
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2638-6003
Case Report(ISSN: 2638-6003) 
Using Musculoskeletal Ultrasound to Identify a Tibial Metadiaphysis Stress Fracture: A Case Report Volume 6 - Issue 4
Jason Le DO1, Sanjay Mahadevan BA2*, Jeffrey Palmer BS3, Kyle J Dineen BS2, Roosevelt Desronvilles BS2
- 1Regenerative Orthopedics and Sports Medicine, Rockville Pike # 300, Rockville, MD, USA
- 2Orthobiologics Research Initiative Inc, 11200 Rockville Pike #230, North Bethesda, MD, USA
- 3Howard University College of Medicine, 520 W St NW, Washington DC, 20059
Received: January 31, 2025; Published: February 10, 2025
Corresponding author: Sanjay Mahadevan, Orthobiologics Research Initiative Inc, 11200 Rockville Pike #230, North Bethesda, MD, USA.
DOI: 10.32474/OSMOAJ.2025.06.000244
Abstract
Lower limb stress fractures (SF) can be challenging for physicians to diagnose due to broad clinical presentation and etiology. Bone scintigraphy (bone scan) has been historically accepted as the gold standard for diagnosing these injuries, but studies appear to show an elevated risk of radiation exposure, necessitating judicious use of this imaging modality. Plain radiography is the most cost-accessible choice for imaging osseus structures, but as this case demonstrates, they do not have a high degree of accuracy for diagnosis SF. Magnetic Resonance Imaging (MRI) is an accurate imaging modality for diagnosing SF, but can carry excessive cost. Musculoskeletal ultrasound (MSK US) imaging is an emerging diagnostic imaging technique that can be used in early detection of SF. This case presents a 67-year-old runner, whose distal tibial metadiaphysis stress fracture was initially identified with MSK US and later confirmed with MRI. This case presents a promising option for patients with SF who are at elevated radiation risk from bone scans and who would like to avoid excessive cost and a delay in medical intervention associated with MRI. Further research and possible randomized controlled trials (RCTs) are needed to further assess the specificity and sensitivity of using MSK US to identify SF.
Keywords: Ultrasound; Musculoskeletal ultrasound; Tibial stress fracture; Stress fracture; Metadiaphysis; Running
Introduction
Diagnosing lower limb stress fractures (SF) clinically can be challenging due to the broad range of potential differential diagnoses. These include conditions such as compartment syndrome, infections, soft tissue injuries, and overuse-related issues like medial tibial stress syndrome and periostitis. Historically, several imaging techniques have been used to diagnose SF, each with varying levels of sensitivity. Plain radiography (X-rays) has traditionally been the initial choice due to its accessibility and low cost, but it often lacks the sensitivity to detect early SF, typically missing fractures until about two to three weeks after symptoms arise, once periosteal reactions or bone remodeling are evident [1,2].
The gold standard for diagnosing SF is either triple-phase technetium-99m bone scan (scintigraphy) or magnetic resonance imaging (MRI). Bone scintigraphy has been important due to its high sensitivity for detecting bone remodeling within days of fracture onset. However, this imaging modality has low specificity as it may also show positive results for infections or tumors [2,3,4]. Additionally, bone scans are typically involving excess radiation exposure to the patient [5,6]. Currently, MRI is considered the most sensitive and specific tool, identifying both the fracture line and the associated marrow edema, which makes it highly effective for early diagnosis. MRI also avoids radiation exposure and offers better softtissue contrast than CT scans, which, while helpful for confirming fracture details, have limited sensitivity for early detection and involve higher radiation doses [2,7]. However, MRIs are costly and taxing on the healthcare system [8,9]. Other clinical tests have also demonstrated promising diagnostic potential.
Diagnostic musculoskeletal (MSK) ultrasound (US) has been identified as a relatively accessible and effective diagnostic tool in various settings and is increasingly recognized as a valuable tool for efficiently assessing SF. While its use is primarily restricted to superficial bones, US can effectively visualize the hyperechoic outer margins of cortical bone, identifying cortical buckling and the surrounding hypoechoic callus [3]. Numerous studies indicate that eliciting pain while US is applied directly over the fracture site may also serve as a reliable indicator of an underlying SF [2]. Moreover, US has been used a diagnostic modality in the detection of lower limb SF of the metatarsal [10,11,12,13,14,15], calcaneus [16,17], ankle malleolus [18], distal fibula [19,20], and proximal tibia [21], There have only a handful of documented cases of USdetected SF of the tibial mid-shaft [14,22,23], none of which describe identification of SF of the distal tibial metadiaphysis. The purpose of this case report is to contribute to the limited evidence in literature regarding the diagnosis of tibial stress fractures with MSK US, and the first document case of identification of SF of a distal tibial metadiaphysis using MSK US.
Case Presentation
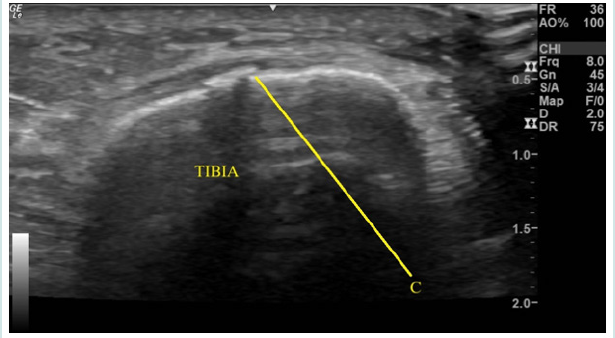
CM was a 67-year-old female runner presenting for an initial evaluation of left ankle and distal medial shin pain. Her pain was primarily present when running and she experienced a deep sharp pain in her shin, with a 5/10 score on the numerical pain scale (NPS). On physical exam, her tibia was tender to palpation with a small prominence over the distal medial aspect. She arrived to clinic with prior recent X-ray, ordered by her primary care physician. As seen in (Figure 1), her X-ray results were unremarkable for any pathology. Next, diagnostic MSK US was performed using the General Electric Logiq E R6 Portable Ultrasound machine, with a high-frequency linear transducer positioned over her area of tenderness on the distal tibial metadiaphysis. Her MSK US exam revealed a frank cortical break in the distal tibia, as seen in (Figure 2). Additionally, she experienced tenderness to sonopalpation. Due to a high clinical suspicion for a stress fracture, an MRI was ordered. She was recommended to strictly avoid weight-bearing activity for [5,7] days and was advised to avoid running for [4,6] weeks, with a gradual return to running through a walk-run program at physical therapy.
Figure 1: Normal radiographs (X-rays) of left lower leg in the anterior-posterior (AP) and lateral orientations with no osseus defects detected.

Figure 2: Musculoskeletal Ultrasound imaging moderate cortical irregularity (C) of the tibial metadiaphysis, visualized in shortaxis, with through sound transmission; suggestive of fracture at area of maximal intensity.
Her 1st MRI, of her ankle, revealed a suspected cortical defect of the tibia with present bone marrow edema. This indicated an incompletely viewed stress fracture of the tibial metadiaphysis, as seen in (Figure 3). For thoroughness another MRI was ordered and received by the patient 3 weeks after the 1st. Her 2nd MRI revealed a near-complete resolution of bone marrow edema, but with a clearly identifiable cortical defect, indicative of a healing stress fracture. This is seen in (Figure 4). The patient was advised to continue her gradual walk-run program through physical therapy after this MRI confirmation. At her 2-month follow-up, the patient reported complete resolution of symptoms.
Figure 3: Axial slice of Magnetic Resonance Imaging (MRI) of left ankle showing cortical irregularity (C) within anterior distal tibial metdiaphysis and mild underlying bone marrow edema (BME) suggestive of potential incompletely imaged stress fracture (SF). Tibia (T) and Fibula (F).
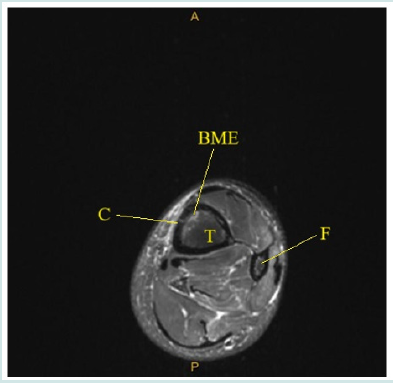
Figure 4: Three axial slices of Magnetic Resonance Imaging (MRI) of left tibia/fibula. Cortical defect identified (C), with improving bone marrow edema (BME), suggestive of healing stress fracture of the anterior and medial distal tibial metadiaphysis. Tibia (T) and Fibula (F).

Discussion
The purpose of discussing this case is to further document the use of MSK US to identify a tibial SF. As previously discussed, X-rays are not a reliable imaging modality for identifying lower limb SF. Bone scans have been documented to present radiation risk to patients and should only be used in cases where other imaging modalities lack accuracy. MSK US presents a potentially cost-saving modality for early detection of SF, especially in comparison to MRI. There are limitations to this case. Firstly, like all other case reports, the findings are not generalizable due to the lack of causality. Additionally, there exists a publishing bias given the prediction to publish positive results and a risk of overinterpretation of the results by the reader [24].
Secondly, the patient’s second MRI revealed a healing SF and was ordered because the first MRI incompletely viewed the original stress fracture. However, studies have shown that MSK US is a reliable tool to identify long bone fractures and cortical breaks [25,26], as was done in this case. Lastly, this patient did not complete patient-reported outcome measures (PROMs) to track functional or pain improvement from baseline in a standardized fashion. While they anecdotally report significant functional improvements, future cases, and studies should include such outcome measures to assess symptomatic improvement over time. However, there are several positive aspects to this case. Publishing observations of new treatments for common pathologies can lead to future research and the inherent educational value of reading clinical cases for physicians [24]. Moreover, the potential utility of MSK US as a standardized modality for early identification of SF especially in radiation-sensitive patients. Because of this, we feel that it is important to add this case report to the published medical literature to increase knowledge and awareness of this diagnostic imaging option.
We believe future cases and higher-level works should incorporate a more scientifically rigorous reproduction, as many significant questions still exist. This highlights the necessity for a thorough investigation of MSK US in early identification of SF, potentially offering a lower risk profile than bone scans and lower cost profile that MRI.
Individual Author Contribution Statement: Conceptualization, J.L, and S.M.; methodology, J.L.; formal analysis, J.L, S.M., J.P, R.D. and K.J.D.; data curation, J.L.; writing-original draft preparation, S.M. and J.P.; writing-review and editing, J.L, S.M, J.P., R.D., and K.J.D.; project administration: J.L and S.M.; supervision, J.L. All authors have read and agreed to the published version of the manuscript.
Competing Interest Disclosure Statement: All authors listed state that they have no relevant material or financial interests or conflicts related to this paper.
Patient Informed Consent: The authors state that they have followed the principles outlined in the Declaration of Helsinki for all human experimental investigations. The authors state that they have obtained verbal and written informed consent from the patient for the inclusion of their medical and treatment history within this case report. As this is a case report, this does not meet the federal DHHS requirements for human subject’s research and thus, IRB approval is not required for this case.
References
- Moran DS, Evans RK, Hadad E (2008) Imaging of Lower Extremity Stress Fracture Injuries. Sports Medicine 38(4): 345-356.
- Schneiders AG, Sullivan SJ, Hendrick PA, et al. (2012) The Ability of Clinical Tests to Diagnose Stress Fractures: A Systematic Review and Meta-analysis. Journal of Orthopaedic & Sports Physical Therapy 42(9): 760-771.
- Matcuk GR, Mahanty SR, Skalski MR, Patel DB (2016) Stress fractures: pathophysiology, clinical presentation, imaging features, and treatment options. Emergency Radiology 23(4): 365-375.
- Wright AA, Hegedus EJ, Lenchik L, Kuhn KJ (2015) Diagnostic Accuracy of Various Imaging Modalities for Suspected Lower Extremity Stress Fractures. The American Journal of Sports Medicine 44(1): 255-263.
- Mettler FA, Huda W, Yoshizumi TT, Mahesh M (2008) Effective Doses in Radiology and Diagnostic Nuclear Medicine: A Catalog. Radiology 248(1): 254-263.
- Nussbaum ED, Holtzman B, Rizzone K (2022) Evaluation and Diagnosis of Tibial Bone Stress Injuries in Adolescents: Imaging and Nomenclature. Journal of the Pediatric Orthopaedic Society of North America 4(1): 1-13.
- Pegrum J, Crisp T, Padhiar N (2012) Diagnosis and management of bone stress injuries of the lower limb in athletes. BMJ 344.
- Bureau NJ, Ziegler D (2016) Economics of Musculoskeletal Ultrasound. Current Radiology Reports 4(8).
- Jacobson JA (2009) Musculoskeletal Ultrasound: Focused Impact on MRI. American Journal of Roentgenology 193(3): 619-627.
- Poenaru D (2023) Ultrasound diagnostic: Rapid detection of second metatarsal stress fracture, case report and literature study.
- Howard CB, Lieberman N, Mozes G, Nyska M (1992) Stress fracture detected sonographically. American Journal of Roentgenology 159(6): 1350-1351.
- Bodner G, Stockl B, Fierlinger A, Schocke M, et al. (2004) Sonographic findings in stress fractures of the lower limb: preliminary findings. European Radiology 15(2): 356-359.
- Banal F (2005) Ultrasound ability in early diagnosis of stress fracture of metatarsal bone. Annals of the Rheumatic Diseases 65(7): 977-978.
- Jones, SL, Phillips, M (2010) Early Identification of Foot and Lower Limb Stress Fractures using Diagnostic Ultrasonography: A review of 3 cases. The Foot and Ankle Online Journal.
- Battaglia PJ, Kaeser MA, Kettner NW (2013) Diagnosis and serial sonography of a proximal fifth metatarsal stress fracture. Journal of Chiropractic Medicine 12(3): 196-200.
- Arni D, Lambert V, Delmi M, Bianchi S (2009) Insufficiency fracture of the calcaneum: Sonographic findings. Journal of Clinical Ultrasound 37(7): 424-427.
- Bianchi S, Luong DH (2017) Stress Fractures of the Calcaneus Diagnosed by Sonography: Report of 8 Cases. Journal of Ultrasound in Medicine 37(2): 521-529.
- Bianchi S, Luong DH (2014) Stress fractures of the ankle malleoli diagnosed by ultrasound: a report of 6 cases. Skeletal Radiology 43(6): 813-818.
- Kim HJ, Park YH, Kim JY, Choi GW (2021) Role of Ultrasound in Early Diagnosis of Stress Fracture: A Case Report of Bilateral Distal Fibular Stress Fracture in a Female Recreational Badminton Player. Journal of the American Podiatric Medical Association 111(1).
- Hoglund LT, Silbernagel KG, Taweel NR (2015) Distal Fibular Stress Fracture in A Female Recreational Runner: A Case Report with Musculoskeletal Ultrasound Imaging Findings. PubMed 10(7): 1050-1058.
- Khy V, Wyssa B, Bianchi S (2012) Bilateral stress fracture of the tibia diagnosed by ultrasound. A case report. Journal of Ultrasound 15(2): 130-134.
- Amoako A, Abid A, Shadiack A, Monaco R (2017) Ultrasound-Diagnosed Tibia Stress Fracture: A Case Report. Clinical Medicine Insights: Arthritis and Musculoskeletal Disorders.
- Farkash U, Naftal J, Deranze E, Blankstein A (2008) Ultrasonography as A Diagnostic Modality of Tibial Stress Fractures. Journal of Musculoskeletal Research 11(02): 55-61.
- Nissen T, Wynn R (2014) The clinical case report: a review of its merits and limitations. BMC Research Notes 7(1).
- Marshburn TH, Legome E, Sargsyan A (2004) Goal-Directed Ultrasound in the Detection of Long-Bone Fractures. Journal of Trauma and Acute Care Surgery 57(2): 329.
- Nicholson JA, Tsang STJ, MacGillivray TJ, Perks F (2019) Simpson AHRW. What is the role of ultrasound in fracture management? Bone & Joint Research 8(7): 304-312.
- Brien AJ, Moussa MA (2020) Using ultrasound to diagnose long bone fractures. JAAPA 33(2): 33-37.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




