed in the cellulo-adipose tissue of the face and neck [1,2]. They constitute a diagnostic and therapeutic emergency in ENT due to the rapidity of their development and the complications they can cause [2,3]. Their prognosis has now improved thanks to modern means of treatment, provided however that these are im plemented quickly, which is not always the case in developing countries [4]. The objective was to describe the diagnostic, therapeutic and evolutionary aspects of cervico-facial cellulitis in our context.
Patients and Methods
This was a retrospective descriptive study on the files of patients hospitalized for the management of cervico-facial cellulitis in the otolaryngology and cervicofacial surgery department of the Omar Bongo Ondimba Armed Forces Training Hospital (HIAOBO) in Libreville, between January 2016 and December 2019. The inclusion criteria were all records of patients hospitalized for cervico- facial cellulitis and the non-inclusion criteria were all unusable records, patients seen on an outpatient basis. The collection of data was done from hospital registers and their collection on a standardized survey sheet. The data studied were age, sex, contributing factors, etiology, consultation time, symptoms and signs, clinical data (physical examination , location, clinical stage: serous or collected, diffuse or circumscribed; imaging), bacteriological, therapeutic (medical or surgical) and evolutive. Data analysis was done using SPSS21.0 software. The quantitative variables were expressed by their measure of central tendency, namely the mean, and the qualitative data were represented as a percentage.
Results
A total of 64 patients were selected including 30 men (47%) and 34 women (53%) with a sex-ratio of 0.88. The average age was 30 years with the extremes of 3 and 73 years. The distribution of patients by age group showed that 10 cases (16%) were children under 15 years old, 27 cases (42%) were aged 23 to 32 years.
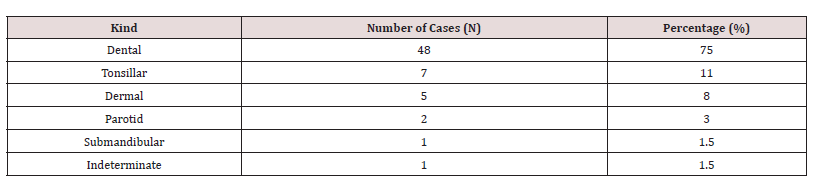
In History the notion of taking non-steroidal or steroidal anti- inflammatory drugs was found in 49 cases (77%) and unsuitable antibiotic therapy in 17 cases (27%). A co-morbidity responsible for immunosuppression was present in 8 patients (12.5%). These were human immunodeficiency virus (HIV) infection in 4 cases (6%), homozygous SS sickle cell disease in 3 cases (5%) and type II diabetes in 1 case (1, 5%). The Gateway was dental in 48 patients (75%). The other entrance doors found are reported in (Table 1). Retromandibular cellulitis of dental origin represented 93% and perimaxillary cellulitis 6.5%. The affected teeth were 46, 47 and 48 on the left side with 55.6%, against 40% on the right for teeth 36, 37 and 38. The involvement was bilateral in 4.4% of cases.
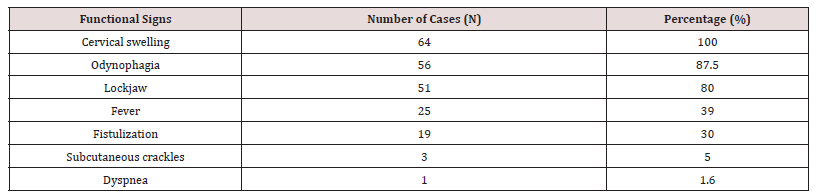
The average consultation time was 12 days with extremes of 2 to 60 days. The reason for consultation was swelling of the face and/or neck present in all patients. This was facial, cervical and cervico-facial in 20%, 28% and 52% of patients respectively (Figure 1). The symptoms and signs of these cellulitis are summarized in (Table 2). Cellulitis was circumscribed in 46 patients (72%) and diffuse in 18 patients (28%) including 3 with mediastinal involvement. They were collected in 51 patients (80%) and serous in 13 patients (20%). Bacteriologically, only 20 samples were analyzed and showed 10 sterile cases and 10 cases isolated a germ including streptococcus spp in 4 cases, Klebsiella pneumonia in 3 cases, Staphylococcus spp 2 cases and Enterobactercloacae in 1 case.
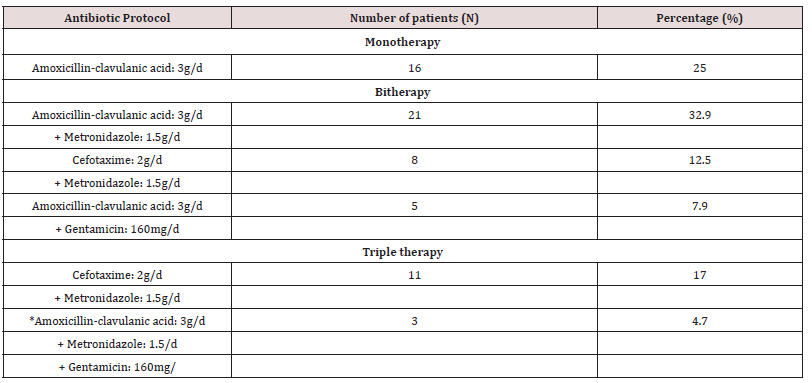
Treatment was probabilistic parenteral antibiotic therapy in all patients which was adjusted based on susceptibility testing. Surgical drainage was performed in patients with the collected form, i.e. 51 cases (80%). It consisted of a scalpel incision with evacuation and drainage of the pus. This surgery was performed under local anesthesia in 15 cases (29%) and under general anesthesia in 36 cases (71%), with debridement, excision of necrotic tissue and abundant washing with betadine, hydrogen peroxide and to the dakin with placement of Delbet- type drainage blades (Figure 2). After evacuation of the pus, surgical drainages and repeated lavages were performed. A minimal incision was performed in 38 patients (74.5%), an L or Paul-André incision in 3 patients (5.9%), the bimastoid incision was performed in 10 patients (19.6 %) and a thoracotomy in 1 patient. Treatment of the portal of entry was a dental avulsion by the stomatologist in 75%, a drainage of the phlegmon and a tonsillectomy. A tracheostomy in 6 cases (11.8%). The duration of the day in resuscitation was on average 7 days with an extreme of 1 to 25 days. Thirteen patients (20%) did not require surgical treatment. The evolution was favorable in 59 patients (92%) with complete healing, complications were noted in 3 cases such as delayed healing, osteitis of the mandible and bilateral pleurisy in one case each. We deplore the death that occurred in 2 cases (3%) following septic shock. The duration of hospitalization varied from 3 to 40 days with an average of 11.5 + or -7.8 days.
Discussion
The incidence of cervico-facial cellulitis is very variable in the literature. Indeed, this study found an average of 16 cases/year. This figure is higher than that of Bouraima Parakou in northern Benin [5] which reports 14 cases/year. This result is close to that of Benzarti et al who had collected 150 odontogenic cellulitis in 10 years, achieving an incidence of 15 cases/year [6] and El Ayoubi et al 60 cases in 4 years, i.e. an incidence of 15 cases/year [7]. High frequencies have been reported with Rouadi 47 cases/year [8], it was 26 cases/year in the series of Njifou Njimah et al. [9] in 2014, 25 cases/year in that of Tran Ba Huy [1] in 2011. It reached 132 cases/ year in Kaba’s study [10] in Gabon in 1998 conducted in a dental department. Lower frequencies had been noted in the studies by Kpemissi in Togo in 1995 [11] with 8 cases/year and by Badou [12] in Côte d’Ivoire had noted a hospital prevalence of cellulite of 3.5% with a annual incidence of 4.3 cases. These figures show that the prevalence of the disease is increasing in the sub-Saharan region. The increase could also be linked to better care-seeking by the community in recent years.
According to the literature [5,9,13,14], this pathology is the prerogative of young adults between 20 and 40 years old, which corresponds to the results of our study with an average age of 30 years. In our study the female predominance was reported, it was also found by Miloundja [2]. However, other authors have reported a male predominance [1,9,14]. This fact would be explained by a greater frequency of accidents of the wisdom tooth at this age [15] and also by the often neglected oral condition, thus constituting the main entry point for cervico-facial cellulitis. Taking NSAIDs was the main risk factor with 49 cases (77%) in our study. This observation was made by Miloundja et al. [2] who reported it with 87.5% and El Yaoubi et al with 48.5% [7] and Vodouhé et al. with [14]. NSAIDs calm pain and fever by inhibiting cyclo-oxygenase and preserve the release of prostaglandins which are the mediators of inflammation and thus reduce the immune defenses of patients [ 16] . This can be explained in our context by the fact that NSAIDs are indeed very accessible and cheap. Thus their consumption is an important factor in the extension of CCFs. These cellulitis readily develop on immuno compromised grounds. The other risk factors such as tobacco, alcohol, diabetes, HIV infection are usually described in several studies [9,13,14]. In our study HIV was found in 6% of cases and diabetes in 1.5% of cases. Njifou Njimah et al report 20% diabetics and 39.3% HIV [9]. Keita et al. [3] had found 4.76% and 9.52% respectively and Tran Ba Huy 1 12% and 2%. These conditions which alter the defense system and promote the occurrence of various infections, probably including cervico-facial cellulitis.
Clinically, the main entry point for cellulite is dental in our study with 75%. It is also found in other series [1,7,9,13]. Lower molars more prone to cavities being the main offending teeth [2,6,9,13]. This therefore explains the predominance, as in our study, of lower and submental gene locations before their extension towards the poneurotic spaces of the neck due to gravity. However, other entry points are possible, in particular pharyngeal infections or cervicofacial trauma. The clinical picture is dominated by inflammatory cervical and/or facial swelling, the most described sign in the literature [17]. Other signs related to inflammation (trismus, fever) and cervical extension (dysphagia, dyspnea) can also be found depending on the location of the cellulitis [1,9,13]. However, the presentation of cellulitis depends on both their location and the stage of infection. Concerning the localization, two types of cellulitis are distinguished: perimaxillary cellulitis, much less frequent, represents 6.5% of the cases in our series, 31.3% in that of Benzarti et al. [6].
Cellulite naturally progresses from the pseudo-phlegmonous (serous) stage to the phlegmonous (collected) stage, these stages being circumscribed or diffuse. There is also a so-called gangrenous form, immediately extensive, which is generally caused by anaerobic germs [18]. As in our study, the collected forms that are the most described in the literature [8,13,15]. This could be explained by the delay in treatment in our context. The bacteriological examination carried out in 20 cases of our series allowed the identification of the germ in 10 including streptococcus spp (4 cases), Klebsiella pneumonia (3 cases), Staphylococcus spp (2 cases) and Enterobactercloacae (1 case). Njifou Njimah et al. [9] report the identification of germs in 11 cases including Streptococcus (5 cases), Staphylococcus (3 cases) and Escherichia coli (3 cases). This reduced number of results after bacteriological analyzes could be linked to the transport time between the place of sampling and the analysis laboratory. The treatment of cervico-facial cellulitis is medico-surgical associated with the treatment of the front door. The antibiotics used by the majority of authors are beta-lactams and imidazoles which are associated in several therapeutic protocols [7,10,13,14]. With antibiogram results other classes of antibiotics such as quinolones are associated. This was the case in our study and also found in the Njifou Njimah and Vodouhe series [9,14]. The surgical treatment consists of a scalpel incision with evacuation and drainage of the pus. In our study, this treatment was performed in 80% of cases including 29% under local anesthesia and 71% under general anesthesia. Atanga et al. [13] performed the drainage incision in 82% of cases, including 98 cases (96%) under local anesthesia and 4% under general anesthesia in the operating room.
The duration of treatment varies according to the authors. It was 3 to 40 days in our study, compared to 10 to 27 days for Njifou Njimah et al. [9], 9 to 26 days for Tran Ba Hui [1] and 1 to 26 days for Atanga [13]. The treatment of cervico-facial cellulitis is medico-surgical associated with the treatment of the front door. In serous forms, treatment with drugs and the portal of entry may be sufficient [19]. The antibiotics used by the majority of authors are beta-lactams and imidazoles which are associated in several therapeutic protocols [7,13,14,15]. Surgical treatment should not be limited to a simple drainage incision but should allow purulent discharge as long as it exists [20]. This is only made possible by a wide incision under general anesthesia in the operating room with flattening of all the collection pockets and abundant washing. This practice was the most common in our study. However, in the series by Njifou Njimah et al. [9], Diallo et al. [15] or Kpemissi et al. [11], the chairside drainage incision was widely practiced. The case fatality rate in this study was 3%. This rate is significantly lower than that of Vodouhé [14] with 14.5%, Atanga 10% [13], Tran Ba Hui 7.5% [1]. These deaths can be explained by the delay in consultation and rapid access to care.
Conclusion
Cervicofacial cellulitis is a medical-surgical emergency. They complicate a dental or oropharyngeal infection and spread by contiguity to the neck and the mediastinum. Knowledge of the predisposing factors would make it possible to take effective preventive measures in order to reduce the occurrence of the condition. . Mortality can be reduced on the condition of early diagnosis and immediate medico-surgical management.
References
- Tran Ba Huy P, Blancal JP, Verillaud B, Mabazaa A, Herman P (2011) Cervicofacial cellulitis a serious ENT emergency. Bull Acad Natle Med 195(3): 661-678.
- Miloundja J, Assini Eyogho SF, Mandji Lawson JM, Ondounda M, Koumba JS, et al. (2011) Diffuse cervico-facial cellulitis. 32 cases seen in Libreville. Health 21: 153.
- Keita M, Doumbia K, Diango D, Diallo M, Timbo SK, et al. (2008) Extensive cervical cellulitis in a sub-Sahelian hospital environment, a forgotten pathology? Case of Mali. Black African Medicine 55 (09): 464-467.
- Bissa H, Salou M, Pegbessou EP (2014) Epidemiological and bacteriological aspects of cervico-facial cellulitis at the CHU Sylvanus Olympio in Lomé. African Journal of ENT and Cervicofacial Surgery 14(1): 2-3.
- Bouraïma FA, Hounkpatin SHR, Vodouhe UB (2019) Diagnostic and therapeutic aspects of cervico-facial cellulitis in parakou, benin. J Rech Science Univ Lomé (Togo), Special 21(2): 299-307.
- Benzarti S, Mardassi A, Ben Mhamed R (2007) Cervicofacial cellulitis of dental origin: about 150 cases. J Tun Orl 19: 24-28.
- El Ayoubi A, El Ayoubi F, Mas E (2009) Diffuse cervico-facial cellulitis of dental origin: about 60 cases. Med Buccale Chir Buccale 15: 127-135.
- Rouadi S, Ouaissi L, El Khiati R (2013) Cervicofacial cellulitis about 130 cases. Pan Afr Med J 14: 88.
- Njifou Njimah A, Essama L, Kouotou EA (2014) Cervicofacial cellulitis in Cameroonian hospitals. Health Sci. Say 15(1): 1-4.
- Kaba M, Cadot S, Miquel JL (1998) Perimaxillary cellulitis at the provincial hospital of Mouila. Tropical Odonto-Stomatology 4:18-22
- Kpemissi E (1995) Cervicofacial cellulitis of oral origin: Study of 26 cases at the University Hospital of Lomé Rev Laryngol Oto-Rhinol 116: 195-197.
- Badou KE, Buraima F, Yoda M, Traore K (2014) Cervicofacial cellulitis at the Yopougon university hospital center (Abidjan-Côte-D'Ivoire). International Review of the College of African Odonto-Stomatology and Maxillofacial Surgery 21(3): 5-10.
- Atanga LC, Ngaba Mballa ON, Edouma Bohimbo J, Zingui Ndongo Ottou MM, et al. (1979) Diagnosis, Treatment and Prognosis of Cervicofacial Cellulitis in Yaoundé (Cameroon). Health Sci. Say 21(6): 60-64
- Bidossèssi Vodouhe U, Gouda N (2006) Diffuse Cervico-Facial Cellulitis: Epidemiological, Diagnostic and Therapeutic Aspects at the Teaching Hospital CNHU HKM of Cotonou. International Journal of Otolaryngology and Head & Neck Surgery 11: 266-276.
- Diallo OR, Balde NM, Conde B, Camara SAT, Bah AT (1982) Cervicofacial cellulitis in diabetic patients at the University Hospital of Conakry. Rev Col Odonto-Stomatol Afr Chir Maxillo-fac 13(3): 13-16.
- Peron, JM, Mangez JF (2002) Cellulites and fistulas of dental origin. Medical-Surgical Encyclopedia (Scientific and Medical Editions Elsevier SAS, Paris 22-033-A-10, 14.
- Potard G, Marianowski R, Fortun C (2000) Face and neck cellulitis: about 13 cases. J Fr ENT 49: 325-327.
- Benbouzid MA, Benhyammou A, EL Messaoudi A, Jazouli N, Kzadri M (2004) Cervicofacial cellulitis: about 8 cases. Medical hope 11(102): 86-90
- Rifki C, Rochd T (2009) Acute circumscribed cervico-facial cellulitis of dental origin. Medical Landmark 35: 1-9.
- Ragot JP (1998) Dental infectious foci and their complications. Rev. Prat 48: 1714-1717.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...