Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2638-6003
Case Report(ISSN: 2638-6003) 
Isolated Scapular Body Fracture in A High School Football Player Volume 5 - Issue 3
Robert Casmus*, Robert Casmus, Kevin Burroughs, Patrick King and Donato Colucci
- Supervisor GWS, Athletic Trainers, Novant Health Forsyth Medical Center, Whitaker Rehabilitation Center, USA
Received:May 13, 2021 Published:May 21, 2021
Corresponding author:Robert Casmus, M.S., LAT, ATC, Supervisor GWS-Athletic Trainers Novant Health Forsyth Medical Center, Whitaker Rehabilitation Center 3333 Silas Creek Parkway, Winston-Salem, NC 27103, USA
DOI: 10.32474/OSMOAJ.2021.05.000211
Abstract
History: A 16-year-old high school football player reported that as he was tackled his posterior shoulder was driven directly into the ground with multiple players landing on top of him. On initial exam there was no obvious deformity or swelling but demonstrated full but painful shoulder ROM for flexion and abduction which diminished as his pain level became intensified. Severe point tenderness noted to the lateral scapular border. Special test for glenohumeral instability were negative as were tests for the AC and sternoclavicular joints. There was no clavicular pain and no paresthesia’s noted. The athlete did note some upper thoracic and rib cage discomfort associated with the trauma. Both vital signs and breath sounds were within normal limits. Initial Care: The athlete was treated with ice and placed in a shoulder sling with instructions to follow-up with the team physician the following day. Differential Diagnosis: Shoulder contusion, rib fracture, glenohumeral sprain, AC sprain, occult clavicular fracture and scapular fracture. Diagnostic Testing: Radiographic images revealed a fracture to the scapula extending from the lateral border through the scapular body to the medial border. A confirmatory CT scan corroborated the initial radiographs for scapular body fracture. Followup Treatment and Care: The athlete continued wearing the sling for the next 4 weeks and was prescribed tramadol and permitted to take ibuprofen. At two weeks post-trauma he was permitted to begin elbow, hand and wrist ROM as pain levels subsided. Followup treatments included hot packs to reduce pain and soreness. Four weeks post-trauma revealed significant fracture site healing and the athlete began progressive upper extremity rehabilitation exercises. At eight weeks he returned to all weight room and football related activities without incident. Uniqueness: The scapula has large muscular coverage and thus fractures are uncommon and account for no more than .5% of all shoulder girdle injuries and no more than 1% of all shoulder girdle fractures. Scapular fractures are commonly associated with high energy forces and blunt trauma impacts such as motor vehicle accidents and falls from various heights. Scapular fractures will often have accompanied injuries to the chest and head. Direct trauma to the scapula leads to fractures of the scapular body, spine or the acromion. Indirect trauma that pulls or levers the arm will result in fractures of the glenoid fossa or scapular neck. Conclusion: Fractures of the scapula body are normally treated nonoperatively with 86% having excellent to good outcomes. 90% of scapular fractures are nondisplaced or moderately displaced and thus treated conservatively. The treatment goal of scapular body fractures is to rest, allow healing to occur and then begin rehabilitation. It is imperative to achieve full active and passive motion as soon as tolerable to decrease adhesion development in the scapulothoracic joint. This case illustrates the appropriate evaluation, conservative treatment and care leading to complete resolution of an isolated scapular body fracture. Complications of scapular fractures if not treated appropriately include altered shoulder girdle dysfunction, rotator cuff dysfunction or impingement and scapulothoracic dyskinesia. The athlete is currently asymptomatic and has returned to all athletic and activities of daily living.
Keywords: Scapula; Fracture Glenohumeral; Trauma
Introduction
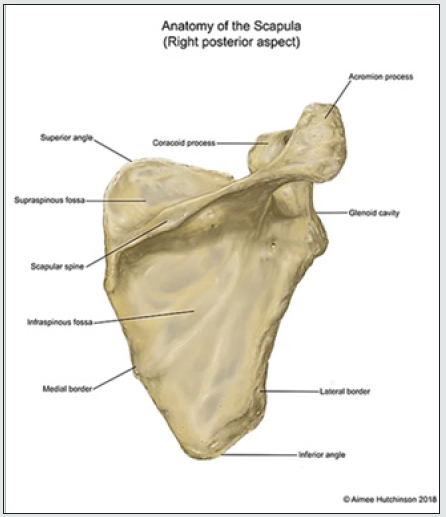
The scapula is a strong, flat and triangular shaped bone that protects the posterior upper chest and is an important component in the function of the shoulder joint serving as the attachment site of multiple muscles.1 It engages in 6 types of motion allowing protraction, retraction, elevation, depression, upward rotation, and downward rotation [1]. The anatomic components of the scapula are detailed in figure 1. Due to its large muscular coverage, scapula fractures are uncommon in general and are rare in sports. They account for no more than 3-5% of all shoulder girdle injuries and no more than 0.4-1% of all fractures.2 Scapular fractures are commonly associated with high energy forces and blunt trauma such as motor vehicle accidents and falls from a height and will often have accompanied injuries to the chest and head.3 Direct trauma to the scapula can lead to fractures of the scapular body, spine or the acromion, while indirect trauma that pulls or levers the arm typically results in more fractures of the glenoid fossa or scapular neck.2 Fatigue fracture of the scapular body is unique to the sporting population and occurs from repetitive trauma to the bone or secondary to muscular contractions causing micro-trauma then frank fracture.3 Scapular body fractures account for about 50% of all scapular fractures, however, most classifications only define simple versus comminuted [4].
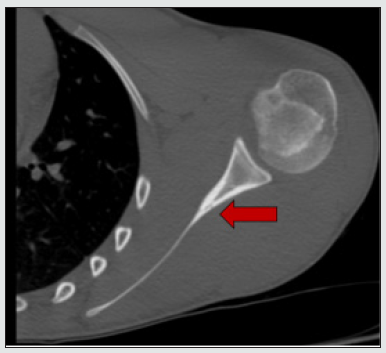
This classification is not practically relevant as does not delineate the anatomic location, nor the recommendations regarding treatment.4 Comorbidity is a concern in trauma secondary to associated injuries including rib fractures, extremity fractures, hemothorax, pneumothorax, pulmonary contusion, head and neck injury and clavicle fractures [5]. Proper care for scapular fractures begins with recognition of the typical injury pattern, then careful examination, and appropriate imaging to properly identify the problem. A comprehensive scapula examination should specifically include direct palpation of the clavicle, acromion, coracoid, the anterior and posterior glenohumeral joint, spine of the scapula, medial and lateral borders of the scapula along with the infraspinatus and supraspinatus fossa (Figure 1). Detection of fractures of the scapula can be difficult due to overlying structures with up to 43% of scapular fractures in trauma patients missed on initial chest radiographs [6]. Dedicated plain radiography using AP, Grashey, axillary, and lateral scapula (Y) views can improve accuracy. These allow diagnosis of scapular and ipsilateral clavicle fractures, as well as acromioclavicular and glenohumeral joint injuries [6]. Computed tomography (CT) is the gold standard for detection and for pre-operative planning for the treatment of complex fractures [6].
There is debate regarding operative versus non-operative management strategies for scapular fractures [7,8]. Controversy stems from the recognition that most extra-articular scapular fractures heal with non-surgical management with little measurable dysfunction, because the shoulder has significant compensatory motion [8]. A study with one-year follow-up of 153 patients presenting with scapular fractures showed 9.8% were treated surgically and only those with glenoid involvement showed improved outcomes [7]. A systematic review showed 100% satisfactory results in patients managed non-operatively and 95.4% in the operative group, with wound complications of 9% in the operative group [9]. Sub-analysis in a systematic review showed excellent or good results in 100% of operative cases, vs 86% in nonoperative, but there were only 2 fractures included in the operative group [10]. The purpose of this report is to present the case of a high school football player who sustained an isolated non-displaced scapular body fracture that was treated non-surgically.
Case Review
A 16-year-old high school football player at the quarterback position reported that as he was tackled his posterior shoulder was driven directly into the ground with multiple players landing on top of him. Initially there was no obvious deformity or swelling and he demonstrated full but painful shoulder range of motion (ROM). However, his flexion and abduction capability diminished as his pain intensified during the sideline evaluation. Severe point tenderness was noted along the lateral scapular border. Special tests for glenohumeral instability were negative as were tests for the AC and sternoclavicular joint pathologies. There was no clavicular pain and no paresthesia’s noted. The athlete did note some upper thoracic and rib cage discomfort. Vital signs and breath sounds were within normal limits. The athlete was withheld from further participation, treated with ice, and placed in a shoulder sling, and given with instructions to follow-up with the team physician the following day.
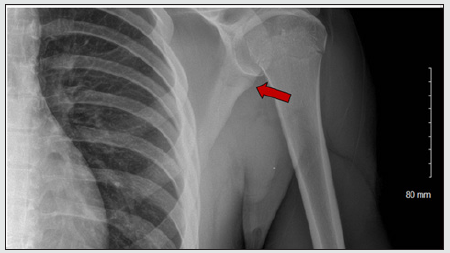
Radiographs the following day revealed a subtle lucency extending from the lateral scapular border transversely to the medial border noted most prominently on the AP (Figure 2). A CT scan was ordered to further delineate the fracture (Figure 3). He was placed in a sling with a body strap for increased immobilization. He was provided with a prescription for ibuprofen and acetaminophen for pain and inflammation with tramadol for breakthrough pain and withheld from athletic activity for the next four weeks. At two weeks he was encouraged to begin elbow, hand and wrist ROM as his pain levels decreased. Additionally, hot packs were used to aid in reducing pain and soreness. Repeat x-rays at four weeks showed evidence of bone callous formation. The athlete was permitted to begin progressive shoulder strengthening exercises as tolerated. Because of the limited resources available at his rural high school, therapeutic interventions were limited. Therapeutic exercises included manual resistance, elastic tubing exercises and dumbbells for muscular strengthening of the deltoid, rotator cuff and trapezius muscles. He also began a progressive football throwing program for distance and intensity as soreness permitted at around 6 weeks post-trauma. At eight weeks he returned to all weight room overhead lifting activities and football participation without incident.
Discussion
The literature shows very few cases of traumatic isolated scapular body fractures in athletes. A systematic review by Neral, et al. found ten reported cases of scapular body fracture sustained during sporting activity with acute trauma responsible for seven of the ten cases documented [3] however, glenoid extension may not be visualized on plain radiographs [11]. Mechanisms varied by activity with forceful maximal internal or external rotation of the upper extremity against resistance being responsible for acute fractures in athletes participating in American football, wrestling, and water skiing, while forceful swinging movements were responsible for fracture in those involved in ice hockey, boxing, and badminton [3]. Additionally, no associated injuries to the remaining shoulder girdle were reported in any reports [3]. The treatment for scapular body fractures is usually conservative with immobilization and relative rest, followed by physical therapy with progressive range-of-motion and strengthening exercises. Fracture healing is determined using serial radiographs. In the review by Neral, et al. involving scapular body fracture in sports activity, there were no complications following conservative management [3]. The criteria for operative treatment of scapular fractures remains controversial and no universal parameters can be found in the existing literature [12]. Markedly displaced scapular body fractures and unstable fractures of the glenoid neck typically undergo open reduction internal fixation for realignment and stabilization and may even include mini-fragment fixation. Both operative and non-operative scapular treatment results in high union rates, high return to functional activity, and minimal complications [12].
Implications for Clinical Practice
Scapula fractures are uncommon in sports with isolated scapular body fractures being very rare. Focused clinical examination and imaging is key to the appropriate diagnosis which guides management decisions.
Substantially displaced fractures of the scapula may alter shoulder girdle function due to malalignment, arthrosis, dysfunction of the rotator cuff, scapulothoracic dyskinesis and impingement type pain [12]. However, the minimally or moderately displaced scapular fracture that does not meet surgical criteria should be managed with a sling for 2-3 weeks until the fracture begins to consolidate, and the pain subsides followed by functional therapy to restore motion and strength [8].
Conclusion
Isolated fractures to the scapular body are rare in sport, however recognition of these injuries is imperative as displaced fractures can alter shoulder girdle function. Typical injury pattern is due to a high energy and blunt force trauma to the scapula. Evaluation must include the assessment for concomitant injury affecting the shoulder and for additional non-shoulder girdle injuries. A conservative approach to non-displaced fractures of the scapula is recommended. Operative management can be considered in cases presenting with significant displacement or an intraarticular component. We outlined a case with conservative management and a progressive rehabilitation program that was successful in aiding a return to sports participation.
All the authors
Casmus, Burroughs, King and Colucci have no conflicts of interest and regarding Declarations.
Conflict of interests
Declare none, In this case report there is no involvement or the use of animal or human subjects.
References
- Cowan PT, Varacallo M (2019) Anatomy, Back, Scapula. StatPearls [Internet] pp.
- Gosens T, Speigner B, Minekus, J (2009) Fracture of the scapular body: Functional outcome after conservative treatment. J Shoulder Elb Surg 18(3): 443-448.
- Neral M, Knapik D, Wetzel R, Salata M, Voos, J (2018) Scapular body fracture in the athlete: A systematic review HSS J 14(3): 328-332.
- Bartonicek J, Klika D, Tucek, M (2018) Classification of scapular fractures. Rozhl Chir 97(2): 67-76.
- Stephens NG, Morgan AS, Corvo P, Bernstein BA (1995) Significance of scapular fracture in the blunt-trauma patient. Ann Emerg Med 26(4): 439-442.
- Berritto D, Pinto A, Russo A, Fabrizio U, Antonella L, et al. (2018) Scapular fractures: a common diagnostic pitfall. Acta Biomed 89(1-S): 102-110.
- Surace P, Boyd A, Vallier, HA (2018) Case series evaluating operative and nonoperative treatment of scapular fractures. Am J Orthop 47(8): 1-11.
- Cole P, Gauger E, Shroder, L (2012) Management of scapular fractures. J Am Acad Orthop Surg 20(3): 130-141.
- Kannan S, Singh HP, Pandey R (2018) A systematic review of management of scapular fractures. Acta Orthop Belg 84: 497-508.
- Zlowodzki M, Bhandari M, Zelle BA, Kregor PJ, Cole PA (2006) Treatment of scapula fractures: Systematic review of 520 fractures in 22 case series. J Orthop Trauma 20(3): 230-233.
- McIntosh J, Akhbari P, Malhas A, Funk L (2019) Scapula fractures in elite soccer and rugby players. Orthopaedic Journal of Sports Medicine 7(12): 2325967119887388.
- Jones CB, Sietsema DL (2011) Analysis of operative versus nonoperative treatment of displaced scapular fractures. Clin Orthop Relat Res 469(12): 3379-3389.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...