Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2638-6003
Research Article(ISSN: 2638-6003) 
Quantitative Ultrasound to Assess Pain in Adult Tendons Volume 6 - Issue 1
Anthony Tran, Kalvin Zee, Thien Ngo, Edwin Davis and Jing Gao*
- Department of Radiology, Rocky Vista University, USA
Received: March 23, 2022; Published: April 07, 2022
Corresponding author: Jing Gao, MD, FAIUM, Director of Ultrasound, Rocky Vista University 255 E. Center Street, Ivins, UT 84738, USA
DOI: 10.32474/OSMOAJ.2022.06.000227
Abstract
Abstract
The study aimed to assess the change in patellar and quadriceps tendon stiffness measured by ultrasound shear wave elastography (SWE) in individuals with knee pain. A total of 124 tendons were scanned using a commercial a linear array ultrasound transducer (8 MHz). Of the tendons 40 were affected with pain whereas 84 were unaffected with pain. Shear wave velocity (SWV, m/s) measurements of the longitudinal tendons were taken twice with the participant supine and knee flexed (30 degrees). The tendons were divided into two groups: affected tendons and unaffected tendons based on the presence of pain. The difference between affected and unaffected tendons was examined using independent grouped t-tests. Intraobserver and interobserver reliability in performing SWE was tested using intraclass correlation coefficient (ICC). The average SWV of affected quadriceps tendons was higher than that of unaffected quadriceps tendons (5.26 m/s vs 4.501 m/s, p=0.04). For the patellar tendon, the average SWV in affected tendons was also higher than that in unaffected patellar tendons (5.42 m/s vs 4.778 m/s, p=0.04). Intraobserver and interobserver reliability for shear wave measurements was good (ICC, 0.90-0.97). The results demonstrate the effectiveness of ultrasound SWV in the assessment of the change in quadriceps and patellar tendon stiffness associated with knee pain.
Keywords: Knee pain; patellar tendon; quadriceps tendon; shear wave elastography; shear wave velocity; ultrasound
Keywords: SWE: Shear Wave Elastography; SWV: Shear Wave Velocity; ICC: Intraclass Correlation Coefficient; CT: Computed Tomography; MRI: Magnetic Resonance Imaging; ARFI: Acoustic Radiation Force Impulse; BMI: Body Mass Index
Introduction
Knee pain accounts for roughly 500,000 health provider visits per year [1]. This warrants the use of imaging modalities to provide reliable structural and functional information associated with the pain. These modalities include plain X-ray film, computed tomography (CT), magnetic resonance imaging (MRI), and ultrasound [2]. Of these choices, the American College of Radiology Appropriateness Criteria recommends plain film as the first-line diagnostic tool [3]. However, plain film is limited in its ability to identify soft tissue injuries such as ligamentous, tendon, and muscular injuries [4,5]. MRI has high image resolution and is feasible to assess skeletal abnormalities [5]. Although MRI is effective at visualizing soft tissue injuries, its practicality in a clinical setting is limited due to its low accessibility and high cost. An alternative to MRI is ultrasound, which has several inherent benefits over MRI. These include high availability, accuracy, mobility, demonstration of real-time soft tissue abnormalities, and low cost [6,7]. Classically, conventional ultrasound provides gray-scale images, which is known as B-Mode Imaging. B-Mode image displays only structural abnormalities within the knee such as joint effusions, popliteal cysts, and hematomas [8]. However, B-Mode alone cannot assess a tissue’s biomechanical properties or function of the knee. New developments in ultrasound technology, such as ultrasound shear wave elastography (SWE), resolves these issues with its capability to evaluate biomechanical properties of the tissue [9].
SWE can identify changes within tissues by measuring their elastic modulus. It produces a measurement of shear wave velocity (SWV, m/s) which provides qualitative and quantitative information for diagnostic purposes [6]. SWV is the speed at which a shear wave propagates through a tissue. This shear wave is achieved by emitting a wave of ultrasound pulses from the transducer to displace the soft tissues within its direct path. These waves travel faster through stiffer tissues and slower through softer tissues. In other words, SWV is high in stiff tissue and low in soft tissue [6,7]. SWE has shown to be an effective tool in diagnosing different pathologies, ranging from solid breast masses to liver fibrosis, kidney cortex stiffness, poststroke spasticity, and soft tissue injuries [10-14]. When evaluating soft tissue pathologies using SWE, an increase or decrease in SWV is noted depending on the structure and injury. For example, Achilles and supraspinatus tendinopathy are associated with a decreased SWV, whereas muscular spasticity, neuropathies, and low back and neck pain are associated with an increased SWV [10, 15-19]. The positive correlation between muscular pain and SWV value has been observed in patients with lower back or neck pain, superficial and deep multifidus, and trapezius, sternocleidomastoid, and splenius capitis [16-19]. Previous studies focused on the correlation between subjective pain within muscles and SWV; however, the knee joint consists primarily of ligaments and tendons in addition to related muscles [20]. The aim of this study was to assess the feasibility of ultrasound SWE to quantify the change in tendon stiffness associated with knee pain.
Methods/Material
Participants
The Institutional Review Board approval for this research study was provided through Rocky Vista University (IRB#2019- 0088). Participants were randomly selected from the from the local community. Inclusion criteria required the study participants to be 20 years of age or older, capable of understanding and signing informed consent, to be tolerant to ultrasonography scans, and having no history of lower extremity surgeries. After providing written informed consent, a standardized questionnaire state questionnaire on musculoskeletal pathologies regarding the lower extremities, the grade of knee pain (level 0-10), and other medical conditions were completed by all participants before scanning. Based on this information, individual knees with reported pain were categorized in the affected group (with pain) whereas the side without pain was categorized in the unaffected group (without pain).
Ultrasound Shear Wave Elastography (SWE)
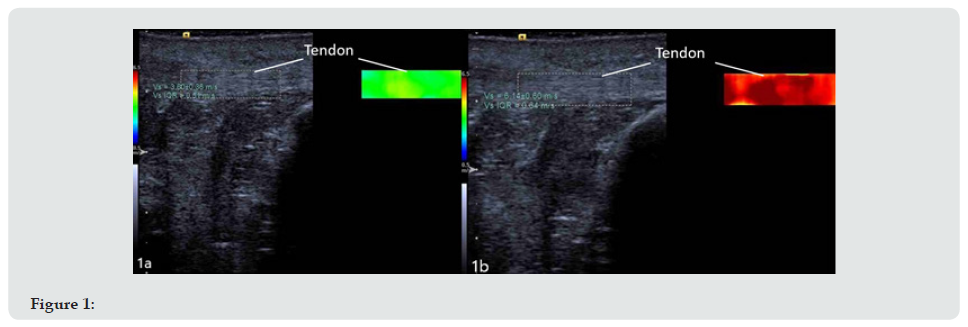
Ultrasound images were taken with a commercial Acuson S3000 ultrasound scanner (Siemens Medical Solutions, Mountain View, CA). A linear array transducer (9L4, bandwidth 4-9 MHz) was used to image the knees. Acoustic radiation force impulse (ARFI)- based point SWE software (Virtual Touch Quantification, Siemens) was installed in the scanner, and manufacture-recommended presettings were applied for acquiring SWE of the tendons. A double image function simultaneously displayed the B-mode image and the color-coded SWV map. Side by side, B-mode images provided anatomic information about the tendon and color-coded SWE displays the stiffness of the tendon (Figure 1). The participant was in a supine position with the knee flexed at 30 degrees for measuring SWV of the patellar tendon and quadriceps tendon. A pillow was placed under the knee to ensure relaxation and stability of the lower extremities. Each tendon was scanned twice in the longitudinal plane (elongate to tendon fibers). The region of interest for the color-coded shear wave elastography map of the tendon was 0.83 cm² (0.55 cm in axial by 1.5 cm in lateral) at the center of the tendon (Figure 1a). A homogenous green appearing in the SWE quality map was used to determine a high quality of SWE acquisition for data analysis. The mean and standard (SD) values of SWV for each tendon were displayed on the image based on estimation of shear wave speed in the ROI. Two SWV values were measured for each tendon and the average of these SWV values was used for analysis. SWV’s were measured two times in the patellar tendon and quadriceps tendon in the knee relaxation. Two operators scanned the patella tendons in 10 participants to test inter-observer reproducibility. An operator scanned patella tendons in the same 10 participants twice to test intra-observer repeatability. All operators had 2 years of training on how to perform ultrasound scan (abdomen, MSK, cardiovascular) and 5 hours of training on how to perform SWE (how to activate SWE function, how to measure SWV of the tendon, select ROI, and how to position the knee) in the study.
Statistical analysis
The age, body mass index (BMI), and all ultrasound parameters are expressed by the mean and standard deviation (SD). Differences in shear wave velocities between affected and unaffected tendons were analyzed by an independent grouped t-test. A p<0.05 was considered statistically significant. Intra- and inter-observer reliability was examined by intraclass correlation coefficient (ICC). ICC is interpreted by poor, moderate, or good correlation based on r-value [21]. Statistical analysis was conducted using commercial SPSS software (SPSS, version 27.0).
Results
Table 1: Average Shear Wave Velocities of the quadriceps tendon (top) and patellar tendon (bottom). There is statistical significance between painful and non-painful quadriceps (p=0.04) and painful and non-painful patellar tendons (p=0.04). Statistical significance was examined using an independent grouped t-test.

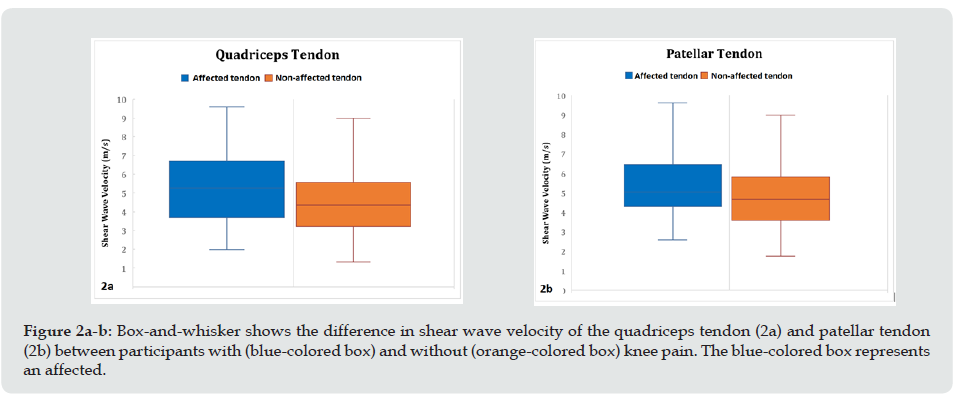
total of 31 adult participants (20 females, 11 males) were recruited. Each tendon was scanned twice and categorized based on the presence of the pain within the knee. There were 40 affected tendons and 84 unaffected tenons. SWV of 40 affected quadriceps and patellar tendons measured 5.26±2.00 m/s and 5.42±1.54 m/s, respectively (Table 1). The SWV of 0 unaffected quadriceps and patellar tendons measured 4.50±1.81 m/s and 4.77±1.62m/s, respectively (Figure 1 & Table 1). A statistically significant difference in SWV between affected and unaffected tendons was found in this study. The quadriceps tendon (p = 0.04) and patellar tendon (p = 0.04) both showed higher SWV in affected tendons compared to that in unaffected tendons (Figure 2). Intraobserver and interobserver reliability for shear wave measurements was good (ICC = 0.90-0.97) (Table 2).
Figure 2: Box-and-whisker shows the difference in shear wave velocity of the quadriceps tendon (2a) and patellar tendon (2b) between participants with (blue-colored box) and without (orange-colored box) knee pain. The blue-colored box represents an affected. Table 2: Reliabili
Discussion
We observed a higher SWV in the affected quadriceps tendons (p = 0.04) and patellar tendons (p = 0.04) compared to unaffected tendons. The result suggest that tendon stiffness (mechanical properties) increases in the knee associated with pain. SWE allows for the assessment of the stiffness of tissue scanned. The speed of shear wave propagation (SWV) through the tissue is dependent on the stiffness of the tissue. SWV is high in stiff tissue and low in soft tissue [22,23]. Our results indicate an increase in shear wave velocity represents increased stiffness in affected tendons. The likely cause of the pain experienced by our participants is tendon injury, which results in an inflammatory response, generating a release of cytokines and other pain modulators [24]. Other physiological changes that occur following tendon injury include architectural changes because of haphazard healing, inflammation, and collagen degeneration [25]. These changes cause an observed increase in tendon thickness and cross-sectional area, and ultimately an increase in tendon stiffness represented by SWV value [25,26]. Current research on the evaluation of tendon injury using SWE shows a variety of changes after an injury. In Achilles tendon injuries, normal tendons were stiffer than pathologic tendons [27, 28].
With regards to the supraspinatus tendon, the results of several studies were in line with our data, showing painful supraspinatus tendons will have a higher SWV [29], and an increase in SWV in individuals with idiopathic adhesive capsulitis [30]. Other studies have shown that increased shear wave velocities are associated with increased stiffness in plantar flexing muscles, infraspinatus, and lower trapezius, with resultant shoulder pain [31, 32]. When examining the tendons of the knee, the results of studies are contradictory. Some studies indicate an increase in SWV due to patellar tendon pathology [33,34], while others indicate a decrease [35, 36]. It is speculated that the variation results from differences in the location of the region of interest measured [37]. Studies that demonstrated a decreased SWV had a more variable region of interest, while studies demonstrating an increased SWV was standardized to a specific point in the tendon. To minimize variations in regions of interest, we chose a region of interest at the center of the tendon, like that of Coombes, et al. [36,37]. The patient population and criteria were also different in our study compared to previous studies. Previous studies included a patient population of only athletes [33,34] or individuals with patellar tendinopathy [35,36], whereas we chose a broad population consisting of athletes and nonathletes and looked solely on whether pain was present. Our results are backed by the fact that in a separate study performed, individuals with healthy patellar tendons were described as soft or having a low SWV [38]. Furthermore, after total knee arthroplasty, researchers showed SWV of the quadriceps tendon and the patellar tendon was higher before surgery than after surgery [39]. This may indicate that after the correction of knee pain, there will be a reduced stiffness in the nearby tendons. Intraclass Correlation Coefficient determined that the interobserver and intraobserver reliability was good (ICC, 0.90-0.97). This is in line with previous studies which show that the SWV to access various musculoskeletal pathologies is reproducible and reliable [35,40].
There were limitations in the study. First, the study lacks participants in variable age groups. The tendon stiffness increases with age. Confounding factors such as tissue change with age should be considered when assessing tendinopathy [41]. Aging can alter the spatial variations in Achilles tendon elasticity, resulting in deformations within the muscle-tendon unit affecting injury potential [42]. Second, we did not analyze the difference in SWV between men and women. Females were found to have a significantly higher Q-angle and hip joint internal rotation angle, which correlated with a higher proportion of females with a history of lower limb sports injuries [43]. Third, our data does not differentiate between types of lower limb pathologies. Different pathologies can result in different SWV values between the quadriceps and patellar tendons. Fourth, we did not examine the difference in SWV of the tendon between athletes and non-athletes. An increase in physical activity has been shown to have increased connective tissue remodeling and increased tendon collagen [26]. This could lead to changes in SWV in athletes. Fifth, we did not have electromyogram as a reference to correlate with pain and ultrasound findings. Finally, pain was used for dividing tendons into affected and unaffected groups. The pain is subjective because the variation of threshold for pain could be huge. However, the study demonstrated that SWE was feasible to distinguish the affected tendon with pain from those unaffected tendons without pain. As such, patients could be placed in different groups based on a subjective measurement. Further studies should use expanded criteria regarding gender, age, and past injury history to the lower limb to stratify participants to provide more detail regarding differences in SWV.
Conclusion
Ultrasound shear wave elastography is feasible to assess the change in tendons associated with knee pain. There is a positive correlation between SWV and knee pain. SWV can be used as a surrogate biomarker to quantify the change in tendons with pain and assess the effect of the treatment for knee pain. Figures 1a-b. Shear wave elastography was performed on a 67-year-old male without knee pain (1a) and 73-year-old woman with knee pain (1b). A linear array transducer (9L4, bandwidth 4-9 MHz) was placed longitudinally on the patellar tendon. Shear wave elastography shows longitudinal plane of the patellar tendon of an unaffected knee. B-mode image (left image) and color-coded SWE (right image) are displayed side by side Mean and standard deviation (SD) of shear wave velocity in unaffected tendon (1a) and affected tendon (1b) was 3.60 + 0.36 m/s and 6.14 + .60 m/s, respectively. The picture on the left indicates a B-Mode image of the tendon while the picture on the right indicates relative stiffness of the tissue with blue/green indicating minimal stiffness and red indicating increased stiffness.
Declarations
Informed consent was given by patients. Ethics approval was given by Rocky Vista University College of Osteopathic Medicine (IRB #2019-0088). There is no financial interest to declare. We acknowledge Siemens Healthineers for loaning the equipment to support the study.
Data Availability
Data is available upon request to the authors.
Acknowledgements
The following manuscript was presented as an oral presentation at the 2021 Scientific Program: Journal of Ultrasound in Medicine.
References
- Niska R, Bhuiya F, Xu J (2010) National Hospital Ambulatory Medical Care Survey: 2007 emergency department summary. Natl Health Stat Rep 6(26): 1-31.
- Hals, Gary, Steven Cruea, Dusty Moses (2007) "Evaluation of the Acutely Injured Knee in the ED: Diagnosis and Treatment: Part I." Emergency Medicine Reports 28(10): 101-111.
- Expert Panel on Musculoskeletal Imaging, Taljanovic MS, Chang EY, Ha AS, Bartolotta RJ, Bucknor M, et al. (2020) ACR Appropriateness Criteria® Acute Trauma to the Knee. J Am Coll Radiol 17(5S): 12-25.
- Gage BE, Mclivain NM, Collins CL, et al. (2012) Epidemiology of 6.6 million knee injuries presenting to United States emergency departments from 1999 through 2008. Acad Emerg Med 19: 378-385.
- Ptasznik R, Feller, Bartlett J, Fitt G, Mitchell A, et al. (1995) The value of sonography: the diagnosis of traumatic rupture of the anterior cruciate ligament of the knee. AJR. Am. Roentgenol 164(6): 1461-1463.
- K Arda N, Ciledag E, Aktas BK, Aribas K Kose (2011) Quantitative assessment of normal soft-tissue elasticity using shear-wave ultrasound elastography. Am J Roentgenol 197(3): 532-536.
- Miller DL, Smith NB, Bailey MR, Czarnota GJ, Hynynen K, et al. (2012) Overview of therapeutic ultrasound applications and safety considerations [Internet]. Journal of ultrasound in medicine 31(4): 623-634.
- Klauser AS, Tagliafico A, Allen GM, Boutry N, Campbell R, et al. (2012) Clinical indications for musculoskeletal ultrasound: a Delphi-based consensus paper of the European Society of Musculoskeletal Radiology. European radiology 22(5): 1140-1148.
- MS Taljanovic, LH Gimber, GW Becker, L Daniel Latt, Andrea S, et al. (2017) Shear-Wave Elastography: basic physics and musculoskeletal applications. RadioGraphics 37(3): 855-870.
- De Zordo T, Chhem R, Smekal V, G Feuchtner, M Reindl, et al. (2010) Real-time sonoelastography: findings in patients with symptomatic achilles tendons and comparison to healthy volunteers. Ultraschall Med 31(4): 394-400.
- Hari S, Paul SB, Vidyasagar R, E Dhamija, A D Adarsh, et al. (2018) Breast mass characterization using shear wave elastography and ultrasound. Diagn Interv Imaging 99(11): 699-707.
- G Ferraioli, P Parekh, AB Levitov, C Filice (2014) Shear wave elastography for evaluation of liver fibrosis. J Ultrasound Med 33: 197-203.
- Hartung EA, Wen J, Poznick L, Furth SL, Darge K (2019) Ultrasound Elastography to Quantify Liver Disease Severity in Autosomal Recessive Polycystic Kidney Disease. J Pediatr 209: 107-115e5.
- Gao J, Rubin JM, Chen J, O'Dell M (2019) Ultrasound Elastography to Assess Botulinum Toxin A Treatment for Post-stroke Spasticity: A Feasibility Study. Ultrasound Med Biol 45(5): 1094-1102.
- Hou SW, Merkle AN, Babb JS, McCabe R, Gyftopoulos S, et al. (2017) Shear wave ultrasound elastography evaluation of the rotator cuff tendon. J Ultrasound Med 36(1): 95-106.
- Kantarci F, Ustabasioglu FE, Delil S, Deniz Cebi Olgun, Bora Korkmazer, et al. (2004) Median nerve stiffness measurement by shear wave elastography: a potential sonographic method in the diagnosis of carpal tunnel syndrome 24(2): 434-440.
- Murillo C, Falla D, Rushton A, Sanderson A, Heneghan NR (2019) Shear wave elastography investigation of multifidus stiffness in individuals with low back pain. J Electromyogr Kinesiol 47:19-24.
- Kuo WH, Jian DW, Wang TG, Wang YC (2013) Neck muscle stiffness quantified by sonoelastography is correlated with body mass index and chronic neck pain symptoms. Ultrasound Med Biol 39(8): 1356-1361.
- Taş S, Korkusuz F, Erden Z (2018) Neck Muscle Stiffness in Participants with and Without Chronic Neck Pain: A Shear-Wave Elastography Study. J Manipulative Physiol Ther 41(7): 580-588.
- Flandry F, Hommel G (2011) Normal Anatomy and Biomechanics of the Knee. Sports Medicine and Arthroscopy Review 19(2): 82-92.
- Popović ZB, Thomas JD (2017) Assessing observer variability: a user's guide. Cardiovasc Diagn Ther 7(3): 317-324.
- B Harmon, M Wells, D Park, J Gao (2019) Ultrasound elastography in neuromuscular and movement disorders. Clin Imaging 53: 35-42.
- SF Eby P, Song S, Chen Q, Chen JF, Greenleaf KN (2013) Validation of shear wave elastography in skeletal muscle. J Biomech 46(4): 2381-2387.
- Thomopoulos S, Parks WC, Rifkin DB, Derwin KA (2015) Mechanisms of tendon injury and repair. J Orthop Res 33(6): 832-839.
- Sharma P, Maffulli N (2006) Biology of tendon injury: healing, modeling and remodeling. J Musculoskelet Neuronal Interact 6(2): 181-190.
- Tardioli A, Malliaras P, Maffulli N (2012) Immediate and short-term effects of exercise on tendon structure: biochemical, biomechanical and imaging responses. Br Med Bull 103(1): 169-202.
- Aubry S, Nueffer JP, Tanter M, Becce F, Vidal C, et al. (2015) Viscoelasticity in Achilles tendonopathy: quantitative assessment by using real-time shear-wave elastography. Radiology 274(3): 821-829.
- De Zordo T, Fink C, Feuchtner GM, Smekal V, Reindl M, et al. (2009) Real-time sonoelastography findings in healthy Achilles tendons. AJR Am J Roentgenol 193(2): 134-138.
- Yoo SJ, Lee S, Song Y, Kim CK, Lee BG, et al. (2020) Elasticity of torn supraspinatus tendons measured by shear wave elastography: a potential surrogate marker of chronicity? Ultrasonography 39(2): 144-151.
- Yun SJ, Jin W, Cho NS, Ryu KN, Yoon YC, et al. (2019) Shear-Wave and Strain Ultrasound Elastography of the Supraspinatus and Infraspinatus Tendons in Patients with Idiopathic Adhesive Capsulitis of the Shoulder: A Prospective Case-Control Study. Korean J Radiol 20(7): 1176-1185.
- Vigotsky AD, Rouse EJ, Lee SSM (1985) Mapping the relationships between joint stiffness, modeled muscle stiffness, and shear wave velocity. J Appl Physiol 129(3): 483-491.
- Mifune Y, Inui A, Nishimoto H, et al. (2020) Assessment of posterior shoulder muscle stiffness related to posterior shoulder tightness in college baseball players using shear wave elastography. Journal of Shoulder and Elbow Surgery 29(3): 571-577.
- Ooi CC, Richards PJ, Maffulli N, Ede D, Schneider ME, et al. (2016) A soft patellar tendon on ultrasound elastography is associated with pain and functional deficit in volleyball players. J Sci Med Sport 19(5): 373-378.
- Dirrichs T, Quack V, Gatz M, Tingart M, Kuhl CK, et al. (2016) Shear Wave Elastography (SWE) for the Evaluation of Patients with Tendinopathies. Acad Radiol 23(10): 1204-1213.
- Zhang ZJ, Ng GY, Lee WC, Fu SN (2014) Changes in morphological and elastic properties of patellar tendon in athletes with unilateral patellar tendinopathy and their relationships with pain and functional disability. PLoS One 10(10): e108337.
- Coombes BK, Tucker K, Vicenzino B, Vuvan V, Mellor R, et al. (2017) Achilles and patellar tendinopathy display opposite changes in elastic properties: A shear wave elastography study. Scand J Med Sci Sports 28(3): 1201-1208.
- Prado-Costa R, Rebelo J, Monteiro-Barroso J, Preto AS (2018) Ultrasound elastography: compression elastography and shear-wave elastography in the assessment of tendon injury. Insights Imaging 9(5): 791-814.
- Porta F, Damjanov N, Galluccio F, Iagnocco A, Matucci-Cerinic M (2014) Ultrasound elastography is a reproducible and feasible tool for the evaluation of the patellar tendon in healthy subjects. Int J Rheum Dis 17(7): 762-766.
- Quack V, Betsch M, Hellmann J, Eschweiler J, Schrading S, et al. (2020) Evaluation of Postoperative Changes in Patellar and Quadriceps Tendons after Total Knee Arthroplasty-A Comprehensive Analysis by Shear Wave Elastography, Power Doppler and B-mode Ultrasound. Acad Radiol 27(6): e148-e157.
- Breda SJ, van der Vlist A, de Vos RJ, Krestin GP, Oei EHG (2020) The association between patellar tendon stiffness measured with shear-wave elastography and patellar tendinopathy-a case-control study. Eur Radiol 30(11): 5942-5951.
- Waugh CM, Blazevich AJ, Fath F, Korff T (2012) Age-related changes in mechanical properties of the Achilles tendon. J Anat 220(2): 144-155.
- Slane LC, Martin J, DeWall R, Thelen D, Lee K (2017) Quantitative ultrasound mapping of regional variations in shear wave speeds of the aging Achilles tendon. Eur Radiol 27(2): 474-482.
- Mitani Y (2017) Gender-related differences in lower limb alignment, range of joint motion, and the incidence of sports injuries in Japanese university athletes. J Phys Ther Sci 29(1): 12-15.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...