Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2638-6003
Review Article(ISSN: 2638-6003) 
Imaging of Muscle Sports Injuries Volume 5 - Issue 3
Sara Muñoz Chiamil*, Edith Miranda Viorklumds and Claudia Astudillo Abarca
- Radiologist, Diagnostic Imaging, Campus Clinica Las Condes, Universidad de Chile, Santiago, Chile
Received:July 2, 2021 Published:July 22, 2021
Corresponding author: Sara Muñoz Chiamil, Radiologist, Diagnostic Imaging, Campus Clinica Las Condes, Universidad de Chile, Santiago, Chile Phone Number: +56996000054 Email: smunoz@clinicalascondes.cl
DOI: 10.32474/OSMOAJ.2021.05.000214
Abstract
Sport activity is common in young and adult population. Muscle injuries affect amateur and professional athletes. It is important the early and accurate diagnosis, for an adequate treatment and follow-up. Imaging are essential in the evaluation of these lesions. It allows determine location, extent, severity and estimate prognosis, as well as the follow-up to determine the return to sport. In this article, microscopic and macroscopic muscle anatomy, types of lesions and their representation in images, on ultrasound (US) and magnetic resonance (MRI) are reviewed. Ultrasound generates images of a greater spatial resolution than MRI. It allows real-time functional and dynamic assessment of muscle and tendons. Different classifications described in the literature are mentioned and a nomenclature and description are proposed, based mainly on the muscle anatomy, the location and quantification of the lesion.
Keywords: Muscle Strain; Sports-Related Muscle Injury; Classification of Muscle Strain
Anatomy
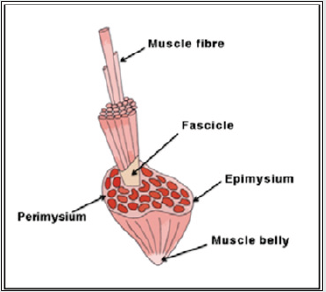
For correct interpretation of the findings on ultrasound and MRI, it is essential to know the microscopic and macroscopic muscle anatomy. The striated muscle, can be considered the largest organ of the body. It represents approximately 25 to 30% of body weight in women and 40 to 50% in men. It consists of two components: muscle fibers and stromal connective tissue. The cell or muscle fiber is the basic structural element. It measures between 10-120 μm. Inside, there are sarcomeres where the actin and myosin filaments are found, responsible for the contraction and elongation of the muscles [1]. The individual muscle fibers are grouped into bundles, the fascicles, which are grouped together to form the muscles. They vary in length and transverse diameter depending on each muscle and tend to be similar in size within the muscle. The connective tissue provides the framework to maintain muscle shape in both relaxed and contracted states. Each muscle fiber is surrounded by a delicate network of connective tissue, the endomysium, which contains small vessels, nerves and proteoglycan matrix for ionic and metabolic exchange. Several muscle fibers form a fascicle that is surrounded by a thicker connective tissue, the perimysium that also provides vascularization, innervation and matrix. Several fascicles form a muscle surrounded by an outer layer of connective tissue, the epimysium [2] (Figure 1).
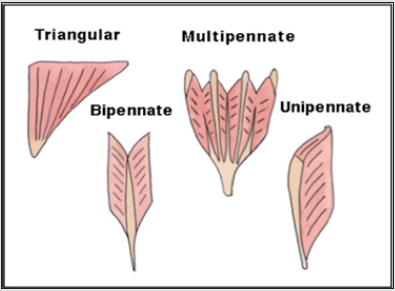
The muscle fibers are inserted into different connective tissue components, including the aponeurosis, the intramuscular aponeurotic septa (central tendons) or directly into the tendon. The internal disposition varies according the orientation of fascicles, which determines the shape and function of the muscle: When fascicles are orientated parallel to the line of traction, a high degree of shortening and high velocity of movement occurs, however, the force is low. Examples are the ribbon-like muscles such as sartorius or rectus abdominis. When the fascicles are orientated obliquely to the line of traction, there is a larger insertion surface, which biomechanically generates greater force with lower range of motion [3]. The oblique orientation of the fascicles is typical of pennate muscles (also called a penniform muscle, from Latin penna: pen and forma: form). There are several types of pennate muscles (Figure 2).
In bipennate muscles the fascicles converge in a single central tendon, whereas the multipennate have more than one tendon. The fascicles can also adopt a spiral arrangement in muscles that curve or have a spiral path as supinator or pectoralis major. On the other hand, the muscles can have a single belly or can be formed by the union of two or three heads as biceps brachii or triceps, which join in a distal tendon [4].
From the histological view there are two types of muscle fibers:
a) Type I or slow contraction (slow-twitch): they have a
smaller diameter, more mitochondria, myoglobin and capillaries
per fiber, more suitable for repetitive contraction, with greater
resistance to fatigue.
b) Type II or rapid contraction (fast-twitch): larger, with
fewer blood vessels and myoglobin, more suitable for fast phasic
forces, better adapted for intense activity of short duration and
greater tension [5].
The active tension produced by a muscle is proportional to the
type of fibers it contains, then, muscles with a high proportion of
type II fibers are capable of generating greater force. Low intensity
exercises selectively involve type I fibers, while type II fibers are
recruited when the intensity of the exercise increases. Sprinters, for
example, have predominance of type II fibers, while in marathon
runners type I predominate. It is not clear if this predominance is
genetically determined or it is a response to training. Muscle strains
are more frequent in muscles with predominance of type II fibers
[6,7]. Each muscle is made up of mixture of both types of fibers. In
some, type II predominates (example: medial calf) and in others
type I (example: soleus). During muscle contraction the force is
transmitted from the tendon to the skeleton, generating three types
of effect [2,3].
a. Isometric contraction: the muscle contracts, and does not
change its length.
b. Isotonic contraction: the muscle contracts and shortens.
c. Eccentric contraction: the muscle contracts and lengthens.
A muscle strain occurs when tension exceeds the strength
of the weakest structural element. It has been experimentally
demonstrated that muscle stretched to failure, always ruptures near
the distal myotendinous junction [8]. This anatomical introduction is
relevant, because muscle strains occur predominantly in biarticular
muscles (muscles that cross more than one joint), of eccentric action
and high proportion of type II fibers. They affect the anatomical or
functional transition zones, corresponding to the insertion of the
fascicles in the fascia, aponeuroses or tendons, whether central or
distal, since they generate the highest concentration of intrinsic
forces, so they are the points of greatest biomechanical weakness [9]. Movement is the result of muscle contraction, and a muscle
group performs the predominant function. Other muscles, called
synergists, act in the same direction of movement, supporting
the main group. Antagonists are those which oppose the action2.
For the correct contraction of one muscle another must relax
allowing the normal movement. If the main muscle contracts
disproportionately in relation to its antagonist, it will not resist the
traction and will rupture during the contraction. Thus, an optimal
training that corrects and improves muscle coordination, which
includes strength and resistance work, is essential to reduce the
incidence of these injuries.
Muscle Imaging
Plain radiograph
X-ray has a limited role because the muscles do not have a good representation. It may be useful to detect calcifications or when ossifying myositis is suspected in the evolution of a muscle lesion. Computed tomography is not indicated for evaluation of muscle strains. It can be useful to differentiate muscle from calcification in contact with cortical bone. US and MRI are the examinations of choice [10-13]. the decision which to use depends on the experience of the radiologist and the availability of appropriate equipment. In our country, US is the best exploration technique most of cases.
MRI and US
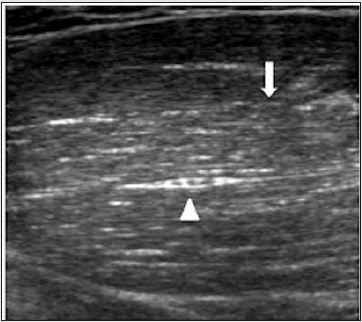
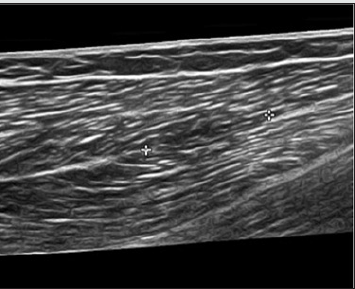
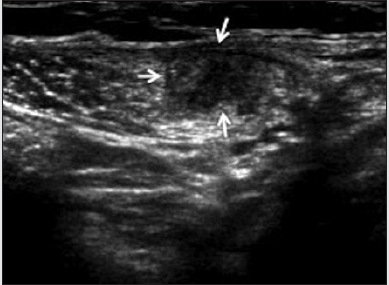
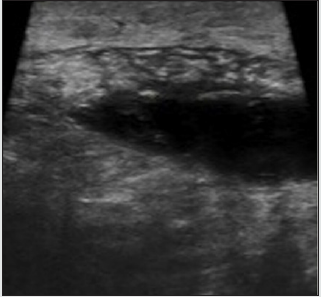
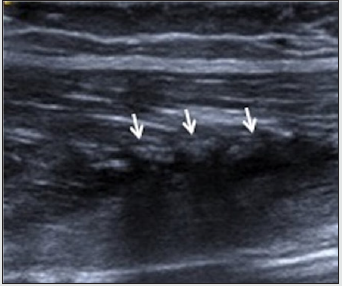
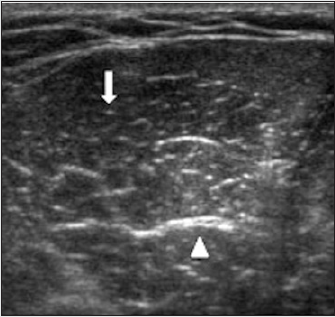
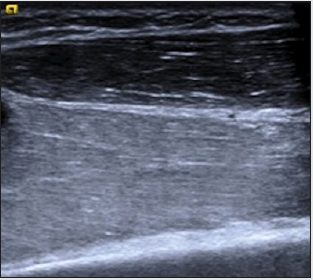
MRI is reproducible, has multiplanar capacity, high tissue contrast, high sensitivity, lower specificity, with the advantage of exploring large areas in a single image. It is more expensive and less available than US. In subtle or extensive lesions, MRI could be better particularly in the high-performance athlete, affording simultaneous evaluation of soft tissues and osseous structures [14]. MRI studies in muscle injuries should include enhanced sequences in T1, T2, Proton density with fat saturation (PD FS) and STIR. Axial, coronal and sagittal planes should be carried out. We recommend the study covering the entire extension of the affected muscle group.US is a real-time examination [14], dynamic and eventually comparative. It is less expensive than MRI, with greater availability in our country. It can serve as guidance for interventional procedures, (platelet-rich plasma, collection drainage). The limitations of US are related to the small field of view, the need for an expert operator, is less sensitive for low-grade muscle injuries and that it is a nonreproducible examination14. High- frequency linear array probes 7-10 MHz are required to adequately image muscle. In voluminous patients or with muscular hypertrophy, it may be necessary to use transducers of less frequency. The examination should be done on the short and long axis of each muscle [3,4]. The aspect of a muscle consists of a hypoechoic background that reflects muscle fascicles and delimited linear hyperechoic bands that represent fibrofatty septa, the perimysium. The intramuscular aponeuroses and tendons appear as hyperechoic bands, which are better visualized on the short axis of the muscle3 4. The distribution between these components explain the proportion between muscle fascicles and connective tissue. US can recognize the muscles architecture and hence the importance of knowing the anatomy of the muscle studied. In the transverse plane, short axis, the ultrasound appearance of the muscle has been described as a “starry night” with the visualization of hyperechoic dots (perimysium) within a hypoechoic background (muscle fascicles) (Figures 6 a, b). US of the normal muscle: Perimysium (arrow). Central tendon (arrow head). a) cross section. b) longitudinal. The angle between the ultrasound beam and the muscle is fundamental. An angle that deviates from the perpendicular causes the muscle to look hypo or hyperechogenic as an artifact (Anisotropy) [3]. The ultrasound semiology of muscle injuries is limited, which makes the clinical correlation indispensable for a correct interpretation of the findings.
Figure 3a: US of the normal muscle: Perimysium (arrow). Central tendon (arrow head). a) cross section. b) longitudinal.
In most of all the injuries we will see one or more of the following signs:
1) Diffuse increase or decrease in echogenicity: depending on the
moment of exploration in relation to the traumatic event, it can
explain microscopic fibrillar lesion, edema, recent bleeding or
inflammatory process.
2) Distortion of the architecture of fascicular pattern: corresponds
to the distortion or loss of the pennate appearance.
3) Muscle defect: it explains macroscopic disruption of fascicles.
It is an avulsion and retraction of muscle fibers in relation
to the tendon or aponeuroses where it is inserted, whether
central intramuscular, peripheral or distal.
4) Fluid collection: which correspond to the hematoma.
Classification
According to their mechanism they have been classified in:
a) Intrinsic or indirect: not caused by an external force.
b) Extrinsic or direct: the cause is an external force.
Intrinsic Or Indirect Injuries
Muscle strain
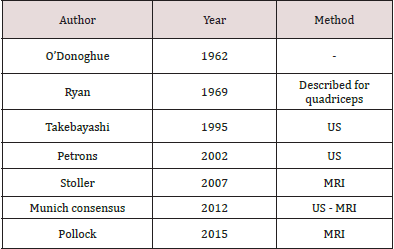
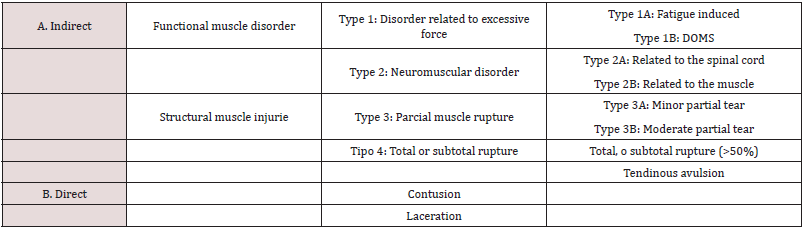
They correspond to a spectrum of lesions ranging from the minimal microscopic fibrillar lesion, (a macroscopic defect is not identified), to the complete rupture of a muscle belly. They occur because of excessive or simultaneous stretching caused by a sudden eccentric contraction. There is structural damage of muscle tissue, breakage of fibers and fascicles. The most frequent mechanism is a sudden elongation at the time of eccentric contraction, which is common in sports involving acceleration deceleration or sudden changes in direction. Over the years different classifications of muscle injuries have been described in the literature, both for US and MRI, most using degrees from 0 to 4, depending on the author. None have been universally accepted. Following are mentioned the ones most used [9,15] (Table 1). In 2012, a meeting of international experts in sports medicine was held to develop practical and scientific definitions of muscle injuries, as well as a new classification system. It is known as the Munich Consensus. (Level of evidence V. Expert opinion), whose suggestion is summarized in (Table 2). This classification includes neuromuscular disorders (type 2), which move away from the interest of this article. In our experience, no classification is fully able to answer the information necessary for the clinical management of sports-related muscle injuries. In our opinion, an exhaustive description of the alteration and its location is more useful than a classification in degrees. Following are reviewed the imaging aspects of the indirect muscle injuries type 1, 3, 4 and of direct lesions (in Munich classification). Most of the of patients seen in radiological practice, whether amateur or professional athletes, correspond to type 3 injuries [16-20].
To correctly interpret the images of an injury it is necessary to
remember that muscle fibers are microscopic, so a “fibrillar” lesion
is not seen as a defect or gap in the muscle tissue.
The fibers (macroscopic) are organized into fascicles measuring
between 2 and 5 mm, which can be viewed using imaging. So,
we call “Fibrillary” the lesion which involves a smaller diameter
than a fascicle, a minor partial strain (“fibrillary strain”3A) and
“Fascicular” when more than one fascicle is involved, a moderate
partial strain (“fascicular strain” 3B). US and MRI do not always
accurately determine the size of the defect and may overestimate
the damage due to edema on US and the signal intensity on MRI
[10]. Sometimes we find patients with positive clinical examination,
with negative imaging findings. In these cases, the patient has
suffered a “contracture”, terminology that the Munich consensus
does not recommend. It would correspond to a functional disorder
related to excessive force induced by fatigue or type 1A injury in
the Munich consensus. There is no structural muscle damage [21].
There is pain and painful palpation of a large area, including a
muscle group. “Fibrillary” strain (or 3A minor partial in the Munich
consensus) Corresponds to the minimum fibrillary lesion. It
produces slight discomfort at the time of the injury. There is pain to
the passive muscle elongation and focal pain on palpation. There is
not defect in the muscle. It produces distortion of the architecture,
edema and/or hemorrhage in the area of the lesion, in areas of
anatomical transition. It must be considered that, in small lesions,
the ultrasound manifestations may take hours to appear, so that
US study should not be performed immediately after the traumatic
event, since it may be negative.
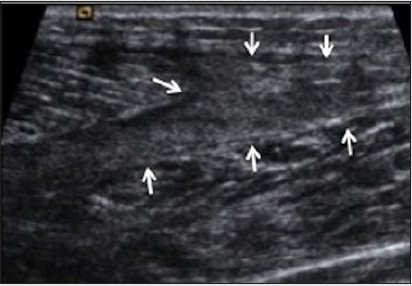
In cases of positive symptoms and negative US study, we
recommend reevaluating after 24 hours. From an ultrasound view,
there may be a focal increase or decrease in echogenicity, associated
or not with distortion of the architecture and the normal fascicular
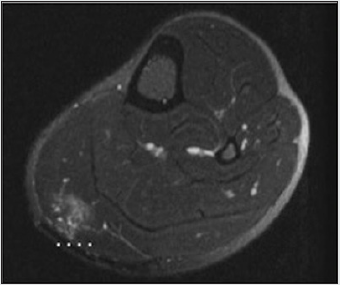
pattern (Figure 4 a,b,c). On MRI the fibrillar lesion is observed as
high signal intensity without macroscopic defect (Figure 5 a,b). Our
recommendation for both methods is to measure the dimensions of
the alteration on the short and long axis. These lesions usually heal
ad integrum, without fibrous scar formation. Partial “fascicular”
strain (3B moderate in the Munich consensus) [22-24] It
corresponds to a partial lesion with involvement of muscle fascicles
that are visible macroscopically. It produces intense pain at the
time of injury, local pain on palpation and passive elongation. The
athlete must stop the activity. Local contractility is lost. Fascicles
and adjacent connective tissue (endomysium and perimysium)
are affected, which helps to differentiate them from the fibrillar
lesion. Fiber disruption, probable shrinkage and hematoma of
these will be seen. Considering that the blood flow is increased
when the muscle is active, these lesions quickly produce bleeding.
This hemorrhage has different presentations, depending on the
integrity of the fascia. If it is undamaged, the bruise is confined
to the muscle. If the fascia is broken, the hematoma accumulates
in the intermuscular or subcutaneous space. This is the case of
patients with ecchymosis. The hematoma is the hallmark of the
muscle rupture and its appearance on US depends on the location
of the injury and the time elapsed. In acute or recent hemorrhage,
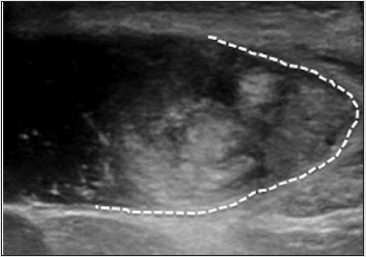
it is usually echogenic (Figure 6a) Within a few hours it behaves
as a hypoechogenic and homogeneous collection (Figure 6b), an
appearance that remains for a variable time depending on its size
[25]. In more chronic stage, the elements of the blood, cells, serum,
fibrin etc., can be separated and give as a result a fluid-fluid level.
After a few days, the collection becomes uniform, anechoic, which
is called a “serosal” stage hematoma (Figure 6c). To estimate the
size of the lesion, which can sometimes be variable and difficult,
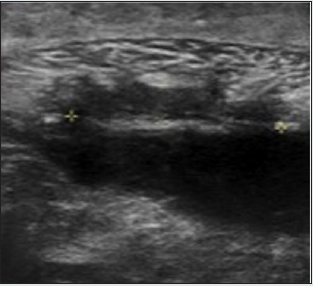
the following is suggested: If the strain occurs at the central
myotendinous or myoaponeurotic junction, we recommend linear
measurement of the hematoma on the short and long axis of the
muscle (Figure 7a and 7b). Their dimensions, in general, coincide
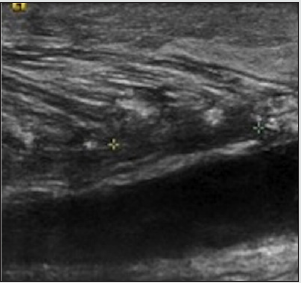
with the magnitude of the damage. If the strain occurs at the junction
of the fibers to the fascia (peripheral myofascial), without rupture
of the fascia, we recommend curve measurement on the short axis
at the periphery of the muscle (Figure 8a) and measurement on the
long axis, also at the periphery (Figure 8b). Usually the dimensions
of the hematoma coincide with the extent of the lesion. If the strain
is located peripheral myofascial with rupture of the muscle fascia,
the hematoma is not contained within the muscle and accumulates
in the intermuscular space. In this situation, it is more difficult to
estimate the amount of damage, since the size of the hematoma
does not necessarily coincide with the extent of the lesion.
Figure 4c: Fibrillary lesion on US: a) Focal increase of echogenicity with measurement on the short axis (cross). b) Reduced focal echogenicity on long axis (cross). c) Distortion of the muscle architecture.
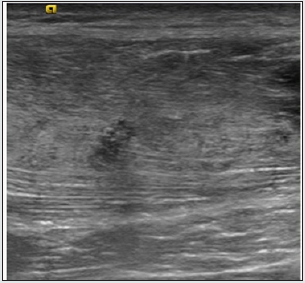
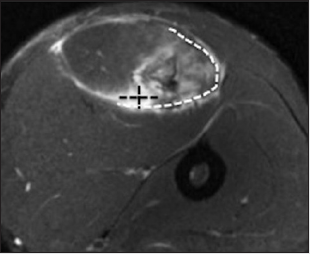
Figure 5b: Fibrillary lesion on MRI. a) Axial PD FS with measurement on short axis (dashed line). b) Coronal PD FS with measurement on long axis.
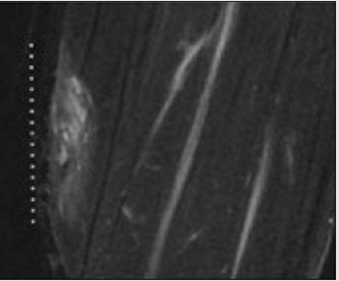
Figure 6c: Phases of the hematoma on US (arrows). a) Echogenic, b) Heterogeneous hypoechogenic, c) Anechogenic or serous.
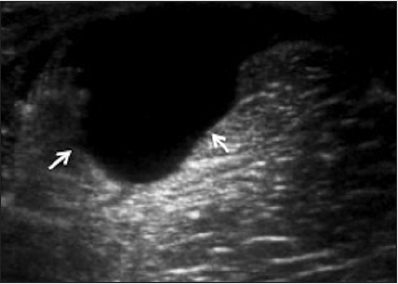
Figure 7a: Phases of the hematoma on US (arrows). a) Echogenic, b) Heterogeneous hypoechogenic, c) Anechogenic or serous.
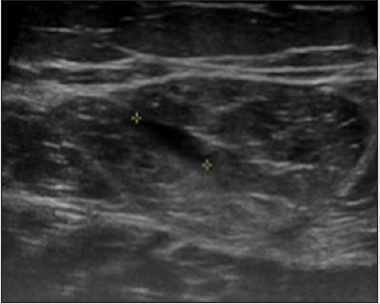
Figure 7b: Myotendinous or central myoaponeurotic fascicular strain with measurement (cross) on US. a) Short axis, b) Long axis
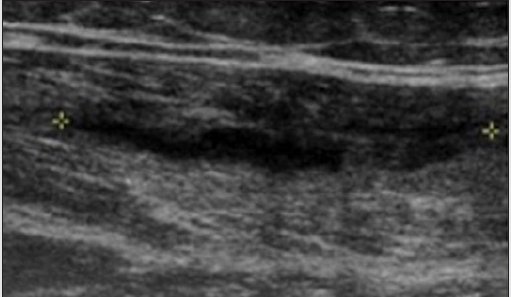
Figure 8b: Fascicular strain in myofascial location, without rupture of the fascia on US. a) Short axis, distortion and disruption of fibers, partial defects and retraction, with curve measurement of the circumferential extension affecting the muscle (dotted line). b) Long axis, longitudinal measurement (cross) of muscle defect with hematoma
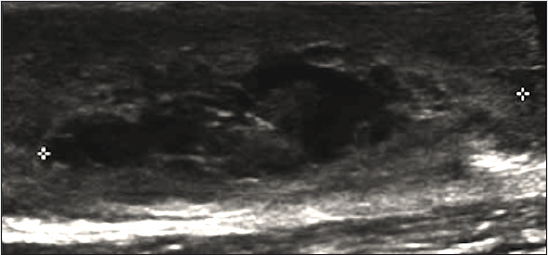
Figure 9d: Fascicular strain in the myofascial location, with rupture of the fascia and intermuscular hematoma on US. a) Short axis of the strain with measurement (cross), b) Long axis of the strain with measurement (cross), c) Short axis of the hematoma, d) Long axis of the hematoma in extended vision
We recommend the estimation of the strain on the short and long axis, and the measurement of the intermuscular hematoma separately (Figure 9 a,b,c,d). On US and MRI, the same criteria for the quantification of the lesions are used. The disadvantage of MRI is that sometimes it can be difficult to differentiate the edema from the hematoma, since sometimes both can appear similar (Figure 10). Total strain - Subtotal (or type 4 in Munich consensus) Complete rupture of a muscle belly is rare. Subtotal strains, which involve more than 50% and avulsions are more frequent. Clinical experience has shown that the healing time of subtotal and total ruptures is similar. Avulsions are included in this category, since biomechanically they correspond to a complete rupture of the insertion origin. The most frequent sites are the proximal femoral rectus insertion, hamstring, long adductor and distal insertion of the semitendinosus.
Figure 10: Fascicular strain in myofascial location, with edema but without fascial rupture on axial PD FS MRI. Curved measurement of the circumferential extension of affected muscle (white lines). Measurement of muscle defect with hematoma (black lines).
The patient presents with severe pain and loss of function, with a palpable defect and ecchymosis. On US, the examination can be difficult due to the limited field of view. There is a defect that involves all the thickness of the muscle and fluid collection interposed between the ends of the rupture. On MRI it is relatively easier to assess the size of the defect and the hematoma.
Delay Onset Muscle Soreness (Type 1b In Munich CONSENSUS)
DOMS: Acronym for Delayed Onset Muscle Soreness . This was described at the beginning of the century and its initial definition has not changed significantly. Its etiopathogenesis has not been clarified. It is estimated that virtually every adult person has once experienced late onset muscle pain. It occurs in beginner athletes or athletes who perform eccentric activities. The symptoms consist of the appearance of muscle pain hours after strenuous or unaccustomed exercise, which lasts 5 to 7 days and which is self-limiting. The peak is 2 or 3 days after the exercise. There is characteristic acute inflammatory pain, due to the local release of inflammatory mediators. On US, an increase in the volume of the affected muscle is observed, associated with a diffuse increase in echogenicity due to edema (Figure 11 a,b), which can also be seen on MRI.
Figure 11a: Fascicular strain in myofascial location, with edema but without fascial rupture on axial PD FS MRI. Curved measurement of the circumferential extension of affected muscle (white lines). Measurement of muscle defect with hematoma (black lines).
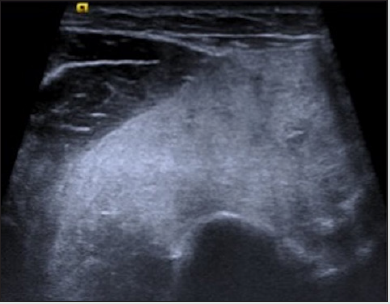
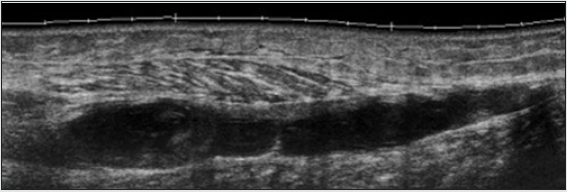
Figure 11b: DOMS on US. Muscle edema with increase in echogenicity and volume of the affected muscle, without alteration of the muscle architecture. a) Short axis, b) Long axis
Extrinsic Or Direct Injuries
Contusion - laceration (type b in munich consensus) The muscle contusion corresponds to a compression of the muscle by direct trauma. It results from the collision of the muscle mass against a hard surface and the bone. These are frequent in contact sports such as rugby, soccer (football), etc. Its severity depends on the contact force and the contraction situation of the muscle at the time of the trauma. It usually affects muscles in a deep location, adjacent to the bone plane, such as the vastus intermedius in the thigh. It causes bleeding that precociously produces a diffuse hyperechogenic appearance of the area, transforming over time into a mixed hypoechoic area with progressive better delimitation. The normal fibrillar pattern is lost. It can affect more than one muscle. On both US and MRI there is edema, hemorrhage, defect, architectural distortion and fluid collection - hematoma. The laceration results from penetrating injuries and is seen in sports such as water skiing, motorcycling, etc. It is accompanied by an open wound in the skin and more frequently affects superficial muscles. Therefore, from our experience and considering the classifications described in literature, we propose the exhaustive description of the muscle injurie, based on the muscle anatomy, the location, size and the type of lesion (fibrillar, fascicular, subtotal or total strain), instead of determine lesion degrees.
Evolution
Muscle injuries are usually self-limiting. To make a correct
interpretation of the findings in images, it is important that in
addition to the anatomy, we know the physiopathology of these
lesions. In an acute injury there is fiber destruction followed by
necrosis, local inflammation and hematoma formation. Then the
necrotic area is invaded by small blood vessels, mononuclear cells,
macrophages and T lymphocytes that infiltrate locally. These release
cytokines and growth factors. The lesions that affect the soft tissues
of the musculoskeletal system are resolved by a mechanism mainly
of repair, unlike bone lesions that heal by regeneration. The healing
model of muscle injuries includes 3 well-differentiated phases,
lasting approximately 3 weeks. Destruction phase: In the first days
there is degeneration and active inflammation. In this period the
rupture of the muscle tissue and the necrosis of the myofibrils takes
place with the formation of a hematoma between the broken fibers.
In addition, an inflammatory cell reaction occurs. Repair phase: the
necrotic tissue reabsorption occurs, the regeneration of myofibrils
and the production of an area of connective tissue and new
capillaries. Regeneration usually begins between 7 and 10 days.
The peak of regeneration is in the second week and decreases in the
third and fourth. Remodeling phase: The newly formed myofibrils
are matured; the reorganization of the tissue will allow the recovery
the contractile capacity of the new muscle. The formation of a scar
(fibrosis) begins between the second and third week, and the scar
increases in size over time. The 3 phases overlap in time.
Part of the role of imaging is to follow up the evolution of
strains and detect eventual complications5, especially with US.
In the fibrillar strains, we look for the resolution of the edema or
hemorrhage by comparing the dimensions of the affected area.
These injuries usually repair ad integrum. In fascicular strains,
the hematoma changes progressively. The cavity is “filled” with
hypoechoic tissue from the periphery to the center. The information
relevant to the clinician is the presence of residual fluid hematoma
and edema of muscle fibers, and in later stages the appearance
of a scar. In total strains, subtotals and tendon avulsions we also
evaluate the regression of the hematoma, which usually takes
longer than in the previous lesions, these lesions being the ones
with the slowest recovery and the worst prognosis.
Complications
Muscle scar
All macroscopic muscle injuries heal with fibrosis to a greater or lesser degree. When the lesion is not treated properly, the result is a fibrous-retractable scar that constitutes a complication, determining new anatomical transition zones that predispose to new injuries. When the treatment is early an adequate, a greater degree of regeneration can be achieved versus scarring and the result will be less fibrosis. Both on US and MRI, a stellate, retractable image can be observed, associated with a decrease in volume and muscle atrophy in the fibers adjacent to the scar (Figure 12 a, b).
Muscle hernia
It constitutes a possible complication of strains that have affected the fascia. It is defined as the protrusion of a part of the muscle through a fascial defect. Most are asymptomatic, although they can sometimes cause pain or edema in the area of the hernia. The best imaging tool is US at rest and dynamic, where it is possible to demonstrate the size of the defect of the fascia and the portion of muscle through it.
Others
Other complications that may occur are chronic compartmental syndrome and calcifications-myositis ossificans.
Conclusion
Muscle injuries in sports are very frequent. The role of imaging is fundamental in the diagnosis and follow-up. US and MRI are the examinations of choice , the decision of which to use should consider the experience of the radiologist and the availability of appropriate equipment. The radiologist must know the individual anatomy of each muscle and the clinical background for the adequate interpretation of the imaging findings. There are multiple classifications of sports-related muscle injuries, the majority in degrees, based mainly on MRI. In this article we propose a nomenclature and description, based mainly on the muscle anatomy, the location and the type of the lesion, useful for both US criteria and improve the management of these injuries.
References
- Exeter D, Connell DA (2010) Skeletal muscle: functional anatomy and pathophysiology. Semin Musculoskelet Radiol 14(2):97-105.
- Huard J, Li Y, Fu FH (2002) Muscle injuries and repair: current trends in research. J Bone Joint Surg Am 84(5):822-32.
- Zamorani MP, Valle M (2007) Muscle and Tendon. In: Bianchi S, Martinoli C. Ultrasound of the Musculoskeletal System. 1st Germany. Springer-Verlag Berlin Heidelberg p: 45-96.
- Lee J, Healy J (2011) Sonography of muscle injury. In: Allan P, Baxter G, Weston M. Clinical Ultrasound, (3rd), United Kingdom. Elsevier pp: 1137-1157.
- El Khoury GY, Brandser EA, Kathol MH, Tearse DS, Callaghan JJ (1996) Imaging of muscle injuries. Skeletal Radiol 25(1): 3-11.
- Muñoz S (2002) Lesiones musculares deportivas: Diagnóstico por imá Rev Chil Radiol 8: 127-132.
- Douis H, Gillett M, James SL (2011) Imaging in the diagnosis, prognostication, and management of lower limb muscle injury. Semin Musculoskelet Radiol 15(1): 27-41.
- Garrett WE Jr, Safran MR, Seaber AV, Glisson RR, Ribbeck BM (1987) Biomechanical comparison of stimulated and nonstimulated skeletal muscle pulled to failure. Am J Sports Med 15(5): 448-454.
- Mueller-Wohlfahrt HW, Haensel L, Mithoefer K, Ekstrand J, English B, et al. (2013) Terminology and classification of muscle injuries in sport: the Munich consensus statement. Br J Sports Med 47(6): 342-350.
- Pedret C, Balius R (2015) Lesiones musculares en el deporte. Actualización de un artículo del Dr. Cabot, publicado en Apuntes de Medicina deportiva en 1965. Apunts Med Esport 50: 111-120.
- Lee JC, Healy J (2004) Sonography of lower limb muscle injury. AJR Am J Roentgenol 182(2): 341-351.
- Shelly MJ, Hodnett PA, MacMahon PJ, Moynagh MR, Kavanagh EC, et al. (2009) MR imaging of muscle injury. Magn Reson Imaging Clin N Am 17(4): 757-773.
- Fleckenstein JL, Weatherall PT, Parkey RW, Payne JA, Peshock RM (1989) Sports-related muscle injuries: evaluation with MR imaging. Radiology 172(3): 793-798.
- Crema MD, Yamada AF, Guermazi A, Roemer FW, Skaf AY (2015) Imaging techniques for muscle injury in sports medicine and clinical relevance. Curr Rev Musculoskelet Med 8(2): 154-161.
- Pollock N, James SL, Lee JC, Chakraverty R (2014) British athletics muscle injury classification: a new grading system. Br J Sports Med 48(18): 1347-1351.
- Evans GF, Haller RG, Wyrick PS, Parkey RW, Fleckenstein JL (1998) Submaximal delayed-onset muscle soreness: correlations between MR imaging findings and clinical measures. Radiology 208(3): 815-820.
- Järvinen TA, Järvinen TL, Kääriäinen M, Kalimo H, Järvinen M (2005) Muscle injuries: biology and treatment. Am J Sports Med 33(5): 745-764.
- Järvinen TA, Järvinen M, Kalimo H (2014) Regeneration of injured skeletal muscle after the injury. Muscles Ligaments Tendons J 3(4): 337-345.
- Woodhouse JB, McNally EG (2011) Ultrasound of skeletal muscle injury: an update. Semin Ultrasound CT MR 32(2): 91-100.
- Beggs I (2003) Sonography of muscle hernias. AJR Am J Roentgenol 180(2): 395-399.
- Boutin RD, Fritz RC, Steinbach LS (2002) Imaging of sports-related muscle injuries. Radiol Clin North Am 40(2): 333-362.
- Counsel P, Breidahl W (2010) Muscle injuries of the lower leg. Semin Musculoskelet Radiol 14(2): 162-175.
- Koh ES, McNally EG (2007) Ultrasound of skeletal muscle injury. Semin Musculoskelet Radiol 11(2): 162-173.
- Flores DV, Mejía Gómez C, Estrada Castrillón M, Smitaman E, Pathria MN (2018) MR Imaging of Muscle Trauma: Anatomy, Biomechanics, Pathophysiology, and Imaging Appearance. Radiographics 38(1): 124-148.
- Wangensteen A, Guermazi A, Tol JL, Roemer FW, Hamilton B, et al. (2018) New MRI muscle classification systems and associations with return to sport after acute hamstring injuries: a prospective study. Eur Radiol 28(8): 3532-3541.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...