
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2638-6003
Case Report(ISSN: 2638-6003) 
Polypropylene Prosthesis in the Definitive Approach in Failure of Thumb Replantation: Case Report Volume 5 - Issue 5
José Martins Juliano Eustáquio1*, Alberto Martins Fontoura Borges, Vitor de Pina Pires1, Rafael Rosano Gotti Alves1, Marco Aurélio Sertório Grecco2 and Octávio Barbosa Neto3
- 1Mário Palmerio Hospital, University of Uberaba (UNIUBE), Uberaba, MG, Brazil.
- 2Clinical Hospital of the Federal University of Triângulo Mineiro, Uberaba, MG, Brazil.
- 3Sport and Exercise Cardiology Research Group, Department of Sports Sciences, Federal University of Ceará, Fortaleza, Brazil.
Received: February 9, 2022; Published: February 22, 2022
Corresponding author: José Martins Juliano Eustaquio, Hospital Mário Palmério- Bloco E Avenida Cecília Palmerio, s/n, Uberaba, MG, CEP: 38050175, Brazil.
DOI: 10.32474/OSMOAJ.2022.05.000224
Abstract
Traumatic amputations of the thumb are serious injuries that can have significant physical limitations and, consequently, cause harmful economic repercussions for the patient and the Health System. The main treatment options are replantation, grafts, autologous flaps, and synthetic materials. As a first option, replantation should always be attempted, provided that there are minimal technical conditions for performing the procedure. The use of synthetic polypropylene material shows good results in the primary treatment of fingertip injuries. Therefore, this case report aimed to demonstrate a viable treatment option for cases of thumb replantation failure. Evidence Level V; Therapeutic Studies; Expert Opinion.
Keywords: Traumatic Amputation; Thumb; Hand Injuries
Introduction/History
Traumatic amputations of the fingers are debilitating injuries that usually cause serious functional damage and economic losses to victims, especially of the thumb [1]. Of all the treatment options, replantation is the most effective way to restore the functionality of the anatomical segment. However, the number of finger replantations is considerably scarce worldwide, possibly due to the deficient training of orthopedists who work in Emergency Care Centers, as well to the lack of adequate structure for the procedure [2]. As long as the conditions of the amputated limb are satisfactory, replantation should always be tried, as it can represent the return of the finger function [3] and also a better relation between cost and benefit [4]. The success rates cannot be evaluated only by the viability of the segment, but by the return to the useful function. In any case, the patient’s profile must be collaborative, as the time for recovery from a replantation will be longer than for healing of a flap or similar procedure. In cases where finger replantation is not successful, flaps are the most frequently performed procedures.5 However, the technique described by Figueiredo et al. [6] which uses a temporary synthetic prosthesis is an inexpensive and effective procedure in most cases, it becomes a viable alternative for tissue coverage in these cases, especially when considering the economic reality of the health system in Brazil. The main goal of this case report was to describe the use of a polypropylene prosthesis, known for the treatment of primary lesions of the fingertips, after a failed thumb replantation procedure.
Case Report
A 35-year-old male patient, blue-collar worker, without comorbidities, smoker (20 years/pack), came to the Emergency Room, victim of an injury caused by an industrial centrifuge, with about 50 minutes of evolution. On physical examination, represented traumatic oblique volar amputation at the proximal level of the distal phalanx of the thumb, due to avulsion (Figure 1A). The company’s staff took the amputation stump of the finger in a refrigerated container (Figure 1B). Approximately three hours after the trauma, the patient was referred to the Surgical Center and, due to the conjuncture of factors (affected finger, time of trauma, conditions for sending the amputation stump, among others), the finger replantation was chosen, even if the service unit did not have microscopy equipment available and that the morphology of the wound was not favorable (avulsion). The patient was initially submitted to brachial plexus block, followed by surgical cleaning of the wound, debridement and identification of the structures to be repaired. The amputation stump, after debridement, was submerged in a 0.9% saline solution until replantation.
Figure 1: Clinical image of the wound, after initial washing in the Surgical Center. (B) Distal end of the thumb, in which an avulsion-type amputation is noted. Source: Author’s personal archive.

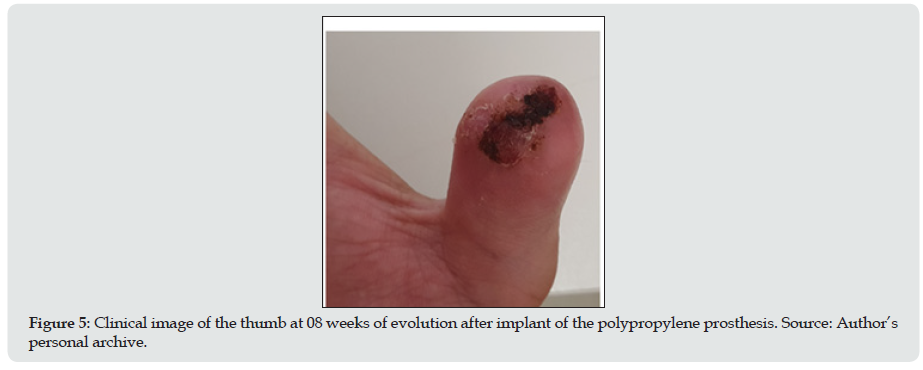
Soon after, the sequential replantation procedure began, with initial stabilization through osteosynthesis with a 1.5 mm Kirschner wire and repair or reconstruction of viable soft tissues. This procedure was initially performed by directly suturing the stumps of the long flexor tendon of the thumb, followed by reconstruction of the ulnar branch of the main artery, through a graft from the dorsal vein, by neurorrhaphy of the ulnar branch of the digital nerve, and finally, by suturing the wound (Figure 2A). The radial branch of the main artery of the thumb and the digital nerve were not possible to be repaired or reconstructed. Owing to the impossibility of performing venous repair or reconstruction, at the end of the procedure, two incisions of approximately 1 cm were made at the tip of the finger and Heparin infiltration was administered into the wound, both to allow continuous bleeding. In the follow-up, at 03 and 07 days after surgery, satisfactory perfusion of the finger was observed (Figure 2B). After 10 days of the procedure, apparently without triggering factor, the replanted segment started with cyanosis and decreased tactile sensitivity. The Kirschner wire was removed on the 12th day, in the attempt to improve the perfusion of the finger, but the segment evolved with distal necrosis around the 14th postoperative day (Figure 2C). Because of this evolution, on the 16th day a revision was made, the amputation stump was removed, and the polypropylene prosthesis was implanted (Figure 3A & 3B). At that time, there was a small distal bone exposure, which was completely covered by the prosthesis. After 06 weeks, the prosthesis (plastic saline) was removed and almost complete healing of the site was observed, with a small remaining area of granulation (Figure 4), which evolved satisfactorily in the following weeks (Figure 5), until healing complete around the eighth week after the procedure. The patient started physical therapy right after the removal of the polypropylene prosthesis and evolved with functional range of motion and normal thumb sensitivity.
Figure 2: Evolutionary images of thumb reimplantation, in the immediate postoperative period (A), on the 7th day (B) and on the 14th day (C) of evolution. Source: Author’s personal archive.
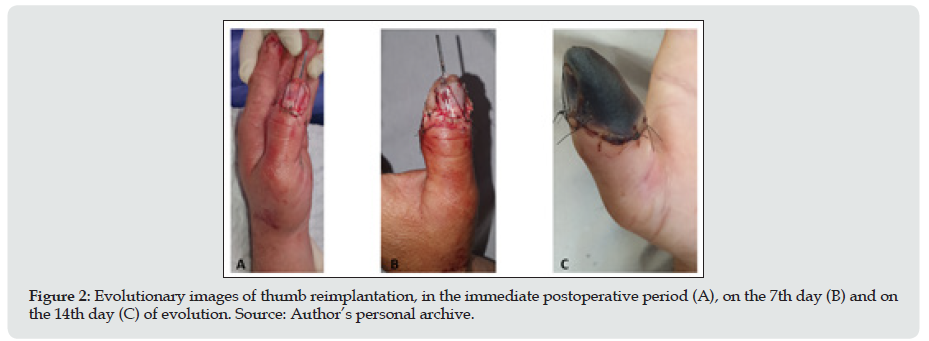
Figure 3: Implant of the polypropylene prosthesis and evolutionary images in the immediate postoperative period (A) and with 02 weeks of evolution (B). Source: Author’s personal archive.
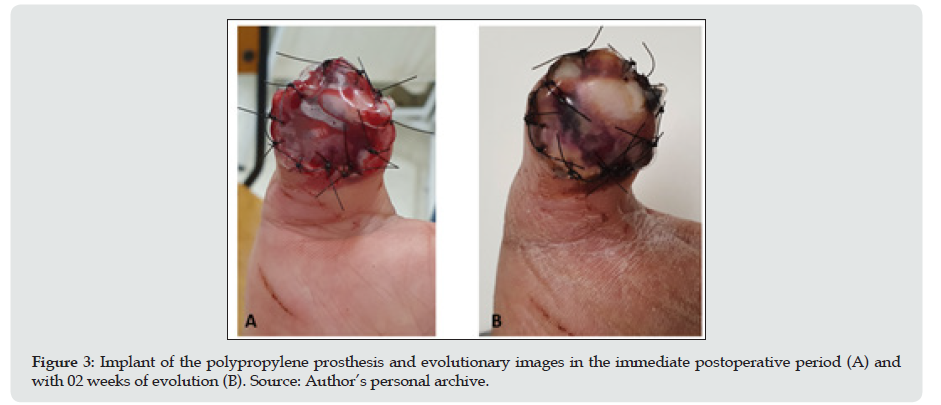
Figure 4: Evolution of healing of the thumb after removal of the polypropylene prosthesis, with 06 weeks of evolution. Source: Author’s personal archive.
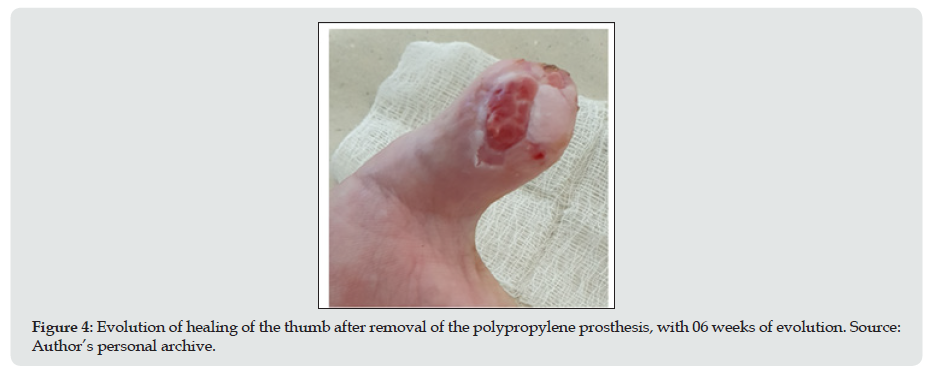
Figure 5: Clinical image of the thumb at 08 weeks of evolution after implant of the polypropylene prosthesis. Source: Author’s personal archive.
Discussion
This case report demonstrates an effective and inexpensive alternative to revision after thumb replantation, based on the great results of the technique in primary fingertip injuries [6]. The choice to perform the replantation should always be considered according to the surgeon’s experience and the clinical and local conditions of the amputated segment. However, for functional and economic reasons, it is a procedure that should always be prioritized, especially in injuries involving the thumb [1,4,7]. Ideally, replantations should involve the use of adequate instruments, mainly based on the microscopy technique, which allows for more accuracy performance of some procedures, such as vascular or nerve transpositions. But this is not a reality of vast majority emergency care services, not only in Brazil [8]. The unsatisfactory evolution of the case starting only in the second week leaves as the main hypothesis the peripheral microangiopathy resulting from the high tobacco load. Additionally, regarding the failure to perform a venous anastomosis, the literature shows robust results that it is not a causal factor for replantation failure.9 It is known that factors such as older age, motivation, associated injuries, systemic diseases (such as diabetes, systemic arterial hypertension, among others), addictions (such as smoking, alcohol, drugs), ischemia time and distal level of amputation predispose to failure of replantation [10]. For these cases, treatment alternatives are the flap, local or distant grafts and synthetic materials. Among these, the polypropylene prosthesis was described and is used to cover fingertip wounds [6]. This prosthesis is easily accessible and effective in protecting noble structures, especially in injuries of the volar oblique type, in which the use of flaps is more challenging. This technique offers biological and mechanical conditions for wound healing to occur [6]. The presence of polypropylene prosthesis induces the formation of a biochemically favorable environment, which provides coordinated healing and restoration of the anatomical shape of the finger. Plastic also provides mechanical protection to the healing tissue, in addition to preventing it from adhering to the dressing materials. It is also worth noting that the polypropylene prosthesis does not have the typical disadvantage of autologous grafts and flaps, which cause morbidity at the donor site. The literature brings good results with fingertip traumas using this technique [6] and, based on the current report, it becomes an attractive option for use in amputation reviews of this body segment.
Financial Support
There was no financial support from public, commercial or non-profitable sources.
Conflict of Interests
The author declares that there is no conflict of interest related to this case report Place where the case report was developed: Hospital Mário Palmerio, Universidade de Uberaba (UNIUBE), Uberaba, MG, Brazil.
References
- Harris AP, Goodman AD, Gil JA, Sobel AD, Li NY, et al. (2018) Incidence, timing, and risk factors for secondary revision after primary revision of traumatic digit amputations. J Hand Surg Am 43(11): 1040.e1-1040.e11.
- Hustedt JW, Bohl DD, Champagne L (2016) The detrimental effect of decentralization in digital replantation in the United States: 15 years of evidence from the National Inpatient Sample. J Hand Surg Am 41(5): 593e601.
- Zumiotti AV, Ohno PE, Guarnieri MV, Prada F (1995) Reimplante de dedos em amputações distais à articulação interfalângica distal Rev Bras Ortop 30(4): 197-200.
- Yoon AP, Mahajani T, Hutton DW, Chung KC (2019) Finger Replantation and Amputation Challenges in Assessing Impairment, Satisfaction, and Effectiveness (FRANCHISE) Group. Cost-effectiveness of Finger Replantation Compared with Revision Amputation. JAMA Netw Open 2(12): e1916509.
- Santos TPS, Oliveira MT, Angelini LC (2018) Estudo retrospectivo para avaliação do tratamento de lesões da polpa digital com retalho homodigital. Rev Bras Ortop 53(2): 200-207.
- Figueiredo LA, Ribeiro RS, Melo ALB, Lima AL, Terra BB, et al. (2017) Provides a polypropylene prosthesis for the treatment of finger injuries. Description of surgical technique and results. Rev Bras Ortop 52(6): 685-692.
- Stone N, Shah A, Chin B, McKinnon V, McRae M (2021) Comparing digital replantation versus revision amputation patient reported outcomes for traumatic digital amputations of the hand: A systematic review and meta-analysis. Microsurgery 41(5): 488-497.
- Fufa D, Calfee R, Wall L, Zeng W, Goldfarb C (2013) Digit replantation: experience of two U.S. academic level-I trauma centers. J Bone Joint Surg Am 95(23): 2127-2134.
- Huang HF, Yeong EK (2015) Surgical treatment of distal digit amputation: success in distal digit replantation is not dependent on venous anastomosis. Plast Reconstr Surg 135(1): 174-178.
- Chung KC, Yoon AP, Malay S, Shauver MJ, Wang L, (2019) FRANCHISE Group. Patient-Reported and Functional Outcomes After Revision Amputation and Replantation of Digit Amputations: The FRANCHISE Multicenter International Retrospective Cohort Study. JAMA Surg 154(7): 637-646.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




