Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2638-6003
Case Report(ISSN: 2638-6003) 
Health Improvement Plan to Increase Physical Activity in Children from ethnic minority and lower socio-economic class (SEC) in London Borough of Ealing, UK- A theorybased solution Volume 5 - Issue 4
Vidhi Sadana*
- Rheumatology Unit, Central Middlesex Hospital, London, UK
Received:October 25, 2021 Published: November 8, 2021
Corresponding author: Rheumatology Unit, Central Middlesex Hospital, London, UK.
DOI: 10.32474/OSMOAJ.2021.05.000216
Abstract
Low levels of physical activity and high levels of sedentary behaviour London Borough of Ealing are primary drivers of high
levels of preventable chronic conditions. In the last two decades, the government has invested heavily to increase PA levels. However,
these initiatives have not reached target groups such as low income and ethnic minorities. Children from this group face number
of social, environmental and cultural barriers to engaging in PA. The article presents a health improvement intervention plan to
improve PA of children aged 8-12 years from ethnic minorities and lower SEC living in the London Borough of Ealing using Socioecological
Theory.
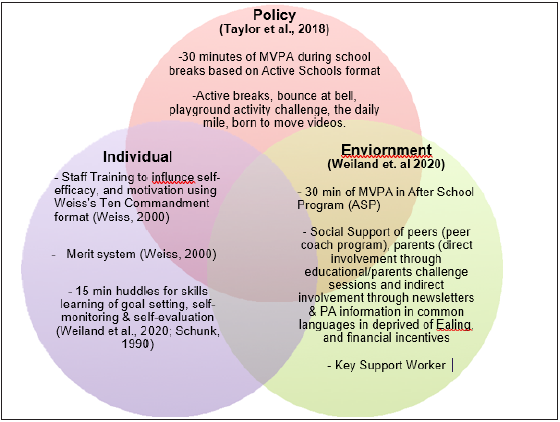
Theory-Based Solution: Let’s Get Fit Ealing is underpinned in a socio-ecological approach focusing on multi-level factors
that can provide a comprehensive solution to increased PA in ethnic minorities children from deprived parts of Ealing. It is a sixweek
school-based intervention to influence children’s behaviour to engage in national guidelines of daily 60 minutes of MVPA.
Components are 30 minutes policy of MVPA during otherwise sedentary times in school hours such as recess.
Discussion: Low SEC ethnic children who have limited access to PA facilities and environmental factors outside of school
deters them from engaging in PA. Additionally, low SEC in London finds neighbourhood constraints as one barrier for children to
engage in PA. However, the solution uses school and its after school component as a setting for the delivery of the health-promoting
intervention for children as it has an advantage due to its universal attendance, a significant amount of time spent in school and
access to PA facilities and PE staff. The additional component includes providing information to parents about national guidelines
and health benefits about PA to support their children in the most common languages used in Ealing.
Conclusions: The socio-ecological framework offers a comprehensive approach to increasing levels of PA in children from ethnic
and low SEC backgrounds of Ealing because it addresses not only the individual characteristics but also social and environmental
influences. With many inactive children residing in this borough and high levels of preventable chronic conditions such as childhood
obesity, the solution presents an excellent opportunity to increase PA in children based on previous successful school-based research.
Introduction
Low levels of physical activity, and high levels of sedentary
behavior London Borough of Ealing are primary drivers of high
levels of preventable chronic conditions (London Borough of
Ealing, 2018) [1]. In the last two decades, government has invested
heavily to increase PA levels. However, these initiatives have not
reached to target groups such as low income and ethnic minorities
(Gov.uk, 2019) [2]. Children from this group face number of social,
environmental and cultural barriers to engage in PA [3]. The article
presents a health improvement intervention plan to improve
PA of children aged 8-12 years from ethnic minorities and lower
SEC living in the London Borough of Ealing using Socio-ecological
Theory (Bronfenbrenner, 1981) [4].
In 2015, only 22% of children aged 5-15 met the national
guidelines of engaging in sixty minutes of moderate to vigorous
activity (MVPA) (NHS England, 2016) [5]. Moreover, only 42% of
the children from low SEC children engaged in PA compared to 54%
of children from high SEC (England, 2019) [6] and highest level
of inactivity was found in Black, Asians and other ethnic minority
children (England, 2019) [6]. In London Borough of Ealing, similar
social and ethnic gradient was found in PA adherence to national guidelines with further low engagement in PA (London Borough of
Ealing, 2018) [1].
Physical inactivity is fourth leading cause for global mortality
and a risk factor for over 20 chronic conditions, including obesity,
coronary heart disease, type 2 diabetes, stroke, cancer and mental
health problems (London Borough of Ealing, 2018) [1]. There is a
rising trend of childhood obesity (20.7 per cent in 2009/10 to 23.3
per cent in 2014/15), a consequence of physical inactivity, in the
deprived parts of Ealing with high proportion of Black, Asian and
other ethnic minorities (London Borough of Ealing, 2018) [1]. To
address lack of PA and its resulting consequences, current Ealing
council’s strategy is to encourage and provide opportunities to
those identified as not participating in enough exercise (London
Borough of Ealing, 2018) [1].
Theory Based Solution
A cross-sectional analysis of Millennium study found clear socioeconomic and ethnic differences in children’s PA levels (Love et al., 2019) [7]. Factors influencing low levels of PA were access to inadequate PA opportunities, cost barriers, parental perceptions of ethnic minority children about PA and lack of home and family support to engage in PA (Love et al., 2019) [7]. This implies that apart from individual characteristics of children, numerous social and environmental factors contribute towards children engaging in PA (Spence and Lee, 2003) [8]. Deprived parts of Ealing chosen for this report have high levels of income deprivation affecting children (Ealing Council, 2004) [9], low levels of parent educationattainment levels and also constitute a large proportion of Asian, Black and other ethnic minorities (London Borough of Ealing, 2018) [1]. This area also has poor access to facilities and above London average crime rates and violence (Ealing Council, 2004) [9]. A socio-ecological approach focusing on multi-level factors can provide a comprehensive solution to increased PA in ethnic minorities children from deprived parts of Ealing. Numerous literature reviews have supported this approach to intervention design aimed at increasing PA levels in children from this group [10,11,12,13,14,15]. However, multi-level interventions that involve individual, environment and policy can sometimes be difficult to put in practice in ‘real-life’ settings due to poor implementation [16]. The article discusses dimensions of RE-AIM model for program planning, implementation and evaluation in order to offer mitigating strategies to potential challenges that may arise in “noncontrolled” settings [17,18,19]. This article outlines a school-based health promoting intervention “Lets Get Fit Ealing” to increase PA targeted at ethnic minority children from the deprived area of Ealing using socio-ecological framework.
Lets Get Fit Ealing Health Promoting Intervention:
It is a six weeks school-based intervention with the aim to influence children’s behaviour to engage in national guidelines of daily 60 minutes of MVPA. Components are 30 minutes policy of MVPA during otherwise sedentary times in school hours such as recess [20] and 30 minutes of structured PA in an After School Program (ASP) [15].
Discussion
School as a setting for health promoting intervention for
children has an advantage due to its universal attendance, large
amount of time spent in school and access to PA facilities and PE
staff. This may be especially helpful for low SEC ethnic children who
have limited access to PA facilities [21] and environmental factors
outside of school that deters them from engaging in PA [22,23].
School leaders can help to shape PA culture and integrate PA
throughout the school day as in case of Health Promoting Schools
(HPS) using Active schools program [8-24]. It used policy guidelines
that gave flexibility to schools to adhere to duration and frequency
of program components according to individual school’s timetables
[14]. Although, despite program’s flexibility in implementation,
standardised definitions and measurements could help in process
evaluations and development of school–based techniques [14].
However, only modest success was found to promote engagement
in PA when delivered only during school times [25,26]. This could
be due to academic curriculum demands and school’s limited
influence on children after school hours [27,28]. There is a potential
risk of widening existing health inequalities despite improving PA
across the population in policy driven in-school-based program as
uptake by schools is voluntary [29,30]. Children who are naturally
motivated towards PA will tend to make the voluntary change as was
in case of other heath promotion programs like water fluoridation
[31]. Additionally, children with disability would also be unable
to participate in the PA exasperating inequalities. However, staff
training provided will help to deal with students with disability and
poor motivation using Weiss’s Ten commandment format [32] and
a reward system for children [33].
After-school programs (ASPs) are cost effective and promising
venues for increased PA in children due to more flexible schedules
than schools, high nationwide enrolment, participation of primarily
low-income and minority youth at high risk for low engagement
in PA [28-36]. Additionally, qualitative study by Rawlins, et al. of
African and South Asian communities from low SEC in London
found neighbourhood constraints as one of the barriers for
children to engage in PA. Parents reported road safety as well as
‘stranger danger’ in the local parks as a concern. Cost was another
barrier to PA cited by low SEC parents who were unable to pay for
activities such as swimming lessons outside of school. Hence, as
previously researched a school environment offering structured PA
opportunities in school and in ASP can have a positive influence on
PA in children [11].
However, school as a mere opportunity may not be enough
to determine that children will engage in PA as this behaviour
requires child’s motivation and subsequent decision to partake
in the activities offered at school despite providing an enabling
environment. Social cognitive variables such as self- efficacy, motivation, self-esteem, and enjoyment are key to decisions to
engage in PA [38]. As previously found, these are fostered through
peers, parent and staff creating a positive social environment [39].
Children who feel supported in multiple settings such as home as
well school are more likely to engage in PA [28-42]. Barriers to
self-efficacy can be overcome through verbal persuasion by PE
teachers through rewards and incentives [43]. Parental modelling
and attitude towards healthy behaviour also has a strong influence
on children adopting health behaviours [44,45]. Hence, a positive
physical and social environment can help to engage children in PA.
Additionally, increased shared decision-making and increased
participant engagement has also found to reduce inequalities
especially in the targeted low SEC groups [46]. However, there may
be a possibility that parents with low education level in this group
in Ealing may not be able to fully support their children due to lack
of understanding and comprehension because of language barriers
and exacerbate inequalities. A study conducted in Switzerland with
culturally heterogenic ethnic target group provided information
to parents about national guidelines and health benefits in ten
different languages found a positive impact on migrant community
[47].
This intervention offers information about PA to support their
children in most common languages used in this area of Ealing.
However, it has also been found parental involvement in
motivating children to increase their PA is difficult and challenging
despite mitigating language barriers [48-49]. Barriers to direct
parental involvement include parents own health beliefs and
beliefs about control about matters such as weather, lack of time
and distance from work and school [50]. A qualitative study found
that when child’s health status is provided to the parents through
regular feedbacks, providing wide range of potential PA benefits for
the whole family and careful consideration for the family structure
was taken into account, parents encouraged their children to
engage in PA [51].
Thus, social support of family, staff and peers targeting at low
SEC children from ethnic minorities in a safe physical environment
of school and ASP will hope to reduce inequalities that would have
been created if we had taken a stand alone universal approach to the
intervention [52]. And these social influences will help to increase
children’s perceptions in physical competencies and motivation,
encouraging them to engage in PA [11, 28]. Ecological frameworks
using school setting and social influences to increase children’s
PA levels could face ethical challenges. Children in school setting
are generally approached as a group as a means to encourage
participation and peer influence is known to affect decision-making
[53]. Some children may feel pressurised to partake in PA due to
peers participating or some children may feel singled-out whose
parents haven’t given consent for intervention participation [53].
To mitigate this challenge, staff will be encouraged to offer alternate
activities to non-participating children in a manner that these are
not perceived as a punishment but rather an attractive proposition
[53]. Verbal persuasion by staff could make participating children
vulnerable threatening their autonomy [54]. And incentives to
children could be considered ethically inappropriate. However,
there is no consensus of this ethical concern in research [55]. A
merit system as incentives used for this intervention is not overly
large and hence not seen as unduly coercive [56,57]. Financial
incentives to parents have been successful especially for low
SEC in influencing health promoting behaviours as in case of
immunisations [58]. Hence, rewards offered in the form of financial
incentives and merits are considered as potential benefit of the
plan and no harm is considered to themselves or others removing
ethical challenges [53].
Although, socio-ecological framework minimises the sole
responsibility of the children about their health by not overemphasising
the role-played by child’s behaviour and considers
social influences, it could result in coercion [59]. Some writers have
argued that physical inactivity is considered as a risk of poor health
by social factor influences resulting in invading child’s or their
families volition [60]. In order to minimise the risk of coercion,
active involvement of the children and their parents in defining
the problem through educational sessions, giving consent to send
their children to ASP and goal-setting of the targets by the children
themselves during huddles may present a more ethical solution
[15]. As previously researched, skills learning of goals setting,
self-monitoring and self-reaction fosters self-efficacy resulting
in greater autonomy [61,62,63]. Another ethical dilemma may be
stigmatisation [8] as personal heath status of child will be used to
encourage parental involvement. This can be minimised by keeping
all identified information absolutely confidential and addressed
through informed consent process.
Implementation and Evaluation
The intervention in schools can be delivered through School Sports Partnership (SSP), a key organisation of Ealing Community Sport and Physical Activity Network (CSPAN) whose commitment is to increase participation in sport and physical activity in Ealing borough and to encourage people to lead healthier lifestyles [64]. CSPAN and SSP have successfully improved standards in physical education between 2003 and 2010 through various links between schools and increased community involvement in primary and secondary schools. Although, future of SSP is somewhat fragmented in some parts of the country due to budget cuts, it has shown positive impact in increasing physical activity in children and adults in Ealing through various program such as Lets Go South all [64,65]. Intervention and control groups will be matched according to number of children, playground and ASP usage before the start of the program. And PA levels will be measured prior to the observation method SOPLAY [66] to measure activity of children as sedentary, walking or very active. Using the RE-AIM framework (Table 1), this article outlines a theoretical process of Lets Get Fit Ealing from its inception to end of the intervention period.
Reach
All schools in the deprived areas of the Ealing Borough will be invited to participate. After receiving consent from parents of the children in participating schools, children will be given the pre and post intervention questionnaires. These have been used previously for PA promotion [67]. Some of the challenges using this questionnaire could be inaccurate completion by the children as self-reporting is vulnerable to recall biases and social desirability [72]. To mitigate this challenge, PA questionnaire can adapt using the guidelines offered in Alice et. Al, designing and testing questionnaires for children [68].
Effectiveness
Children who are already active may be more motivated to further increase their PA levels [15] and present a barrier towards effectiveness to reach our target population. A combination of direct observations through SOPLAY and accelerometer will help us determine the intervention effectiveness [66]. Direct observations will offer assessment of pattern, frequency and intensity of behaviour as well as contextual information on PA behaviour of children, but this method is time consuming [69]. This will be coupled with use of accelerometers offering assessment strategy to consider and identify factors such as proportion of populations for whom behaviour change versus stability of targeted outcome [15]. Participation in PA during out of school hours are considered to be low due to low parental buy-ins and parental concerns of safety of the areas in low SEC [14]. This is mitigated through parental involvement into the intervention plan and the ASP component to the intervention plan [14-70].
Adoption
Schools are also busy places and may not have the capacity to support research activity such as helping children complete the questionnaires or attend staff training [71]. As previously found in school-based PA promotion research (Verjans-Janssen et al., 2018), reasons for non- participation could include other ASP program already running in schools, already active PA policy, more children to teacher ratio or schools may think the children are already active enough. In a study by Janssen et al., these were mitigated by initial collaborative meetings with other health programs and combining efforts [72]. In the same study, reasons for lack of adoption for nonparticipating were top down decisions by head teachers without teachers involvement [72]. Hence, teacher involvement meetings during developmental stages could mitigate this challenge. Benefits of intervention to children in terms of either change in behaviours, costs-benefit analysis and clear role descriptions and incentives for staff involvement will be given [73].
Implementation
Although school staff were given the flexibility to implement PA components when it best suited their school or class, teacher burden relating to planning and implementation may present as a barrier for in-school component of the intervention [14].Management buyins and teacher professional development training to implement the intervention in school as well as training and support to be provided in ASP could help to mitigate this challenge [74]. Additional support could be offered providing by a key support person to help support staff implement the intervention [72].
Maintenance
Funding is an important factor in maintenance of an intervention plan and can become a challenge to sustain the intervention in the long-term [75]. A physical environment that is conducive to engaging children in increased PA such as well-kept playgrounds, replacing faulty PA equipment and any other material needed to support PA activities during school and in the ASP, requires funding. As found in previous research, partnership working with funding bodies such as Ealing Council in collaboration with SSP and CSPAN can increase knowledge, skills and resources of the schools [75]. Previous research has shown that presence of a student intern or a key worker from school were facilitating factors in continuing the intervention in the long run that also requires funding [72-78].
Conclusion
Socio-ecological framework offers a comprehensive approach to increasing levels of PA in children from ethnic and low SEC background of Ealing because it addresses not only the individual characteristics but also social and environmental influences. With a large proportion of inactive children residing in this borough and high levels of preventable chronic condition such as childhood obesity, the solution presents a great opportunity to increase PA in children that is based on previous successful school-based research. Re-Aim framework used in this report provides a systematic and methodical approach to potential barriers and offers mitigating strategies. Caveats to implementation and evaluation include support in the form of resources and funding will be available because of local authority and school management buy-ins to deliver this intervention. Additionally, it is assumed that PA measurements through accelerometer are based on true sedentary time [15]. Limitation of this intervention is that it does not consider biological differences such as gender previously known to impact PA levels. Overall, Lets Get Fit Ealing offers a theory-based solution to increase PA activity in children.
References
- London Borough of Ealing. (2018). Sport And Physical Activity Strategy 2012 - 2018 | Ealing Council. (online) Ealing.gov.uk.
- Gov uk (2019) Physical inactivity - GOV.UK Ethnicity facts and figures.
- Rawlins E, Baker G, Maynard M, Harding S (2013) Perceptions of healthy eating and physical activity in an ethnically diverse sample of young children and their parents: the DEAL prevention of obesity study. Journal of Human Nutrition and Dietetics. Blackwell Publishing Ltd 26(2): 132-144.
- Bronfenbrenner U (1981) The Ecology of Human Development-Experiments by Nature and Design, The Educational Forum. Informa UK Limited 46(1): 117-123.
- NHS England (2015) Physical activity in children Health Survey for England 2015: Physical activity in
- Sports England (2019) Latest Activity Figures on Children and Young People Published | Sport (online) Sport England.
- Love R, Adams J, Atkin A, Van Sluijs E (2019) Socioeconomic and ethnic differences in children’s vigorous intensity physical activity: A cross-sectional analysis of the UK Millennium Cohort BMJ Open. BMJ Publishing Group 9(5): e027627.
- Spence JC, Lee RE (2003) Toward a comprehensive model of physical activity. Psychology of Sport and Exercise. Elsevier 4(1): 7-24.
- Ealing Council (2004) Indices of Deprivation For Ealing | Ealing Council.
- Sallis JF, Bauman A, Pratt, M (1998) Environmental and policy interventions to promote physical activity. American Journal of Preventive Medicine. Elsevier 15(4): 379-397.
- Sallis JF, Conway TL, Prochaska JJ, Mckenzie TL, Marshall SJ (2001) The Association of School Environments with Youth Physical Activity. American Journal of Public Health 91(4): 618-620.
- Zhang T, Solmon MA, Gao Z, Kosma M (2012) Promoting School Students’ Physical Activity: A Social Ecological Perspective. Journal of Applied Sport Psychology 24(1): 92-105.
- McKay HA, Macdonald HM, Nettlefold L, Masse LC, Day M, et al. (2015) Action Schools! BC implementation: From efficacy to effectiveness to scale-up. British Journal of Sports BMJ Publishing Group 49(4): 210-218.
- Taylor SL, Noonan RJ, Knowles ZR, Owen MB, McGrane B, et al. (2018) Evaluation of a pilot school-based physical activity clustered randomised controlled trial-active schools: Skelmersdale. International Journal of Environmental Research and Public MDPI AG 15(5): 1011.
- Wieland ML, Biggs BK, Brockman TA, Johnson A, Meiers SJ, et al. (2020) Club Fit: Development of a Physical Activity and Healthy Eating Intervention at a Boys & Girls Club After School Program. Journal of Primary Prevention. Springer 41(2): 153-170.
- Van Kann DH H, Kremers SPJ, de Vries NK, de Vries SI, Jansen MWJ (2016) The effect of a school-centered multicomponent intervention on daily physical activity and sedentary behavior in primary school children: The Active Living study. Preventive Medicine. Academic Press Inc 89: 64-69.
- Okely AD, Lubans DR, Morgan PJ, Cotton W, Peralta L, et al. (2017) Promoting physical activity among adolescent girls: The Girls in Sport group randomized trial. International Journal of Behavioral Nutrition and Physical Activity. BioMed Central Ltd 14(1).
- Glasgow RE, Vogt TM, Boles SM (1999) Evaluating the public health impact of health promotion interventions: The RE-AIM framework. American Journal of Public Health. American Public Health Association Inc 89(9): 1322-1327.
- Kessler RS, Peyton Purcell E, Glasgow RE, Klesges LM, Benkeser RM, et al. (2012) What Does It Mean to “‘Employ’” the RE-AIM Model?. Evaluation & the Health Professions 36(1): 44-66.
- Taylor SL, Noonan RJ, Knowles ZR, Owen MB, Fairclough SJ (2018) Process evaluation of a pilot multi-component physical activity intervention - Active schools: Skelmersdale. BMC Public Health. BioMed Central Ltd 18(1): 1-16.
- Umstattd Meyer MR, Sharkey JR, Patterson MS, Dean WR (2013) Understanding contextual barriers, supports, and opportunities for physical activity among Mexican-origin children in Texas border colonias: a descriptive study. BMC public health. BioMed Central 13(1): 14.
- Davidson Z., Simen-Kapeu A, Veugelers PJ (2010) Neighborhood determinants of self- efficacy, physical activity, and body weights among Canadian children. Health and Place. Elsevier Ltd 16(3): 567-572.
- Gidlow CJ, Ellis NJ (2011) Neighbourhood green space in deprived urban communities: Issues and barriers to use. Local Environment. Routledge 16(10): 989-1002.
- Sallis, JF, McKenzie TL, Alcaraz JE, Kolody B, Faucette N, et al. (1997) The effects of a 2-year physical education program (SPARK) on physical activity and fitness in elementary school students. American Journal of Public Health. American Public Health Association Inc 87(8): 1328-1334.
- TUDOR-LOCKE C, LEE SM, MORGAN CF, BEIGHLE A, PANGRAZI RP (2006) Children’s Pedometer-Determined Physical Activity during the Segmented School Day. Medicine & Science in Sports & Exercise, 38(10): 1732-1738.
- Kropski JA, Keckley PH, Jensen GL (2008) School-based obesity prevention programs: An evidence-based review. Obesity. John Wiley & Sons, Ltd 16(5): 1009-1018.
- Slater SJ, Nicholson L, Chriqui J, Turner L, Chaloupka F, et al. (2012) The impact of state laws and district policies on physical education and recess practices in a nationally representative sample of US public elementary schools. Archives of Pediatrics and Adolescent Medicine, 166(4): 311-316.
- Harmon BE, Nigg CR, Long C, Amato K, Anwar Kutchman E, et al. (2014) What matters when children play: Influence of social cognitive theory and perceived environment on levels of physical activity among elementary-aged youth. Psychology of Sport and Exercise. Elsevier 15(3): 272-279.
- Maziak W, Ward KD, Stockton MB (2008) Childhood obesity: Are we missing the big picture? Obesity Reviews 9(1): 35-42.
- Lorenc T, Petticrew M, Welch V, Tugwell P (2013) What types of interventions generate inequalities? Evidence from systematic reviews. Journal of Epidemiology and Community Health. BMJ Publishing Group Ltd 67(2): 190-193.
- White M, Adams J, Heywood P (2009) How and why do interventions that increase health overall widen inequalities within populations?, Public Health Research Programme.
- Weiss MR (2000) Motivating Kids in Physical Activity.
- Harland J, White M, Drinkwater C, Chinn D, Farr L, et al. (1999) The Newcastle exercise project: A randomised controlled trial of methods to promote physical activity in primary British Medical Journal. BMJ Publishing Group 319(7213): 828: 832.
- Iversen CSS, Nigg C, Titchenal CA (2011) The impact of an elementary after-school nutrition and physical activity program on children’s fruit and vegetable intake, physical activity, and body mass index: Fun 5. Hawaii medical journal 70(7 Suppl 1): 37-41.
- Branscum P, Sharma M (2012) After-School Based Obesity Prevention Interventions: A Comprehensive Review of the Literature. International Journal of Environmental Research and Public Molecular Diversity Preservation International 9(4): pp. 1438-1457.
- Beets MW, Webster C, Saunders R, Huberty JL (2013) Translating Policies into Practice. Health Promotion Practice. SAGE PublicationsSage CA: Los Angeles, CA 14(2): 228-237.
- Bauman AE, Reis RS, Sallis JF, Wells JC, Loos RJF, et al, (2012) Correlates of physical activity: Why are some people physically active and others not? The Lancet. Lancet Publishing Group pp 258-271.
- Rhodes RE, McEwan D, Rebar AL (2019) Theories of physical activity behaviour change: A history and synthesis of approaches. Psychology of Sport and Exercise. Elsevier Ltd pp. 100-109.
- Prochaska JJ, Rodgers MW, Sallis JF (2002) Association of parent and peer support with adolescent physical activity. Research Quarterly for Exercise and Sport. Taylor & Francis Group 73(2): 206-210.
- Weiss MR, Duncan SC (1992) The relationship between physical competence and peer acceptance in the context of children’s sports participation. Journal of Sport & Exercise Psychology 14: 177-191.
- Brustad RJ (1996) Attraction to physical activity in urban schoolchildren: Parental socialization and gender influences. Research Quarterly for Exercise and Sport. Res Q Exerc Sport 67(3): 316-
- Kunesh MA, Hasbrook CA, Lewthwaite R (2016) Physical Activity Socialization: Peer Interactions and Affective Responses among a Sample of Sixth Grade Girls. Sociology of Sport Human Kinetics, 9(4): 385-396.
- Bandura A (2004) Health Promotion by Social Cognitive Means’, Health Education & Behavior. SAGE Publications 31(2): 143-164.
- Mcguire MT, Hannan PJ, Neumark-Sztainer D, Cossrow NHF, Story M (2002) Parental correlates of physical activity in a racially/ethnically diverse adolescent sample. Journal of Adolescent Elsevier, 30(4): 253-261.
- VAN DER HORST K, PAW MJCA, TWISK JWR, VAN MECHELEN W (2007) A Brief Review on Correlates of Physical Activity and Sedentariness in Youth. Medicine & Science in Sports & Exercise 39(8): 1241-1250.
- Durand MA, Carpenter L, Dolan H, Bravo P, Mann M, et al. (2014) Do interventions designed to support shared decision- making reduce health inequalities? A systematic review and meta-analysis. PLoS ONE. Public Library of Science 9(4).
- Bürgi F, Niederer I, Schindler C, Bodenmann P, Marques-Vidal P (2012) Effect of a lifestyle intervention on adiposity and fitness in socially disadvantaged subgroups of preschoolers: A cluster-randomized trial (Ballabeina). Preventive Medicine Prev Med 54(5): 335-340.
- Langford R, Bonell C, Jones H, Campbell R (2015) Obesity prevention and the Health promoting Schools framework: Essential components and barriers to success. International Journal of Behavioral Nutrition and Physical Activity. BioMed Central Ltd., 12(1): 15.
- Verjans-Janssen SRB, van de Kolk I, Van Kann DHH, Kremers SPJ, Gerards SMPL (2018) Effectiveness of school-based physical activity and nutrition interventions with direct parental involvement on children’s BMI and energy balance-related behaviors-A systematic review. PLOS ONE. Edited by J. P. van Wouwe. Public Library of Science 13(9): e0204560.
- Rhodes RE, Lim C (2018) Promoting Parent and Child Physical Activity Together: Elicitation of Potential Intervention Targets and Preferences. Health Education and Behavior. SAGE Publications Inc 45(1): 112-123.
- Brown HE, Schiff A, Van Sluijs EMF (2015) Engaging families in physical activity research: A family-based focus group study. BMC Public Health. BioMed Central Ltd 15(1).
- Vander Ploeg KA, Maximova K, McGavock J, Davis W, Veugelers P (2014) Do school- based physical activity interventions increase or reduce inequalities in health?. Social Science and Elsevier Ltd 112: 80-87.
- Felzmann H (2009) Ethical Issues in School-Based Research. Research Ethics. SAGE Publications 5(3): 104-109.
- Gardner J (2014) Ethical issues in public health promotion. South African Journal of Bioethics and Health and Medical Publishing Group 7(1): 30.
- Borzekowski DLG, Rickert VI, Ipp L, Fortenberry JD (2003) At what price? The current state of subject payment in adolescent research. Journal of Adolescent Health. Elsevier Inc 33(5): 378-384.
- Scherer DG, Brody JL, Annett RD, Hetter J, Roberts LW, et al. (2005) Financial compensation to adolescents for participation in biomedical research: Adolescent and parent perspectives in seven studies. Journal of Pediatrics. Mosby Inc 146(4): 552-558.
- Bagleya SJ, Reynolds WW, Nelson RM (2007) Is a “wage-payment” model for research participation appropriate for children?. American Academy of Pediatrics, 119(1): 46-51.
- Achat H, Mcintyre P, Burgess M (1999) Health care incentives in immunisation. Australian and New Zealand Journal of Public Health. Public Health Association of Australia Inc 23(3): 285-288.
- McLeroy K, Bibeau D, Steckler, A, Glanz K (1988) An Ecological Perspective on Health Promotion Programs. Health Education Quarterly 15(4): 351-377.
- Beauchamp D (1976) Public Health as Social Justice. Inquiry 13(1): 3-14.
- Schunk DH (1990) Goal Setting and Self-Efficacy During Self-Regulated Learning. Educational Lawrence Erlbaum Associates Inc 25(1): 71-86.
- World Health Organisation (2001) Skills for Health Skills-based health education including life skills: An important component of a Child-Friendly/Health-Promoting School.
- Cheung E (2004) Goal Setting as Motivational tool in Student’s Self-regulated Learning, Educational Research Quarterly 27(3): 3-9.
- Sports England and London Borough of Ealing (2018) Let’s Go Southall-First Steps- At a glance Southall Dormers Wells.
- London Borough of Ealing (2016) Draft Ealing Health and Wellbeing Strategy 2016-21 Summary | Ealing Council.
- McKenzie TL, Marshall SJ, Sallis JF, Conway TL (2000) Leisure-time physical activity in school environments: An observational study using SOPLAY. Preventive Medicine. Academic Press Inc 30(1): 70-77.
- Collard DCM, Chinapaw MJM, Verhagen EALM, Bakker I, van Mechelen W (2010) Effectiveness of a school-based physical activity-related injury prevention program on risk behavior and neuromotor fitness a cluster randomized controlled trial. International Journal of Behavioral Nutrition and Physical Activity. BioMed Central 7(1):
- Bell A (2007) Designing and testing questionnaires for children. Journal of Research in Nursing Los Angeles 12(5): 461-469.
- Ridgers ND, Stratton G, Fairclough SJ (2006) Physical activity levels of children during school playtime. Sports Medicine. Springer 359-371.
- Austin G, Bell T, Caperchione C, Mummery WK (2011) Translating Research to Practice: Using the RE-AIM Framework to Examine an Evidence-Based Physical Activity Intervention in Primary School Settings. Health Promotion Practice. SAGE PublicationsSage CA: Los Angeles CA 12(6): 932-941.
- Wamp Z (2009) Creating a Culture of Movement The Benefits of Promoting Physical Activity in Schools and the Workplace 36(2): S55-66.
- Janssen M, Toussaint HM, van Mechelen W, Verhagen EALM (2013) Translating the PLAYgrounds program into practice: A process evaluation using the RE-AIM framework. Journal of Science and Medicine in Sport. Elsevier 16(3): 211-216.
- Ginexi EM, Hilton TF (2006) What’s next for translation research? Evaluation & the health Sage PublicationsSage CA: Thousand Oaks, CA, 29(3): 334-347.
- Dzewaltowski DA, Estabrooks PA, Glasgow RE (2004) The Future of Physical Activity Behavior Change Research: What Is Needed to Improve Translation of Research into Health Promotion Practice?. Exercise and Sport Sciences Reviews. Exerc Sport Sci Rev 57-63.
- Cass Y, Price P, Rimes T (2005) Finding the common ground: where health and educational agendas meet--the School Health Incentive Program (SHIP) grants scheme. Health promotion journal of Australia : official journal of Australian Association of Health Promotion Professionals. John Wiley & Sons, Ltd 16(2): 134-137.
- Babakus WS, Thompson JL (2012) Physical activity among South Asian women: A systematic, mixed-methods review. International Journal of Behavioral Nutrition and Physical Activity 1.
- Mackintosh C (2014) Dismantling the school sport partnership infrastructure: findings from a survey of physical education and school sport practitioners. Education 3-13. Routledge 42(4): 432-449.
- Nielsen JV, Skovgaard T, Bredahl TVG, Bugge A, Wedderkopp N, et al. (2018) Using the RE-AIM framework to evaluate a school-based municipal programme tripling time spent on PE. Evaluation and Program Planning. Elsevier Ltd 70: 1-11.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...