Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2638-6003
Case Report(ISSN: 2638-6003) 
Meniscal Tear in a Toddler with Spontaneous Healing: A Case Report Volume 6 - Issue 1
Courtney Bull1* and Lisa Phillips2
- 1Department of Orthopedics, BC Children’s Hospital, Department of Orthopedics, Canada
- 2Department of Orthopedics, Alberta Children’s Hopsital, Canada
Received: February 22, 2022; Published: March 8, 2022
Corresponding author: Courtney Bull, BC Children’s Hospital, Department of Orthopedics, 4480 Oak Street, 1D Vancouver, BC V6H 3V4 Canada
DOI: 10.32474/OSMOAJ.2022.06.000226
Abstract
A meniscal tear in a very young child has not been reported in the literature. We report a case of a 12-month-old male who presented with a prolonged course of septic arthritis of the knee. A posterior horn radial tear to the periphery with extrusion of the meniscal body was arthroscopically diagnosed during irrigation and debridement for septic joint. The patient was treated with resolution of the septic arthritis but no repair was performed on the radial meniscal tear. Clinical and radiographic outcomes have been obtained over a 2-year follow-up period. The final follow-up MRI revealed spontaneous healing of the radial tear in the medial meniscus and resolution of meniscal extrusion.
Introduction
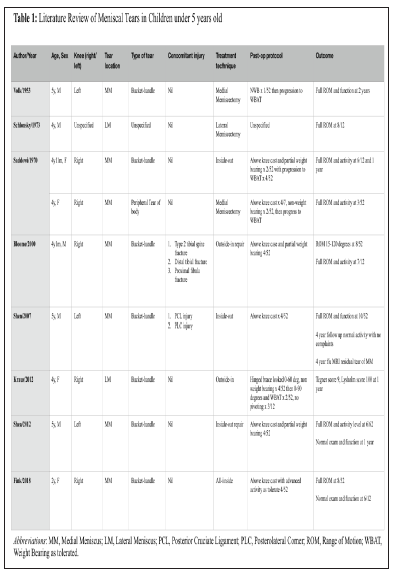
A 12-month-old male presented to the emergency department with a ten-day history of intermittent fever and atraumatic rightsided knee pain and swelling. He had developed a progressive inability to weight bear during this period. His parents reported a concurrent history of an upper respiratory tract infection. Upon initial presentation, the child refused to weight bear on the right lower extremity and demonstrated a moderate-sized knee joint effusion, diffuse tenderness upon palpation, and passive range of motion limited to 75 degrees of flexion due to patient discomfort. Standard laboratory tests, radiographic analysis and arthrocentesis confirmed the diagnosis of septic arthritis. An MRI was initially completed to evaluate for possible adjacent osteomyelitis. In retrospect, when the MRI was re-evaluated post-operatively it did demonstrate a radial tear in the posterior horn-body junction of the medial meniscus with some undersurface tearing extending into the body which was extruded (Figure 1).
Figure 1: T2-FS hypointense collections within the right knee joint extending to the suprapatellar region. Findings are consistent with septic arthritis of knee joint with associated soft tissue inflammatory changes. There is a radial tear of the posterior hornbody junction of the medial meniscus (A) with some undersurface tearing extending into the body which is extruded (B; arrow).
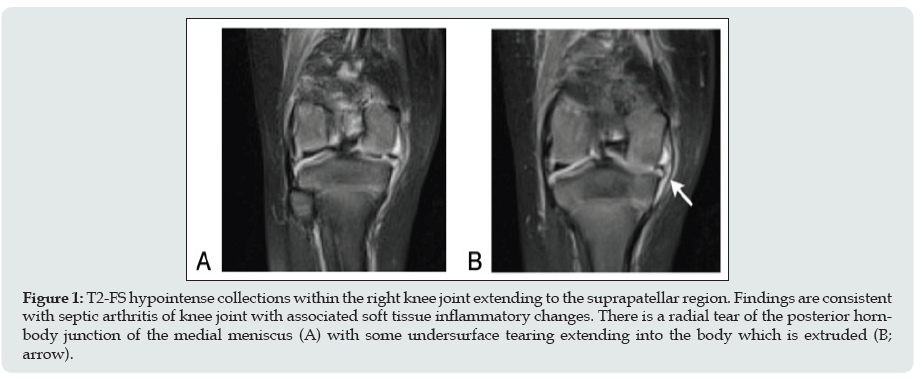
Arthroscopic irrigation of the knee and intravenous antibiotics were used to treat the septic arthritis of the knee. Standard arthroscopic portals were utilized. After a thorough irrigation with 6L of normal saline was completed, all inflamed synovial tissue was debrided, and a diagnostic arthroscopy was performed. Arthroscopic findings were remarkable for diffuse synovitis, central fraying in the medial meniscal body and a radial tear to the periphery at the posterior horn-body junction (Figures 2 A-C). The central fraying was minimally debrided with a shaver (Figure 2D). A decision was made intra-operatively to perform no further intervention with respect to radial tear within the posterior horn of the medial meniscus. Post-operatively, the patient had no activity restrictions and was treated with one week of intravenous cefazolin followed by two weeks of oral cephalexin. Upon discharge from hospital his clinical examination had improved significantly, and his bloodwork parameters had returned to within normal limits. At 2-year follow-up, the patient was completely asymptomatic and had no post-operative pain, mechanical symptoms or functional limitations. Upon examination, his gait was unremarkable, he had full range-of-motion compared to the contralateral side and no joint-line tenderness. Repeat MRIs were performed at 1- and 2- years postoperatively. This demonstrated complete spontaneous healing of the radial tear in medial meniscus and resolution of the meniscal body extrusion (Figure 3).
Figure 2: Medial meniscal tear in a toddler. Static arthroscopic images of the right knee, demonstrating an inflammatory synovitis secondary to a septic joint (A), a normal appearing lateral meniscus and lateral compartment (B), a radial tear within the posterior horn of the medial meniscus (white arrow) (C), as well as central fraying within the body of the medial meniscus (black arrow) seen before (C) and after debridement (D).
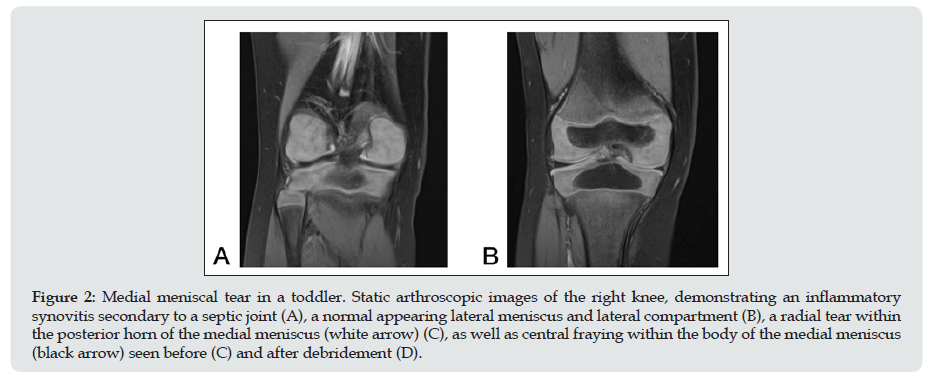
Figure 3: Two-year follow-up MRI. Coronal MRI images of the right knee demonstrates uniform low PD and T2 FS of the medial meniscus. There is evidence of healing of the posterior horn of the medial meniscus (A) and no further evidence of meniscal extrusion (B).
Systematic Literature Review
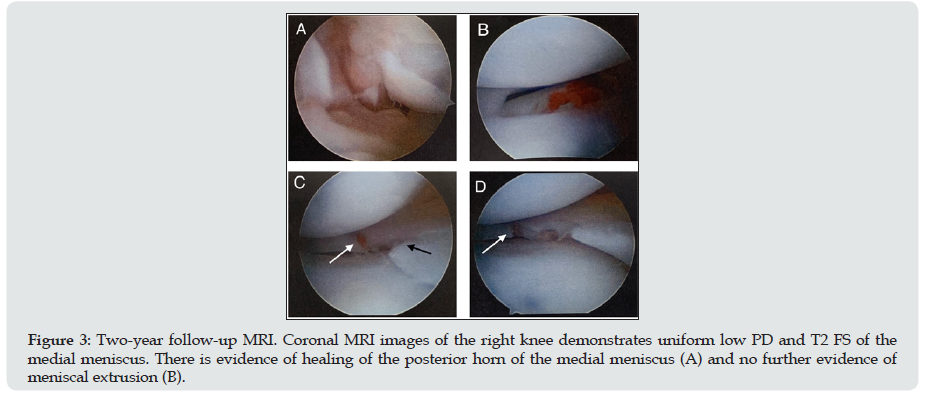
The literature was systematically reviewed using PubMed with the following medical subject headings (MESH): [“infant” or “child/preschool”] AND [“Meniscus” or “Meniscus/abnormalities” or “meniscus/diagnosis” or “meniscus/diagnostic imaging” or “meniscus/growth and development” or “meniscus/injuries” or “meniscus/pathology” or “meniscus/surgery” or “tibial meniscus injuries” or tibial meniscus injuries/diagnosis” or “tibial meniscus injuries/surgery” or “menisci, tibial/abnormalities” or “menisci, tibial/diagnostic imaging” or “menisci, tibial/diagnosis” or “menisci, tibial/surgery” or “knee injuries/surgery” ]. The search was last updated on November 28, 2020. The inclusion criteria for our literature search were as follows: studies reporting the outcomes of meniscal tears in patients 5-years-old or younger and English language studies. We excluded cadaveric studies and studies including discoid meniscus. All references from included studies were reviewed to ensure that no relevant articles were missing from the systematic search. Our search identified 295 citations from which relevant studies were selected for further review based on their abstract. Twelve articles were selected and available for full-text review. After a thorough review of these articles and their references, a total of 8 studies were included in the final analysis (Table 1).
Discussion
Traumatic isolated meniscal tears in skeletally immature patients are rare but well-described injuries. Several risk factors for meniscal injuries in the paediatric population exist, including adolescent age, male sex, increased BMI, concomitant ACL injury, and sports participation [1]. Although young people are at risk of meniscal injury due to their high level of activity, meniscal tears in individuals under 18-years-old occur with far less frequency compared to the adult population. The majority of meniscal tears seen in the very young paediatric population are more likely to be associated with a discoid meniscus configuration [2]. A systematic review of the literature was completed for this case report to improve upon the understanding of meniscal tears in very young children and to help define important factors that influence treatment options. This review highlights eight articles that discussed a total of 9 cases of meniscal tears in children aged five-years-old and under with otherwise normal menisci [3-10]. All 9 cases were bucket-handle type tears that were secondary to a traumatic aetiology. Three of the earliest reports on isolated meniscal tears in children younger than 5 years revealed good functional results following either partial or total meninscetomy [3- 5] Bloome, et al. was the first to report on 2 of the youngest patients with traumatic meniscal tears treated with surgical suture repair techniques [6]. Since then, the other 4 reported cases of mensical tear in this age group have also been treated with meniscal repair [7-10]. Regardless of surgical technique, all 9 cases demonstrated good outcomes at short-term follow-up. Overall, there have been no reported cases of children under the age of 2-years-old, making this case report of a 12-month-old child the youngest patient reported with an acquired meniscal tear. At birth, the developing meniscus is highly vascular, with the vasculature extending across the entire width of the meniscus. Throughout maturation there is a gradual decline in both cellularity and vascularity. By the age of 2 years an avascular inner circumference begins to develop, eventually progressing to only the peripheral 10-30% having a blood supply by adulthood [1]. In paediatric patients, it is postulated that this increased vascularity makes meniscal tears more amenable to healing following repair [9]. While radial tears that occur in the avascular one-third of the meniscus have little potential for healing in adults, perhaps the same is not true in the young child [11]. A recent systematic review has reported good to excellent outcomes of meniscal repairs in the paediatric population regardless of injury pattern, zone or surgical technique [12].
While meniscal tears in normal meniscal tissue in very young children is exceedingly rare, there are documented reports of meniscal tears in younger patients with discoid meniscal anomalies. Two case reports have described the treatment of symptomatic discoid meniscal tears in very young children. Lee et al, described excellent clinical results for a 26-month-old infant with a meniscal tear of a discoid lateral meniscus treated with a one-piece excision technique at 35-month follow-up evaluation [13]. In 2013 Fazio et al, reported good outcomes in a 32-month-old child treated with saucerization of a lateral discoid meniscus with repair of an associated unstable anterior horn tear at 3-month follow-up [14]. Very limited data is available for treatment strategies for meniscal tears in this paediatric age group, regardless of aetiology or predisposing factors, and more literature is required to understand these injuries along with the expected outcomes. Based on the current literature review, longitudinal and bucket-handle type meniscal tears were the most commonly reported pattern in children under 5-years-old. It has been hypothesized that children are predisposed to this tear pattern due to increased joint laxity, making radial tears relatively uncommon [9]. There is currently no consensus regarding optimal treatment strategy for radial tears of the meniscus, with various operative techniques revealing incomplete and non-anatomic healing [15]. This is the first reported case of spontaneous healing of radial meniscal tear which also happens to be in a very young child. This provides evidence for the healing capabilities of meniscal tearing in the young child and precedent for successful non-operative treatment in this age group. In the absence of meniscal repair, excellent clinical and radiographic outcomes were achieved at two years follow-up in the patient described.
A level of complexity is embedded in this case report, as the meniscal tear was an incidental finding in a child presenting with a septic joint. To the author’s knowledge, after a comprehensive literature search, there are no reported cases of meniscal tear resulting from a septic knee. It has been proposed that chronic infection may lead to meniscal mucoid degeneration and predispose patients to risk of meniscal tear; however, a recent study by Boya et al reveals no association between bacterial infection and mucoid degenerative pathology of the meniscus [16,17]. However, in the absence of a congenitally abnormal meniscus or history of trauma, we believe it is necessary to consider in this case that the meniscus tearing could have occurred as a result of the prolonged 10- day course of septic arthritis.
Conclusion
This is the first report of an isolated meniscus tear in a child this young and the first to suggest a possible association between joint infection and meniscal tearing in this age group. We have demonstrated spontaneous healing, without meniscal repair, of a radial meniscal tear with associated meniscal extrusion in a child of 12 months of age. It provides precedent for the non-operative management of meniscal tears in this age group.
References
- Jackson T, Peter D Fabricant, Nicholas Beck, Eileen Storey, Neeraj M Patel, et al. (2019) Epidemiology, Injury Patterns, and Treatment of Meniscal Tears in Pediatric Patients: A 16-year experience of a single center. Orthop J Sports Med 7(12): 2325967119890325.
- Kramer DE, Leslie A Kalish, Daniel J Martin, Yi-Meng Yen, Mininder S Kocher, et al. Outcomes after the operative treatment of bucket-handle meniscal tears in children and adolescents. Ortho J Sports Med 7(1): 2325967118820305.
- Volk H, Smith FM (1953) Bucket-handle tear of the medial meniscus in a five-year-old boy. J Bone Joint Surg Am 35(1): 234-236.
- Saddawi ND, Hoffman BK (1970) Tear of the attachment of a normal medial meniscus of the knee in a four-year-old child: a case report. J Bone Joint Surg Am 52(4): 809-811.
- Schlonsky J, Eyring EJ (1973) Lateral meniscus tears in young children. Clin Orthop Relat Res 97: 1178.
- Bloome DM (2000) Meniscal repair in very young children. Arthroscopy 16(5): 545-54
- Shen HC (2007) Surgical treatment of injury of the anterior cruciate ligament and posterolateral instability in the knee of a 5-year-old: A case report. Am J Sports Med 35(5): 831-83
- Shea KG (202) Bucket-handle meniscal tear in a 5-year-old child. Knee Surg Sports Traumatol Arthrosc 20(11): 2291-229
- Kraus T (2012) Outcome of repaired unstable meniscal tears in children and adolescents. Acta Orthopaedica 83(3): 261-266.
- Fink K (2018) Bucket-handle tear of the medial meniscus in a 2-year-old child. Orthopedics 41(4): e580-e582.
- Weiss CB (1989) Non-operative treatment of meniscal tears. J Bone Joint Surg Am 71(6): 811-8
- Ferrari MB (2019) Meniscus Repair in Children and Adolescents: A Systematic Review of Treatment Approaches, Meniscal Healing, and Outcomes. J Knee Surg 32(6): 490-498.
- Lee BI, Choi HS (2003) Arthroscopic treatment of a symptomatic discoid lateral meniscus in a 26-month-old girl. Arthroscopy 19(10): 1133-113
- Fazio MG, Rpyston EJ, Rooks VJ (2015) An atypical symptomatic discoid lateral meniscus in a toddler. Radiol Case Rep 8(2): 828.
- Ra HJ, Ha JK, Jang SH, Lee DW, Kim JG (2013) Arthroscopic inside-out repair of complete radial tears of the meniscus with a fibrin clot. Knee Surg Sports Traumatol Arthrosc 21(9): 2126-2130.
- Boya H (2004) Clinical and arthroscopic features of meniscal tears and a search for the role of infection in histologically confirmed meniscal mucoid degeneration. Knee Surg Sports Traumatol Arthrosc 12(4): 294-29
- De Lee JC (1985) Complications of arthroscopy and arthroscopic surgery: Results of a national survey. Arthroscopy 1: 214-22

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...