Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2638-6003
Case Report(ISSN: 2638-6003) 
The Implementation of the Integrative Cognitive Rehabilitation Psychotherapy Model in a Pediatric Concussion Clinic Volume 6 - Issue 2
Mark Pedrotty*
- Professor Emeritus, Pediatrics, Carrie Tingley Hospital, University of New Mexico, USA
Received:September 29, 2022; Published: October 12, 2022
Corresponding author: Mark Pedrotty, Professor Emeritus, Pediatrics, Carrie Tingley Hospital- University of New Mexico, 1127 University Blvd NE, Albuquerque, NM 87103, USA
DOI: 10.32474/OSMOAJ.2022.06.000232
Abstract
Introduction: The Integrative Cognitive Rehabilitation Psychotherapy (ICRP) model is essential in treating co-occurring issues in pediatric concussions. Knowledge of this model allows clinicians to identify co-occurring issues that can complicate recovery and refer to appropriate treatment team members to appropriately set treatment goals and maximize outcome.
Discussion: The ICRP model is described and application to different types of patients provided. Three cases with different complexity are reviewed.
Conclusion: The majority of pediatric concussions resolve quickly. However, the symptoms for many pediatric concussions can linger for a year of more. Identifying co-occurring issues and applying the ICRP model results in participation in treatment and positive outcome.
Introduction
Pediatric concussions are common and typically resolve quickly. However, many pediatric concussions are not simple, and symptoms can continue to be present up to a year post injury. Identifying co-occurring issues and treating accordingly can engage the patient and family in treatment and maximize outcome. The Integrative Cognitive Rehabilitation Psychotherapy (ICRP) model [1] provides a format to treat complex pediatric concussions.
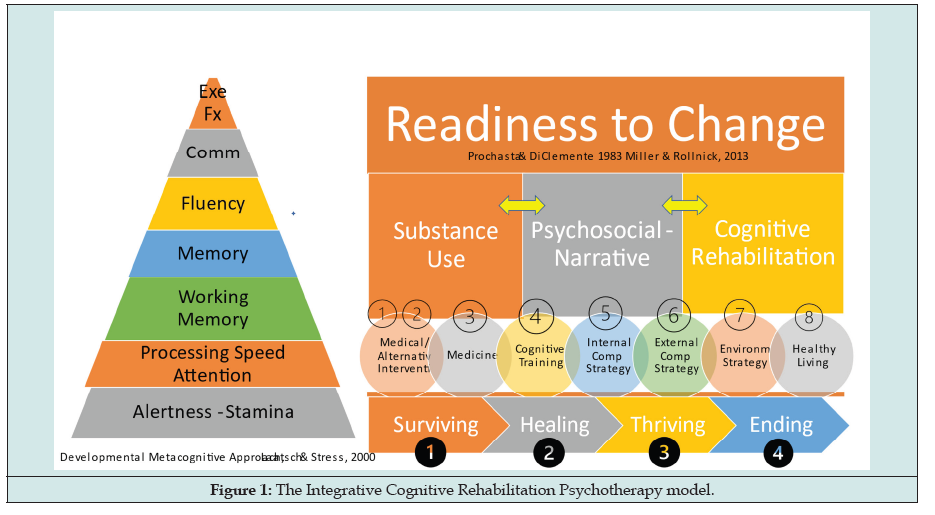
The ICRP model assesses the quantity and quality of cooccurring elements (cognitive, psychosocial, biological, and substance use) to develop goals and objectives that are culturally sensitive and specific to the stage of recovery (i.e., surviving, healing, thriving, and maintaining). The goals and objectives include eight interventions (medical, complementary and alternative medicine, healthy lifestyle, medication, environmental strategies, external compensatory strategies, internal compensatory strategies, and cognitive retraining or training). The goals and objectives include any of the seven cognitive areas (alertness and stamina, attention and problem solving, working memory, memory, communication, fluency, and executive functioning) that might be impaired and accommodate treatment of co-occurring issues to integrate the cognitive issues into care. Readiness to change is assessed in determining level of awareness and insight into issues and creating client-centered and culturally sensitive goals and objectives. An interdisciplinary or transdisciplinary team provides ongoing assessment and cross communication in creating and implementing treatment strategies. Emergent issues and engagement in treatment issues are managed by the team through ongoing communication. Initial assessment establishes which experts on the team focus on what issues. The primary care provider (PCP) or sports medicine provider (SMP) identifies what co-occurring issues are present and refers to the appropriate experts to treat related co-occurring issues. The complexity of the case drives the involvement of experts on the team. A review of different complex cases will be discussed.
Readiness to change is assessed in determining level of awareness and insight into issues and creating client-centered and culturally sensitive goals and objectives. (add in here See Figure 1). An interdisciplinary or transdisciplinary team provides ongoing assessment and cross communication in creating and implementing treatment strategies.
Discussion
Case I
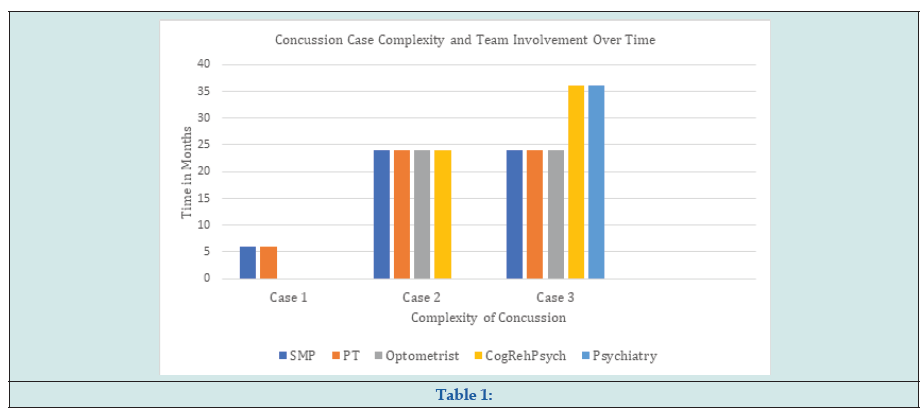
Adolescent suffers a third concussion within the year playing sports, and recovery is slower than recovery from previous concussions. Vestibular, ocular and motor issues, cognitive slowness, memory issues, light and sound sensitivity, and headaches are present. The sports medicine physician (SMP) or primary care physician (PCP) manages the headaches and sleep issues and refers to physical therapist (PT) who treats the vestibular ocular and motor issues. Cognitive, memory, and sensitivity to light and sound issues resolve as treatment progresses. Return to learn protocol was implemented, and over time, the adolescent returned to school with accommodations and then without accommodations. Return to play was discussed with patient and family by SMP or PCP.
Case 2
Latency age child with mild TBI was treated by SMP, PCP, PT, occupational therapy (OT) and speech therapy (SLP). Rehabilitation psychologist was added to the treatment team as psychological and cognitive issues continued and treatment goals and objectives were integrated across disciplines Cognitive issues are identified and worked on simultaneously with psychological issues to incorporate emotional regulation, trauma resolution and compensatory strategies into managing symptoms. Headaches and nausea persist, so vision evaluation and treatment of persistent visual issues are integrated into treatment. Resolution of vision issues resulted in resolution of headaches and nausea and improvement in academic, cognitive, and psychological functioning. Student was able to participate in school without accommodations and engage in extracurricular and community activities without issues.
Case 3
Young adult suffers multiple concussions as an adolescent engaging in recreational activity and then in return to play in a school sport. One year post initial concussions, the symptoms continue. The SMP or PCP, PT, optometrist, and rehabilitation psychologist work on co-occurring issues. Symptoms improve initially. Psychosocial and cognitive issues worsen resulting in reduced engagement in other therapies and emergent care. Psychiatric care is added to the treatment team to manage serious psychiatric issues, while rehabilitation psychologist and counselor focus on accommodations for cognitive and psychological issues to improve engagement in other therapies and develop appropriate coping skills and compensatory strategies. Concussion symptoms begin to resolve, and management of the psychiatric symptoms with accommodations for cognitive and psychological issues become the focus of care (Table 1).
Conclusion
These case studies support the benefits of applying the ICRP model to the care of pediatric and young adult concussion. The essential element to the model is the integrative treatment of cooccurring issues that would be ignored or inadequately treated using traditional care that does not accommodate for the cognitive issues and the relationship of those issues to treatment of co-occurring issues. An important component of ICRP is the application of an interdisciplinary or transdisciplinary model in setting goals and objectives across co-occurring issues and the simultaneous care of several co-occurring issues. Working through stages of recovery in developing appropriate goals and objectives and accommodations across interventions for cognitive issues is essential to engagement in therapy and good outcome.
Thanks to Drs. T. Sim-Wong and E. Wilde for helpful comments on manuscript and staff and families in the pediatric concussion clinic for their teamwork.
References

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...