Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2638-6003
Case Report(ISSN: 2638-6003) 
Functional Outcome Measures and Patients’ Satisfaction following Primary Total Knee Arthroplasty, a Systematic Review Volume 5 - Issue 4
Bodor Bin sheeha1*, Malcolm Granat2, Anita Williams2, Richard Jones2
- 1College of Health & Rehabilitation Science, Princess Nourah Bint Abdulrahman University, KSA
- 2School of Health and Society, University of Salford Manchester, Salford, UK
Received:October 30, 2021 Published: November 12, 2021
Corresponding author: Bodor Bin sheeha, College of Health & Rehabilitation Science, Princess Nourah Bint Abdul Rahman University, Riyadh, KSA
DOI: 10.32474/OSMOAJ.2021.05.000218
Abstract
Background and Objective: Commonly, only different types of patient-reported outcome measures (PROMs) are used
to measure outcomes post-total knee arthroplasty (TKA), despite their limitations. This review’s objectives were to: assess the
psychometric properties of commonly used PROMs and other objective tools to measure function post-TKA, such as: Performancebased
Outcome Measure (PBOMs), Star Excursion Balance Test (SEBT) and accelerometers to measure physical activity. In addition
to assess the tools used to measure patients’ satisfaction post-TKA.
Methods: A systematic review was conducted to investigate the available methods for measuring TKA outcomes. The
psychometric properties of each method were reviewed to recommend the best tools to capture accurately improvements in
function and satisfaction post-TKA.
Results and Conclusions: KOOS and OKS showed good reliability, validity and sensitivity with a post-TKA population. However,
patient function is multidimensional and requires more than just a questionnaire. Therefore, it is recommended to use other
objective methods in addition to PROMs, such as PBOMs, SEBT and reliable accelerometers to paint a detailed and accurate overall
recovery picture post-TKA. Four of the five PBOMs tests recommended by the Osteoarthritis Research Society International (OARSI)
showed excellent to good psychometric properties with a post-TKA population. ActivPAL show good reliability and had advantages
over other accelerometers in its ability to accurately measure both volume- and event-based patterns. Using one question with
different options to answer to assess satisfaction is not accurate and so it is recommended to use satisfaction tools that cover each
issue in isolation to better understand the impact of each factor on satisfaction.
Keywords: Knee Arthroplasty; Patient-Reported Outcome Measures; Performance-Based Outcome Measures; Star Excursion Balance Test; Free-Living Physical Activity; Satisfaction
Introduction
Individuals with end-stage knee osteoarthritis (KOA) complain that pain persists at rest and at night, which may disturb sleep, in addition to a marked and limited range of motion. Pain and limited movement are major sources limiting physical activity (PA), and subsequently chronic disability [1]. Total knee arthroplasty (TKA) is a cost-effective treatment option for end-stage KOA and the procedures rate is increasing due to high functional demands in an ageing society [2,3]. TKA success has traditionally been evaluated from the surgeon’s perspective, e.g. the presence of surgical complications or implant survival. This is gradually changing to involve the patient when measuring health outcomes and decisionmaking processes. Patient-reported outcome measures (PROMs) have evolved in order to better explore patient perspectives by monitoring the quality of care in health organisations and conducting clinical trial outcomes [4]. However, subjective over/ underestimation and recall bias of PROMs cannot be excluded. So, further objective methods are commonly used post-TKA, such as assessments of functional performance, balance and PA. Each assessment method has its strengths and limitations; therefore, the aim of this review was to systemically identify, appraise and synthesise available studies to determine proper outcome measurements methods to assess outcomes post-TKA.
Materials and Methods
Search strategy
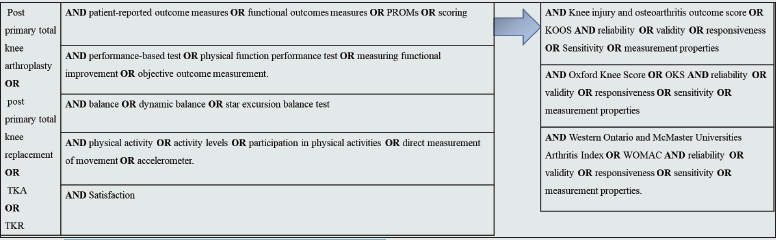
In accordance with PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) guidelines, a systematic review of the literature was conducted electronically, making use of several medical databases including: Cumulative Index to Nursing and Allied Health Literature (CINAHL), Medline/ PubMed, PEDro, Cochrane Library, Cochrane Central Register of Controlled Trials (CENTRAL), ProQuest, TRIP and Google Scholar. To define the search strategy, the PICO (Population, Intervention, Comparison and Outcome) framework was used. The keywords and terms used are shown in Figure 1 and 9. The search was limited to research published in English between 2004 and May 2020 on human adult participants and with full access to articles. Unpublished studies were not included because they are rarely peer-reviewed.
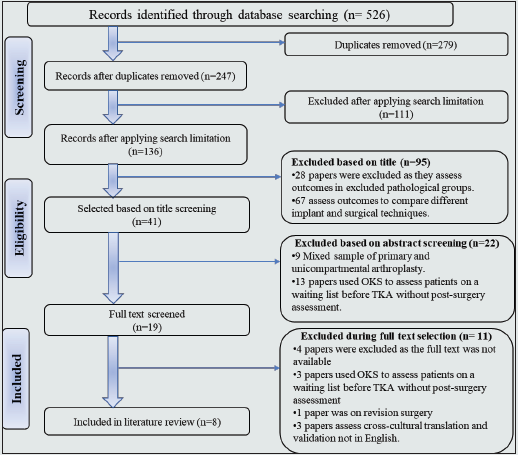
Figure 2: PRISMA 2009 Flow Diagram for Patients Reported Outcome Measures Post-Total knee arthroplasty.
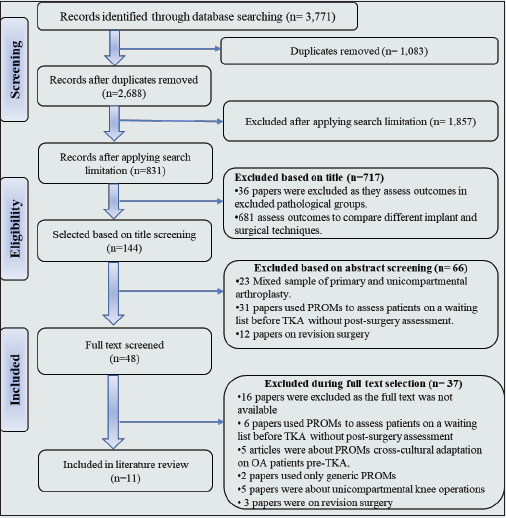
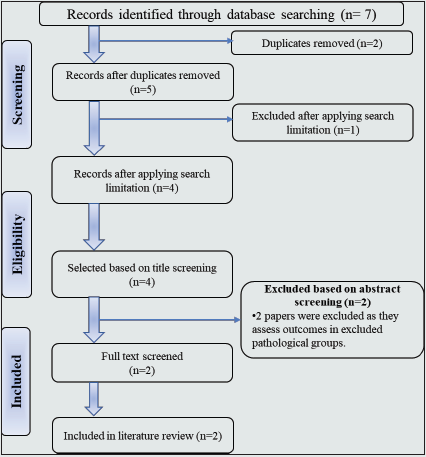
Figure 3: PRISMA Flow Diagram for Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) Post-Total knee arthroplasty.

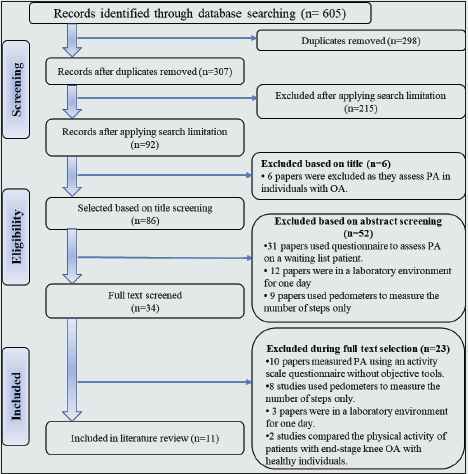
Figure 4: PRISMA Flow Diagram for Knee Injury and Osteoarthritis Outcome Score (KOOS) Post-Total knee arthroplasty.

Eligibility Criteria
Studies were included if they satisfied: any study methodology measuring outcomes post-primary TKA in terms of PROMs alone or combined with patient performance-based tests, dynamic balance, physical-activity measuring devices and satisfaction. However, any study assessing an outcome other than after primary TKA was excluded, such as: post-traumatic and revision TKA outcome measurements, unicompartmental knee-replacement, TKR in pathological groups, such as neurological disorders (stroke, Parkinson’s disease etc.), and post-TKA outcomes based on implant survival, surgical techniques, complications, engineering metallurgic issues and radiographic or any other outcomes not patient generated. Reference management software (Endnote X7) was used to merge results and remove duplicates.
Critical appraisal of risk of methodology bias
Study quality was appraised using CASP (Critical Appraisal Skills Program) and a suitable study-design tools checklist (CASP, 2007) according to two independent reviewers. The CASP tool assesses three main aspects of a research paper: the validity of a study, the quality of the reported results and the value of the conclusions drawn. Positive items (YES) were calculated to estimate the total CASP score and thus assess a study’s internal validity and bias potential. A study with a high positive (YES) score was considered to have low bias risk, and a study with one or more key domains with a negative score (NO) was considered to have high bias risk and so its conclusion was interpreted carefully [5].
Results
Outcomes measurement post-surgery is variable and there are many patient factors that may influence outcomes. Each outcome measure in the literature was assessed independently.
Patient-reported outcome measures (PROMs)
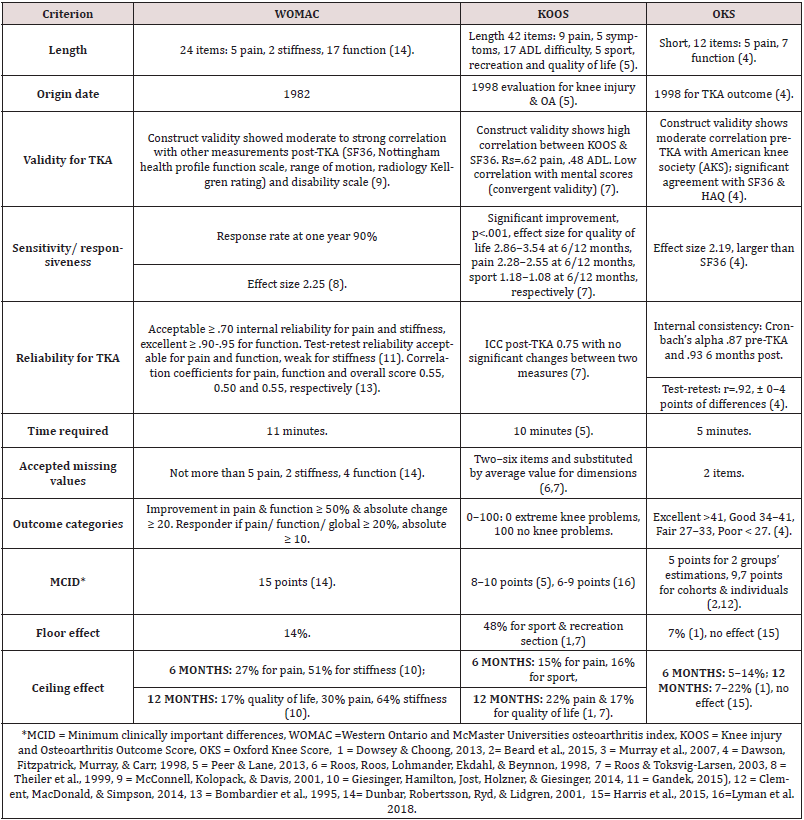
Generic PROMs, such as short forms (SF-36, SF-12) and the EQ-5D questionnaire, provide crucial global assessments of outcomes post-TKA, rather than specific isolated evaluations of pain, satisfaction or function. Generic PROM methods are limited to assessing the specific details required for various disease populations, which may decrease their sensitivity, maximise ceiling effects and produce type-2 errors in hypothesis testing. Specific PROMs address issues pertinent to health-related quality of life in relation to a specific pathology or intervention in order to improve sensitivity, better detect changes and minimise ceiling effects [6]. A PRISMA search strategy for PROMs is summarised in Flow Diagram 2. Six systematic reviews and four prospective cohort studies, as well as a committee survey report from ISAR (International Society of Arthroplasty Registries), reached comparable conclusions; Knee injury and Osteoarthritis Outcome Score (KOOS), Oxford Knee Score (OKS) and the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) are the PROMs most commonly used for assessment post-TKA [4,7,8,9,10,11,12,13, 14,15,16]. It is hard to conclude that there is one best or gold standard for specific PROMs for patients post-TKA from the available evidence, thus in-depth analysis is recommended to explore the PROMs’ (KOOS, OKS, WOMAC) validity, reliability and responsiveness, with details of the function-assessment strengths and limitations of each one (summarised in Table 1). Therefore, this includes any study assessing the measurement properties of WOMAC, KOOS or OKS in patients undergoing TKA at any point in time post-TKA for adult subjects, without any limitation regarding publication date, in order to explore original developments in PROMs.
Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC)
WOMAC is a commonly used specific PROM for lower-limb dysfunction, it has been used for over 30 years, with different patient pathologies, to evaluate changes in patients’ status posttherapeutic intervention. Originally, it assessed pain, joint stiffness and physical function in osteoarthritis hip/knee patients. A PRISMA search strategy for WOMAC is summarised in Flow Diagram 3. Eight studies assessed WOMAC with post-TKA patients, as summarised in Table 2 [6,17,18,19,20,21 ,22,23]. It was originally validated for knee and hip osteoarthritis patients within a double blinded randomized study investigating the effects of two different types of anti-rheumatic drugs on osteoarthritis hip/ knee patients [24]. Pain, stiffness and physical functions fulfil the criteria required for content, construct and face validity. WOMAC is a reliable and responsive PROM for osteoarthritis. Cronbach’s alpha for pain, stiffness and function were, respectively, 0.86–0.89, 0.90–0.91 and 0.90. Test-retest reliability with a one-week interval was 0.68 for both pain and function and 0.48 for stiffness [24]. WOMAC shows moderate to strong validity and excellent physical function-internal consistency with a large effect size post-TKA [6,17,18,19,20, 21,22,23]. It has acceptable pain and stiffness internal consistency, but weak stiffness test-retest reliability. The low sensitivity of WOMAC’s stiffness subscale reduces the overall standardized response mean [6,22]. The ceiling effect was higher than the acceptable percentage of 15% [25] at 6, 12 and 24 months [6,19,20]. These weaknesses in WOMAC’s tools for a post-TKA population are enough to exclude it as an option for assessment tools (Table 1).
Table 2: Characteristics of Reliability and Validity Studies for Patient-reported outcome measures (PROMs).

Knee Injury and Osteoarthritis Outcome Score (KOOS)
KOOS is an extension of WOMAC, which has remained unchanged since 1998. The main purpose of KOOS is to measure short- and long-term follow-up of patients’ opinions about their knee and accompanying problems, with good coverage of function in terms of joint mobility, stability, stiffness, pain sensation, activities of daily living, sport, recreation and knee-related quality of life, as the intended population is the young and middle-aged with post-knee injuries or trauma and patients with KOA. Its main strong point is a short function score which covers functional requirement assessment suitable for active participants while minimizing the ceiling effect [9, 26, 27]. A PRISMA search strategy for KOOS is summarised in Flow Diagram 4. Four studies assessed the psychometric properties of KOOS with post-TKA patients, as summarised in Table 2. KOOS is a valid, reliable and responsive assessment tool for patients post-TKA, it has certain advantages over WOMAC and OKS, especially in groups with high PA expectations and for young subjects [28,29,30,31]. Also, it evaluates knee-related quality of life, which is a crucial issue for the majority of patients post-TKA, something not covered by WOMAC or OKS [28]. All four studies concluded that KOOS has sufficient validity and reliability post-TKA [28,29,30,31]. Special consideration is required if KOOS is used for a 12-month follow-up as the ceiling effect reaches 22% on the pain scale and 17% for quality of life [28], which are above the acceptable ceiling effect percentage of 15% [25] (Table 1). Hence it is recommended to use other measurement scales for patient quality of life and expectations, rather than KOOS [29].
Oxford Knee Score (OKS)
A final version of a 12-item questionnaire was developed to assess patients post-TKA after interviews with patients undergoing joint replacement and a multiple drafting process to identify their experiences and problems post-TKA since 1998 [32]. The main objective of the questionnaire was to measure the patient’s perspective on outcomes post-TKA in a short, reliable, practical and valid way, with good sensitivity to important clinical changes. The questionnaire elicited data on recall symptoms in the previous four weeks. It assessed the severity of pain and the ability to engage in the basic daily activities of living [32, 33]. A PRISMA search strategy for OKS is summarised in Flow Diagram 5. Eight studies assessed the psychometric properties of OKS with post-TKA patients, as summarised in Table 2. OKS is a valid, reliable and responsive assessment tool for the period post-TKA, it has certain advantages over WOMAC and KOOS, as it simple and short. As a PROM’s main concern is to explore outcomes from the patient’s perspective, OKS has the advantage of offering clear MIDC values for all types of studies and is designed to ensure that the results are recognized by patients, in addition to statistical differences, and this may improve the power calculation [11,34,35,36,37,38,39,40]. The ceiling effect is more than acceptable at 12 months follow-up [39], as is KOOS [25] (Table 1). In contrast, OKS does not assess knee-related quality of life and recreation as KOOS does.
Functional performance
The assessment of daily and overall PA is essential, as the proportion of young patients undergoing TKA is increasing, and it is important for assessments to be compatible with a core set of definitions and the International Classification of Functioning, Disability and Health definitions of the World Health Organization [8]. Also, PROM results cannot exclude a research participant effect (RPE) or subjective over/underestimation due to psychosocial effects or pain from other joints, such as hips or back [41,42,43]. Hence, objective clinical evaluation methods can minimise patients’ subjective over/underestimations of outcomes, though RPE cannot be excluded. Objective assessment has some advantages over PROMs, such as a lack of ceiling effects and more precision and responsiveness, and it does not require cultural and language adaptation. In contrast, it is costly and not feasible in clinical practice, thus limited to research centres, and it requires specific in-depth training in its use to ensure reliability. In addition, technically, it is only applicable to small groups, in contrast to PROMs. Many reliable objective measurement tools have been used in populations post-TKA, such as video-motion analysis with a force plate, which offers ultimate functional evaluation [44,45,46]. Performance-based Outcome Measures (PBOMs), a balance test and free-living PA accelerometer are clinically feasible and are less costly assessment tools than video-motion analysis to capture functional improvements post-TKA.
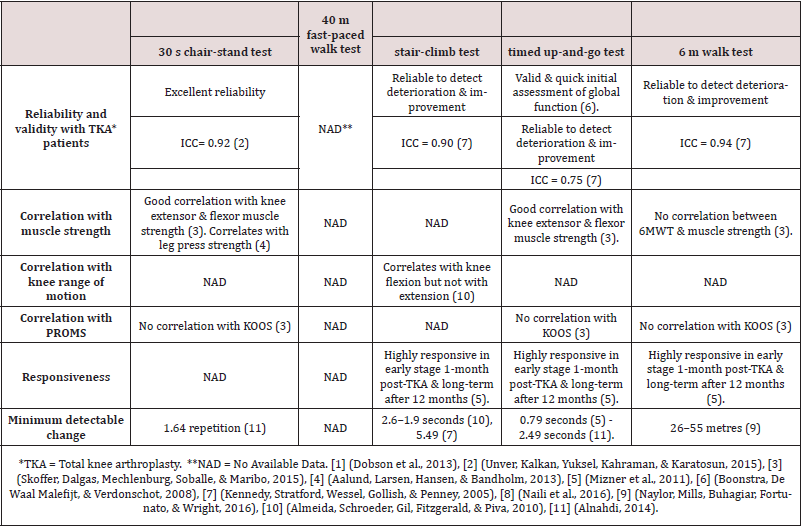
Performance-based Outcome Measures (PBOMs)
PBOMs are sensitive for detecting change, responsive and have a minimal ceiling effect, as well as being feasible. PROMs and PBOM measurement tools assess different aspects of function post- TKA. PROMs mainly assess patients’ functional ability beliefs and experiences, while objective functional assessment instruments and PBOM measurement tools evaluate patients’ actual ability and function and highly correlate with body impairments [7,47]. A PRISMA search strategy for PBOMs is summarised in Flow Diagram 6. Twelve studies assessed PBOMs post-TKA: Six studies explored the correlation between PBOMs and other outcomes post-TKA [14,47,48,49,50,51], and six studies assessed the psychometric properties of PBOMs in a post-TKA population [52,53,54,55,56,57] (summarised in Table 3). Four of the five PBOMs tests recommended by the Osteoarthritis Research Society International (OARSI) show excellent to good psychometric properties with a post-TKA population. These are: 30 s chair-stand test (30 s CT), 40 m fastpaced walk test (40 m FPWT), a stair-climb test (SCT), timed upand- go test (TUG) and a 6 m walk test (6MWT) [58], summarised in Table 4. A timed up-and-go test, a valid quick functional assessment tool, a 30 s chair-stand test and a timed up and go and walking test showed good correlation with knee extensor and flexor muscle strength. The stair climb test correlated with knee flexion range of motion.
Table 3: Characteristics of patients’ Performance Based Outcome Measurements post-total knee arthroplasty studies.
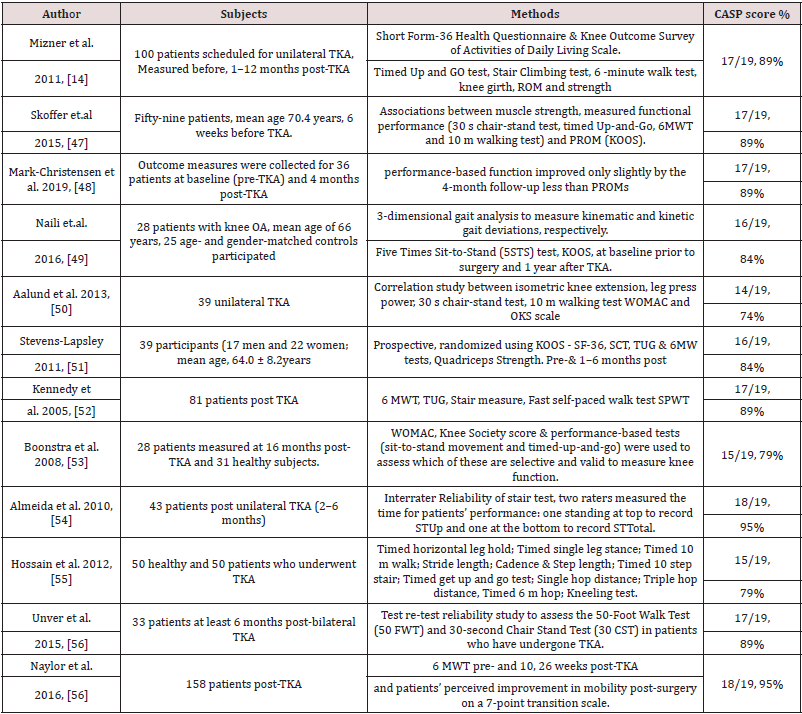
Table 4: Measurements Criteria for recommended Performance -Based test by Osteoarthritis Research Society International (OARSI) [1].
Balance
Instability in end-stage knee OA is one of the main factors that correlate with disability and a high risk of falling [59,60]. Assessing balance improvement post-TKA is essential to capture functional improvements. Dynamic balance has an advantage over a static based assessment, in that it closely mimics PA demand, as the history of falling in the OA population is seen more during dynamic activities rather than in a static position. Dynamic balance in individuals with OA is commonly assessed using a step test [61,62,63]. The test only assesses dynamic balance in one direction, it does not reflect daily activity balance requirements, and muscular endurance may affect test performance. Dynamic balance may be assessed with another test, i.e. the Star Excursion Balance Test (SEBT). In a SEBT, the individual stands in the centre of the grid and is instructed to stand on the affected or operated leg while reaching out as far as possible in one of three directions with the other lower extremities, and then returns that leg to the centre. The assessor measures the reach distance in each direction, in centimetres, and then normalises the average of the three trials to leg length [64,65]. Thus, this test assesses balance in multiple directions, which may better mimic daily life activity requirements, and it has excellent inter-rater reliability for healthy participants. A PRISMA search strategy for SEBT is summarised in Flow Diagram 7. Two studies used SEBT with knee OA patients, one assessed reliability with early to moderate knee OA and responsiveness after an exercise programme. SEBT showed excellent psychometric properties in early and moderate stages of knee OA [66]. The other study by Al- Khlaifat et al. (2016) found significant improvements in dynamic balance after six weeks of training for knee OA patients, which indicates good sensitivity to detect improvements after an exercise programme [67]. Interestingly, no studies have assessed dynamic balance post-TKA using SEBT or a reliability study with individuals with end-stage OA or post-TKA.
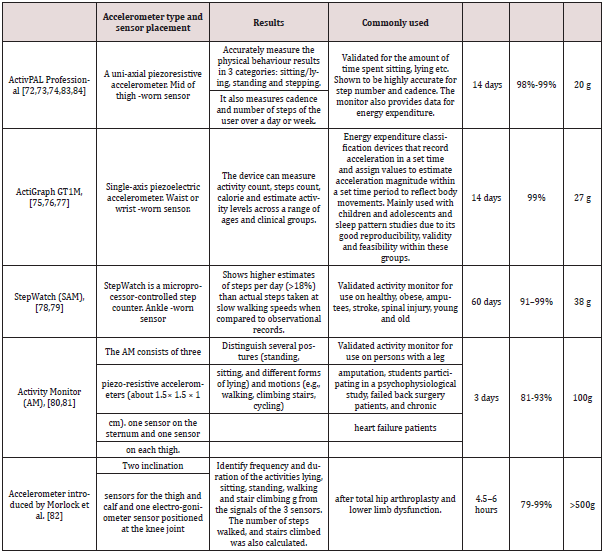
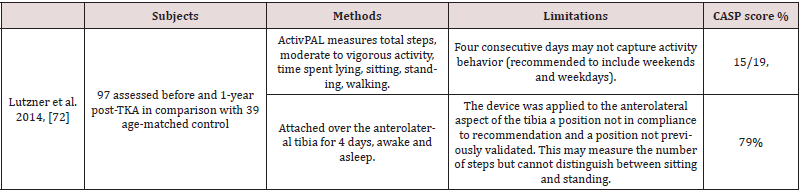
Assessment of free-living physical activity
Although the main outcomes expected after TKA are reduced
pain and improved functional performance, there is limited
research on overall free-living physical behaviour (PB) outcomes
post-TKA. According to the World Health Organisation, physical
activity (PA) is defined as any bodily movement that results in
energy expenditure by the skeletal muscles. This includes sport,
exercise and other activities, such as playing, walking, doing
household chores, gardening and dancing. PA has many positive
benefits, such as improved cardio-respiratory fitness and enhanced
physical and cognitive function. In addition, it lowers the rates of
coronary heart disease, high blood pressure, stroke, diabetes, colon
and breast cancer, depression and the risk of falling [68]. Many
methods are used to assess PA, e.g. direct observation, diaries and
questionnaires, though these have subjective limitations and high
rates of under/overestimation. In contrast, objective technology
analysis, such as foot switches, optical motion analysis, gait mats
and force plates, offer a great degree of accuracy, though they
have the limitation of being unsuitable for free-living physical
activity assessment and so are primarily for laboratory use. Whilst
they can collect objective, valid and reliable data to analyse the
quality of movements during assessment, they cannot capture
the actual quantity and quality of daily life movements [69,70].
Accelerometers have the advantage of offering free-living reliable,
feasible and environmentally constrained methods to monitor PA
without subjective limitations and reasonable cost when compared
to laboratory motion-analysis technology. An accelerometer has the
advantage of detecting the intensity and frequency of movements
better than a pedometer or actometer [71]. A PRISMA search
strategy for PA measured by accelerometers is summarised in Flow
Diagram 8. Abstract screening found that 11 papers satisfied the
eligibility criteria. Eleven studies assessed PA post-TKA utilizing
different types of accelerometers. Three studies used ActivPAL
[72,73,74], three used ActiGraph 1GT1M [75,76,77], two used
StepWatch Activity Monitor (SAM) [78,79], two studies used an
Activity Monitor (AM) accelerometer [80,81], and the last study
used hardware introduced by Morlock et al. (2015) [82]; study
summaries and quality assessments are presented in Table 5. All
accelerometer characteristics and their outcomes are summarised
in Table 6. The hardware accelerometer introduced by Morlock et
al. [82], the AM accelerometer [80,81], and the ActivPAL [72,73,74]
accelerometer assess, in addition to steps per day, the time spent
lying, standing and sitting. This accelerometer category –postural
classification devices –has the ability to determine the inclination
of one or more body segments and drive the body position. The AM
and Morlock et al. accelerometers are heavy, which is a disadvantage,
at 100 grams and 500 grams, respectively. They consist of three
sensors applied to the sternum and one on each thigh. Their heavy
weight and multiple sensors require professional application and
the patient needs to take it off for sleeping or showering, which may
decrease the time it is worn and its feasibility [80,81,82]. On the
other hand, ActivPAL had the advantage of being light in weight,
at only 20 grams, with one small sensor easily applied to the midthigh,
and also waterproof. The patient can wear it day and night,
which improves the accuracy of measurements [72,73,74] (see
Table 6).
ActivPAL has the ability to measure volume free-living PA by
considering external environmental confounding factors in addition
to patterns of PA and sedentary behaviour. It assesses low-energy
positions (sitting and lying) to estimate sedentary behaviour.
It also accurately assesses the start time for each position and
the duration spent in it. In a similar manner, it estimates upright
events (standing, stepping) time in addition to the number of
steps and average cadence [83,84]. ActivPAL showed good interdevice
reliability, ranging from 0.79 to 0.99. The mean percentage
differences between ActivPAL and direct observation of the total
time spent sitting and standing were 0.19% (limit of agreement
from −0.68% to 1.06%) and 1.4% (limit of agreement from-
6.2% to 9.1%) [84] (Table 6). ActiGraph is an energy expenditure
classification device that records acceleration in a set time and
assign values to estimate acceleration magnitude within a set time
period to reflect body movements. It has the ability to estimate energy expenditure, but may overestimate low-level activities and
underestimate vigorous ones. Its ability to detect body posture is
limited due to minimal acceleration records when standing, and
similarly in a sitting position because it worn at hip level [83,84].
Table 5: Characteristics and limitations for physical activity accelerometers post-Total Knee Arthroplasty Studies.
Patients’ Satisfaction
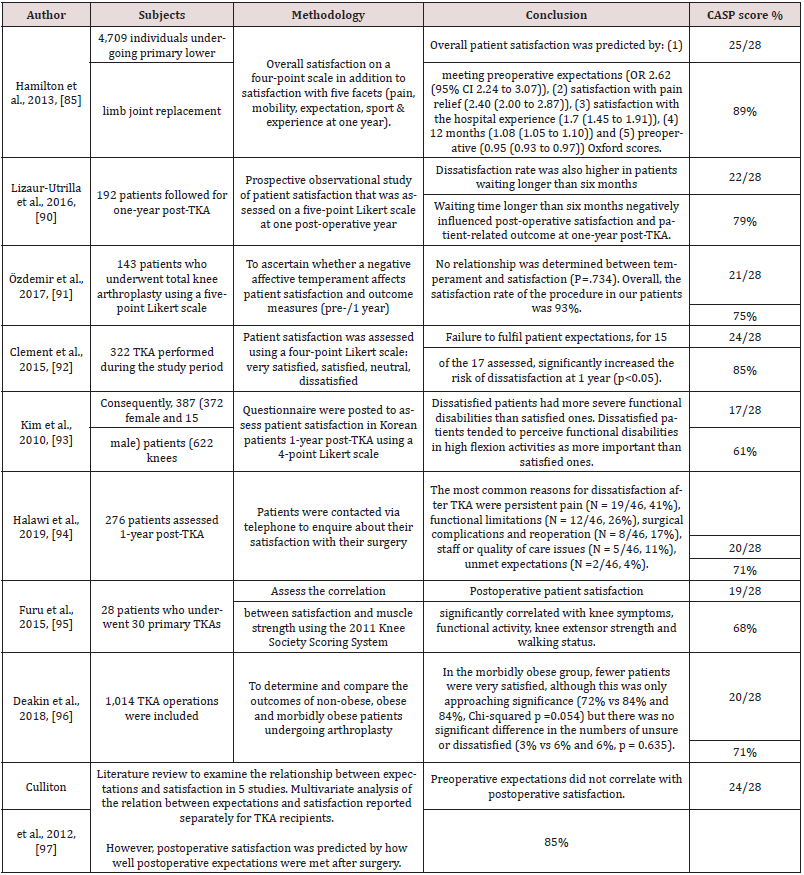
Satisfaction post-TKA is usually linked to functional improvements and pain reduction. Much research attempts to improve the understanding of patients’ satisfaction post-TKA, as the degree of satisfaction post-TKA is significantly less than for post-total hip arthroplasty, with up to 20% of patients post-TKA not being satisfied [85,86,87,88,89]. To understand the patientsatisfaction assessment tools used post-TKA, a systematic review of the patient satisfaction post-primary TKA literature was conducted. A PRISMA search strategy was used to devise a transparent articleselection process, which is summarised in Flow Diagram 9. Full-text screening found that 27 papers satisfied the eligibility criteria, these are included and summarised in Table 7. Eleven papers assessed the factors that might affect satisfaction one-year post-TKA [90,91, 92,93,94,95,96,97,98,99,100], seven studies assessed the effect 2–5 years post-TKA [101,102,103,104,105,106,107], one study assessed satisfaction 24 hours after surgery[108], four studies developed predictions for three months and one year satisfaction post-TKA [85,109,110,111], two studies assessed the satisfaction rate at one year post-TKA in Korean and Saudi patients [112,113], one recent study assessed satisfaction with single question correlation with other PROMs [114], and one study assessed satisfaction changes nine years post-TKA [115]. Patients’ satisfaction post-TKA is usually measured using one question with different response options on a five-point Likert scale (very satisfied, satisfied, neutral, dissatisfied, very dissatisfied) [90,91,92] , a 4-point Likert scale (very satisfied, satisfied, unsure, dissatisfied) [93,94,95,96] , a visual analogue scale (VAS) for satisfaction [97,98] or by asking patients if they are satisfied with their TKA (and given the options of answering “Yes”, “No” or “I’m not sure”) [99,100,101]. In conclusion, although patients’ overall satisfaction post-TKA is commonly measured using one question with different reply options (binary, 4- or 5-point Likert scales, VAS), this may not accurately assess the reasons behind dissatisfaction. A patient’s overall satisfaction may be affected by the hospital experience, surgical complications, pain reduction, functional improvements and expectation achievements. Therefore, it is recommended to use satisfaction tools that cover each issue in isolation and to elicit responses in more depth in order to understand the impact of each factor on satisfaction [112,116].
Table 7: Characteristics and Results of Patients’ satisfaction studies Post-Total Knee Arthroplasty Studies.
Risk of methodology bias
The overall critical appraisal results varied for each outcome measurement. PROM study scores range from 89% to 57%, PBOMs from 95% to 74%, PA from 85% to 50% and patient satisfaction from 89% to 57%. PROMs studies’ main risks of bias were methods of selection, included patients, randomisation, blindness, not including all subjects in the results without sufficient clarification, ignoring confounding factors in outcome measurements and analyses, and samples mixing different pathologies or interventions. PBOMs studies had less risk of bias and the main limitations concerned randomisation, assessor blindness and similarity of the group baseline. PA studies’ main risk of bias was due to the failure to report the psychometric properties of the accelerometer that was used, insufficient details regarding reported outcomes and how they were measured, not considering confounding factors in the results and analysis, limited follow-up post-TKA, no randomisation, the sample selection not representing the population, no blindness, and not all participants completing follow-up. For all outcomes post-TKA, the majority of studies did not consider confounding factors in their results and analyses, which may affect the generalisation of findings. For example, the presence of a previous chronic condition, PA limitation before surgery, a patient’s age and psychology may affect the outcome post- TKA and should be considered so as to improve the generalisation of outcomes and improve the understanding of affecting factors. The main limitations of patient satisfaction studies lay in their sampling methods, assessor blindness, follow-up being limited to the short and medium term, using non-validated methods to assess satisfaction, and conclusions based on low levels of evidence which might increase the risk of conclusion bias. The overall risk of bias across the studies ranges from low to high, and high-risk findings should be interpreted with caution.
Conclusion and Future Directions
Primary TKA remains the gold standard treatment for patients
with end stage KOA in terms of cost and outcome. The increasing
TKA demand across the globe increases the importance of
understand patient outcomes following procedures. In general,
assessments of PROMs post-TKA focus on function, activity and
participation, with limitations in terms of receiving competent
care from family, neighbours and healthcare workers, and intimate
relationships. In a population younger than 65 years, driving, a
return to work and hobbies are limited in all of them. Function
and environmental assessment depth differ according to the age of
the population post-TKA, as those older than 65 years may require
further assessments of mental and physical endurance. A younger
population needs more in-depth assessment for a return to work,
driving, recreation and sport activity. That may be why there is no
available gold standard that covers all the gaps and is suitable for
broad age requirements post-TKA, with a suitable balance being
struck between complexity and simplicity. Both KOOS and OKS
showed good reliability and validity with a post-TKA population.
Both of them had similar values for a ceiling effect at a 12-month
follow-up. The OKS has the advantage that it is simple and short,
has better reliability scores with TKA patients, clear MIDC values
and clear outcome categories (Table 2). In contrast, KOOS has the
advantage of being more suitable for young patients to assess, in
sufficient depth, function, sport, recreation and knee-related quality
of life. In terms of the quality of items used to assess symptoms and
functional recovery post-TKA, the three commonly used PROMs are
compared in depth in Table 2. Striking a balance between complexity,
the ability to assess items and maintain sufficient measurement
properties is required to achieve comprehensive, valid and reliable
outcomes post-TKA. PBOMs are simple and feasible functional tests
able to capture different aspects of patient function, they differ
from PROMs and do not require any cultural adaptation. They
show excellent to good psychometric properties with a post-TKA
population. Recommended PBOMs are not multi-item, as in real life,
which may affect their ecological validity and leave them prone to
RPE [4,42]. In addition, PROMs assess function, sport, recreation
and knee-related quality of life, with a risk of subjective under/
overestimation. So, inevitably, other measurements are required to
overcome this limitation.
Accelerometers are feasible and environmentally constrained
methods to monitor free-living PA without subjective limitations and
at a reasonable cost when compared to laboratory motion-analysis
technology. There is a conflict regarding accelerometer outcomes
post-TKA, which may be due to many confounding factors, such as
accelerometer measurements not being in a standardized timeline
with regard to the timing of TKA and mixed subjects’ post-knee and
-hip arthroplasty [117,118,119]. In addition, each accelerometer
has different outcomes depending on the study objectives and
accelerometer placement, such as time spent on PA, rest time,
intensity of PA or energy expenditure, which affect the results and
conclusion. Interestingly, no study has explored PA in terms of
volume patterns with a long follow-up of more than one-year post-
TKA to capture the wider picture of PA recovery as is done with
PROMs. No study has assessed the reliability and responsiveness
of the Star Excursion Balance Rest post-TKA, despite its advantage
of closely mimicking PA demand and the history of falling in the
OA population that occurs during dynamic activities rather than in
a static position. No previous study has assessed the sensitivity of
the 30 s chair-stand test and the 40 m fast-paced walk test to detect
changes post-TKA.
Table 8: Individual interview findings of Early Patient concerns following total knee arthroplasty and patient reported outcome measures (n = 30) (Rastogi, Davis, & Chesworth, 2007).
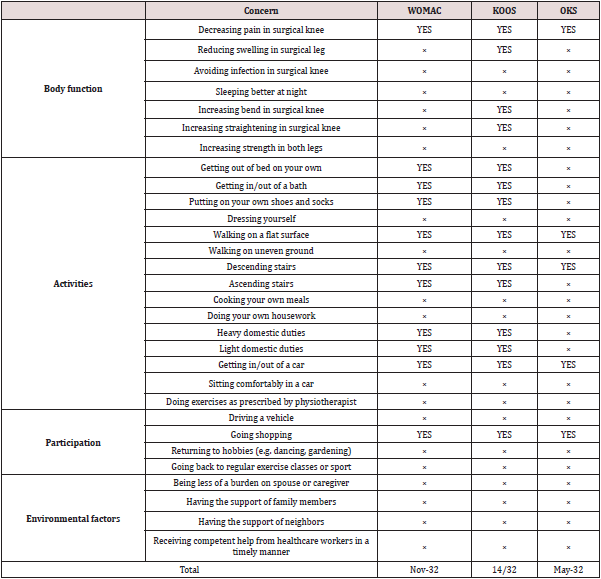
Each outcome measure assesses the outcome post-TKA on a different spectrum. PROMs, PBOMs and accelerometers are valid and reliable tools to evaluate outcomes post-TKA with clear ignorance of personal and environmental factors. These tools’ main concern is solely to quantify body impairments and physical ability, without considering other factors. Therefore, a new tool is recommended to explicate the complexity and deeper meaning of patient experience, concerns, functional recovery, outcome expectations and satisfaction post-TKA. More than half of patients’ early concerns post-TKA are not considered in commonly used PROMs. Individual interviews with 30 patients post-TKA concluded that 32 patient concerns were not covered sufficiently in KOOS, WOMAC or OKS, as shown in Table 8 [120]. This indicates that current medical outcomes evaluation for intervention implications differ from the patient’s perspective. This may be explained by the dissatisfaction of some patients post-TKA. So, more sensitivity to patients’ experience of assessment methods is required, in addition to profession-driven tools to paint a full picture of outcomes post- TKA. Therefore, it is recommended to use satisfaction tools that cover each issue in isolation and to elicit responses in more depth to understand the impact of each factor on satisfaction. The main limitation of the current review is its inability to perform a metaanalysis due to the heterogeneity of outcomes across studies. This limited the ability to derive pooled estimations for effect sizes and, overall, obtain clearer findings for each outcome method. However, the minimal detectable changes concluded for PROMs and PROMs clarify expected outcome changes post-TKA. In conclusion, PROMs play a prominent and feasible role in assessing outcomes post- TKA. However, patient function is multidimensional and requires more than a questionnaire. Therefore, it is recommended to use other objective methods in addition to PROMs, such as PBOMs and accelerometers, to capture the accurate overall recovery picture post-TKA in more depth. Furthermore, future research should seek to assess outcomes post-TKA and devise further interventions aiming to increase the amount of PA engaged in by patients having undergone TKA.
Conflict of interest
This research project received no grants or funding from agencies in the public, commercial, or nonprofit sectors. The author has no financial or personal relationships with other people or organisations that could inappropriately influence (bias) this work. There are no other conflicts of interest to declare.
Acknowledgements
Many thanks to the University of Salford Manchester and Princess Nourah bint Abdul Rahman University for supporting this study.
References
- Heidari B (2011) Knee osteoarthritis prevalence, risk factors, pathogenesis and features: Part I. Caspian J Intern Med 2(2): 205-212.
- Carr A, Robertsson O, Graves S, Price A, Arden N, et al. (2012) Knee replacement. The Lancet 379(9823): 1331-1340.
- Tambascia A, Vasconcelos A, Mello W, Teixeira P, Grossi B (2016) Pre-operative Functional Parameters of Patients Undergoing Total Knee Arthroplasty. Physiotherapy Research International 21(2): 77-83.
- Hossain F, Konan S, Patel S, Rodriguez Merchan E, Haddad F (2015) The assessment of outcome after total knee arthroplasty: are we there yet? Bone Joint J 97-b (1): 3-9.
- Higgins J, Gree S (2011) Cochrane handbook for systematic reviews: Intervention version.
- Giesinger K, Hamilton D, Jost B, Holzner B, Giesinger J (2014) Comparative responsiveness of outcome measures for total knee arthroplasty. Osteoarthritis Cartilage 22(2): 184-189.
- Alnahdi A (2014) Outcome measures capturing ICF domains in patient with total knee arthroplasty. Int J Rehabil Res 37(4): 281-289.
- Alviar M, Olver J, Brand C, Hale T, Khan F (2011) Do patient-reported outcome measures used in assessing outcomes in rehabilitation after hip and knee arthroplasty capture issues relevant to patients? Results of a systematic review and ICF linking process. J Rehabil Med 43(5): 374-381.
- Collins N, Misra D, Felson D, Crossley K, Roos E (2011) Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res (Hoboken) 63 Suppl 11(0 11): S208-228.
- Dowsey M, Choong P (2013) The utility of outcome measures in total knee replacement surgery. Int J Rheumatol pp: 506518.
- Hamilton D, Gaston P, Simpson A (2012) Is patient reporting of physical function accurate following total knee replacement? J Bone Joint Surg Br 94(11): 1506-1510.
- Kauppila A, Kyllonen E, Ohtonen P, Leppilahti J, Sintonen H, et al. (2011) Outcomes of primary total knee arthroplasty: the impact of patient-relevant factors on self-reported function and quality of life. Disabil Rehabil 33(17-18): 1659-1667.
- Khanna G, Singh J, Pomeroy D, Gioe T (2011) Comparison of patient-reported and clinician-assessed outcomes following total knee arthroplasty. J Bone Joint Surg Am 93(20): e117(111)-(117).
- Mizner R, Petterson S, Clements K, Zeni J, Irrgang J, et al. (2011) Measuring functional improvement after total knee arthroplasty requires both performance-based and patient-report assessments: a longitudinal analysis of outcomes. J Arthroplasty 26(5): 728-737.
- Ramkumar P, Harris J, Noble P (2015) Patient-reported outcome measures after total knee arthroplasty: a systematic review. Bone Joint Res 4(7): 120-127.
- Rolfson O, Bohm E, Franklin P, Lyman S, Denissen G, et al. (2016) Patient-reported outcome measures in arthroplasty registries Report of the Patient-Reported Outcome Measures Working Group of the International Society of Arthroplasty Registries Part II. Recommendations for selection, administration, and analysis. Acta Orthop 87 Suppl 1: 9-23.
- Bombardier C, Melfi C, Paul J, Green R, Hawker G, et al. (1995) Comparison of a generic and a disease-specific measure of pain and physical function after knee replacement surgery. Med Care 33(4 Suppl): As131-144.
- Griffiths G, Bellamy N, Bailey W, Bailey S, McLaren A, et al. (1995) A comparative study of the relative efficiency of the WOMAC, AIMS and HAQ instruments in evaluating the outcome of total KNEE arthroplasty. Inflammo Pharmacology 3(1): 1-6.
- Dunbar M, Robertsson O, Ryd L, Lidgren, L (2001) Appropriate questionnaires for knee arthroplasty. Results of a survey of 3600 patients from The Swedish Knee Arthroplasty Registry. J Bone Joint Surg Br 83(3): 339-344.
- Gandek B (2015) Measurement properties of the Western Ontario and McMaster Universities Osteoarthritis Index: a systematic review. Arthritis Care Res (Hoboken) 67(2): 216-229.
- McConnell S, Kolopack P, Davis A M (2001) The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC): a review of its utility and measurement properties. Arthritis Rheum 45(5): 453-461.
- Theiler R, Sangha O, Schaeren S, Michel B, Tyndall A, et al. (1999) Superior responsiveness of the pain and function sections of the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) as compared to the Lequesne-Algofunctional Index in patients with osteoarthritis of the lower extremities. Osteoarthritis Cartilage 7(6): 515-519.
- Escobar A, Quintana J, Bilbao A, Arostegui I, Lafuente I, et al. (2007) Responsiveness and clinically important differences for the WOMAC and SF-36 after total knee replacement. Osteoarthritis Cartilage 15(3): 273-280.
- Bellamy N, Buchanan W, Goldsmith C, Campbell J, Stitt L (1988) Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 15(12): 1833-1840.
- Terwee C, Bot S, de Boer M, van der Windt D, Knol D, et al. (2007) Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 60(1): 34-42.
- Peer M, Lane J (2013) The Knee Injury and Osteoarthritis Outcome Score (KOOS): a review of its psychometric properties in people undergoing total knee arthroplasty. J Orthop Sports Phys Ther 43(1): 20-28.
- Roos E, Roos H, Lohmander L, Ekdahl C, Beynnon B (1998) Knee Injury and Osteoarthritis Outcome Score (KOOS)-development of a self-administered outcome measure. J Orthop Sports Phys Ther 28(2): 88-96.
- Roos E (2003) Effectiveness and practice variation of rehabilitation after joint replacement. Curr Opin Rheumatol 15(2): 160-162.
- Sasaki E, Tsuda E, Yamamoto Y, Meada S, Otsuka H, et al. (2014) Relationship between patient-based outcome score and conventional objective outcome scales in post-operative total knee arthroplasty patients. Int Orthop 38(2): 373-378.
- Davis A, Perruccio A, Canizares M, Hawker G, Roos E, et al. (2009) Comparative, validity and responsiveness of the HOOS-PS and KOOS-PS to the WOMAC physical function subscale in total joint replacement for osteoarthritis. Osteoarthritis Cartilage 17(7): 843-847.
- Lyman S, Lee Y, McLawhorn A, Islam W, Maclean C (2018) What Are the Minimal and Substantial Improvements in the HOOS and KOOS and JR Versions After Total Joint Replacement? Clinical orthopaedics and related research 476(12): 2432-2441.
- Dawson J, Fitzpatrick R, Murray D, Carr A (1998) Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br 80(1): 63-69.
- Murray D, Fitzpatrick R, Rogers K, Pandit H, Beard D, et al. (2007) The use of the Oxford hip and knee scores. J Bone Joint Surg Br 89(8): 1010-1014.
- Beard D, Harris K, Dawson J, Doll H, Murray D, et al. (2015) Meaningful changes for the Oxford hip and knee scores after joint replacement surgery. J Clin Epidemiol 68(1): 73-79.
- Clement N, MacDonald D, Patton J, Burnett R (2015) Post-operative Oxford knee score can be used to indicate whether patient expectations have been achieved after primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 23(6): 1578-1590.
- Clement N D, MacDonald D, Simpson A H (2014) The minimal clinically important difference in the Oxford knee score and Short Form 12 score after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc, 22(8): 1933-1939.
- Gen L, Bin Abd Razak H, Chi C, Chye T (2015) No Gender-Based Differences in Outcomes after Conventional Total Knee Arthroplasty in Asians. J Arthroplasty 30(9): 1548-1550.
- Judge A, Arden N, Kiran A, Price A, Javaid M, et al (2012) Interpretation of patient-reported outcomes for hip and knee replacement surgery: identification of thresholds associated with satisfaction with surgery. J Bone Joint Surg Br 94(3): 412-418.
- Marx R, Jones E, Atwan N, Closkey R, Salvati E, et al. (2005) Measuring improvement following total hip and knee arthroplasty using patient-based measures of outcome. J Bone Joint Surg Am 87(9): 1999-2005.
- Matharu G, McBryde C, Robb C, Pynsent P (2014) An analysis of Oxford hip and knee scores following primary hip and knee replacement performed at a specialist centre. Bone Joint J 96-B (7): 928-935.
- Harris K, Dawson J, Doll H, Field R, Murray D, et al. (2013) Can pain and function be distinguished in the Oxford Knee Score in a meaningful way? An exploratory and confirmatory factor analysis. Qual Life Res 22(9): 2561-2568.
- McCambridge J, Witton J, Elbourne D (2014) Systematic review of the Hawthorne effect: new concepts are needed to study research participation effects. J Clin Epidemiol 67(3): 267-277.
- Thumboo J, Chew L, Lewin Koh S (2002) Socioeconomic and psychosocial factors influence pain or physical function in Asian patients with knee or hip osteoarthritis. Ann Rheum Dis 61(11): 1017-1020.
- Bolink S, van Laarhoven S, Lipperts M, Heyligers I, Grimm B (2012) Inertial sensor motion analysis of gait, sit-stand transfers and step-up transfers: differentiating knee patients from healthy controls. Physiol Meas 33(11): 1947-1958.
- Jacobs C, Christensen C (2009) Correlations between knee society function scores and functional force measures. Clin Orthop Relat Res 467(9): 2414-2419.
- Wiik A, Manning V, Strachan R, Amis A, Cobb J (2013) Unicompartmental knee arthroplasty enables near normal gait at higher speeds, unlike total knee arthroplasty. J Arthroplasty 28(9 Suppl): 176-178.
- Skoffer B, Dalgas U, Mechlenburg I, Soballe K, Maribo T (2015) Functional performance is associated with both knee extensor and flexor muscle strength in patients scheduled for total knee arthroplasty: A cross-sectional study. J Rehabil Med 47(5): 454-459.
- Mark Christensen T, Kehlet H (2019) Assessment of functional recovery after total hip and knee arthroplasty: An observational study of 95 patients. Musculoskeletal Care 17(4): 300-312.
- Naili J, Iversen M, Esbjornsson A, Hedström M, Schwartz M, et al. (2016) Deficits in functional performance and gait one year after total knee arthroplasty despite improved self-reported function. Knee Surg Sports Traumatol Arthrosc 25(11).
- Aalund P, Larsen K, Hansen T, Bandholm T (2013) Normalized knee-extension strength or leg-press power after fast-track total knee arthroplasty: which measure is most closely associated with performance-based and self-reported function? Arch Phys Med Rehabil 94(2): 384-390.
- Stevens Lapsley J E, Schenkman M L, Dayton M R (2011) Comparison of self-reported knee injury and osteoarthritis outcome score to performance measures in patients after total knee arthroplasty. Pm r 3(6): 541-549; quiz 549.
- Kennedy D, Stratford P, Wessel J, Gollish J, Penney D (2005) Assessing stability and change of four performance measures: a longitudinal study evaluating outcome following total hip and knee arthroplasty. BMC Musculoskelet Disord 6(3).
- Boonstra M C, De Waal Malefijt M C, Verdonschot N (2008) How to quantify knee function after total knee arthroplasty? Knee 15(5): 390-395.
- Almeida G, Schroeder C, Gil A, Fitzgerald G, Piva S R (2010) Interrater reliability and validity of the stair ascend/descend test in subjects with total knee arthroplasty. Arch Phys Med Rehabil 91(6): 932-938.
- Hossain F, Patel S, Fernandez M, Konan S, Haddad F (2013) A performance-based patient outcome score for active patients following total knee arthroplasty. Osteoarthritis Cartilage 21(1): 51-59.
- Unver B, Kalkan S, Yuksel E, Kahraman T, Karatosun V (2015) Reliability of the 50-foot walk test and 30-sec chair stand test in total knee arthroplasty. Acta Ortop Bras 23(4): 184-187.
- Naylor J, Mills K, Buhagiar M, Fortunato R, Wright R (2016) Minimal important improvement thresholds for the six-minute walk test in a knee arthroplasty cohort: triangulation of anchor- and distribution-based methods. BMC Musculoskelet Disord 17(1): 390.
- Dobson F, Hinman R, Roos E, Abbott J, Stratford P, et al. (2013) OARSI recommended performance-based tests to assess physical function in people diagnosed with hip or knee osteoarthritis. Osteoarthritis Cartilage 21(8): 1042-1052.
- Kauppila A, Kyllonen E, Mikkonen P, Ohtonen P, Laine V, et al. (2009) Disability in end-stage knee osteoarthritis. Disabil Rehabil 31(5): 370-380.
- Zasadzka E, Borowicz A, Roszak M, Pawlaczyk M (2015) Assessment of the risk of falling with the use of timed up and go test in the elderly with lower extremity osteoarthritis. Clin Interv Aging 10: 1289-1298.
- Hinman R, Bennell K, Metcalf B, Crossley K (2002) Balance impairments in individuals with symptomatic knee osteoarthritis: a comparison with matched controls using clinical tests. Rheumatology 41(12): 1388-1394.
- Hinman R, Heywood S, Day A (2007) Aquatic physical therapy for hip and knee osteoarthritis: results of a single-blind randomized controlled trial. Phys Ther 87(1): 32-43.
- Lim B, Hinman R, Wrigley T, Sharma L, Bennell K (2008) Does knee malalignment mediate the effects of quadriceps strengthening on knee adduction moment, pain, and function in medial knee osteoarthritis? A randomized controlled trial. Arthritis Rheum 59(7): 943-951.
- Coughlan G, Fullam K, Delahunt E, Gissane C, Caulfield B (2012) A comparison between performance on selected directions of the star excursion balance test and the Y balance test. J Athl Train 47(4): 366-371.
- Fullam K, Caulfield B, Coughlan G, Delahunt E (2014) Kinematic analysis of selected reach directions of the Star Excursion Balance Test compared with the Y-Balance Test. J Sport Rehabil 23(1): 27-35.
- Kanko L, Birmingham T, Bryant D, Gillanders K, Lemmon K, et al. (2019) The star excursion balance test is a reliable and valid outcome measure for patients with knee osteoarthritis. Osteoarthritis Cartilage 27(4): 580-585.
- Al Khlaifat L, Herrington L, Tyson S, Hammond A, Jones R (2016) The effectiveness of an exercise programme on dynamic balance in patients with medial knee osteoarthritis: A pilot study. Knee 23(5): 849-856.
- (2020) World Health Organization Global Strategy on Diet, Physical Activity and Health.
- Abbasi Bafghi H, Fallah Yakhdani H R, Meijer O G, de Vet H, Bruijn S, et al. (2012) The effects of knee arthroplasty on walking speed: a meta-analysis. BMC Musculoskelet Disord 13: 66.
- Hatfield G L, Stanish W D, Hubley Kozey C L (2015) Three-dimensional biomechanical gait characteristics at baseline are associated with progression to total knee arthroplasty. Arthritis Care Res (Hoboken) 67(7): 1004-1014.
- Agarwal V, Smuck M, Shah N H (2017) Quantifying the relative change in physical activity after Total Knee Arthroplasty using accelerometer-based measurements. AMIA Joint Summits on Translational Science proceedings. AMIA Joint Summits on Translational Science 463-472.
- Lutzner C, Kirschner S, Lutzner J (2014) Patient activity after TKA depends on patient-specific parameters. Clin Orthop Relat Res 472(12): 3933-3940.
- Meiring R, Frimpong E, Mokete L, Pietrzak J, Van Der Jagt D, et al. (2016) Rationale, design and protocol of a longitudinal study assessing the effect of total knee arthroplasty on habitual physical activity and sedentary behaviour in adults with osteoarthritis. BMC Musculoskelet Disord 17: 281.
- Bin sheeha B, Granat M, Williams A, Johnson D, Jones R (2020) Does free-living physical activity improve one-year following total knee arthroplasty in patients with osteoarthritis: A prospective study. Osteoarthritis and Cartilage Open 100065.
- Harding P, Holland A, Delany C, Hinman R (2014) Do activity levels increase after total hip and knee arthroplasty? Clin Orthop Relat Res 472(5): 1502-1511.
- Kahn T, Schwarzkopf R (2015) Does Total Knee Arthroplasty Affect Physical Activity Levels? Data from the Osteoarthritis Initiative. J Arthroplasty 30(9): 1521-1525.
- Frimpong E, McVeigh J A, van der Jagt D, Mokete L, Kaoje Y, et al. (2019) Light intensity physical activity increases and sedentary behavior decreases following total knee arthroplasty in patients with osteoarthritis. Knee Surg Sports Traumatol Arthrosc 27: 2196-2205.
- Brandes M, Ringling M, Winter C, Hillmann A, Rosenbaum D (2011) Changes in physical activity and health-related quality of life during the first year after total knee arthroplasty. Arthritis Care Res (Hoboken) 63(3): 328‐334.
- Robertson N, Battenberg A, Kertzner M, Schmalzried T (2016) Defining high activity in arthroplasty patients. Bone Joint J 98-b (1 Suppl A): 95-97.
- De Groot I B, Bussmann H J, Stam H J, Verhaar J (2008) Small increase of actual physical activity 6 months after total hip or knee arthroplasty. Clinical orthopaedics and related research 466(9): 2201-2208.
- Vissers M, Bussmann J, De Groot I, Verhaar J, Reijman M (2013) Physical functioning four years after total hip and knee arthroplasty. Gait Posture 38(2): 310-315.
- Wimmer M, Nechtow W, Schwenke T, Moisio K (2015) Knee Flexion and Daily Activities in Patients following Total Knee Replacement: A Comparison with ISO Standard 14243. Biomed Res Int 157541.
- Granat M (2012) Event-based analysis of free-living behaviour. Physiol Meas 33(11): 1785-1800.
- Grant P, Ryan C, Tigbe W, Granat M (2006) The validation of a novel activity monitor in the measurement of posture and motion during everyday activities. Br J Sports Med 40(12): 992-997.
- Hamilton D F, Lane J V, Gaston P, Patton J, Macdonald D, et al. (2013) What determines patient satisfaction with surgery? A prospective cohort study of 4709 patients following total joint replacement. BMJ Open 3(4).
- Klit J, Jacobsen S, Rosenlund S, Sonne Holm S, Troelsen A (2014) Total knee arthroplasty in younger patients evaluated by alternative outcome measures. J Arthroplasty 29(5): 912-917.
- Neuprez A, Delcour J, Fatemi F, Gillet P, Crielaard J, et al. (2016) Patients' Expectations Impact Their Satisfaction following Total Hip or Knee Arthroplasty. PLoS One 11(12): e0167911.
- Noble P, Conditt M, Cook K, Mathis K (2006) The John Insall Award: Patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res 452: 35-43.
- Scott C, Howie C, MacDonald D, Biant L (2010) Predicting dissatisfaction following total knee replacement: a prospective study of 1217 patients. J Bone Joint Surg Br 92(9): 1253-1258.
- Lizaur Utrilla A, Martinez Mendez D, Miralles Munoz F, Marco Gomez L, Lopez Prats F (2016) Negative impact of waiting time for primary total knee arthroplasty on satisfaction and patient-reported outcome. Int Orthop 40(11): 2303-2307.
- Ozdemir M, Demirkale I, Sesen H, Taskesen A, Okkaoglu M, Altay M (2017) Affective temperament does not influence satisfaction after total knee arthroplasty. Medicine (Baltimore) 96(19): e6852.
- Clement N, MacDonald D, Patton J, Burnett R (2015) Post-operative Oxford knee score can be used to indicate whether patient expectations have been achieved after primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 23(6): 1578-1590.
- Kim T, Kwon S, Kang Y, Chang C, Seong S (2010) Functional disabilities and satisfaction after total knee arthroplasty in female Asian patients. J Arthroplasty 25(3): 458-464.e451-452.
- Halawi M, Jongbloed W, Baron S, Savoy L, Williams V, Cote M (2019) Patient Dissatisfaction After Primary Total Joint Arthroplasty: The Patient Perspective. J Arthroplasty 34(6): 1093-1096.
- Furu M, Ito H, Nishikawa T, Nankaku M, Kuriyama S, et al. (2016) Quadriceps strength affects patient satisfaction after total knee arthroplasty. J Orthop Sci 21(1): 38-43.
- Deakin A H, Iyayi Igbinovia A, Love G J (2018) A comparison of outcomes in morbidly obese, obese and non-obese patients undergoing primary total knee and total hip arthroplasty. Surgeon 16(1): 40-45.
- Culliton S, Bryant D, Overend T, MacDonald S, Chesworth B (2012) The relationship between expectations and satisfaction in patients undergoing primary total knee arthroplasty. J Arthroplasty 27(3): 490-492.
- Clement N D, Burnett R (2013) Patient satisfaction after total knee arthroplasty is affected by their general physical well-being. Knee Surg Sports Traumatol Arthrosc 21(11): 2638-2646.
- Williams D, O Brien S, Doran E, Price A, Beard D, et al. (2013) Early postoperative predictors of satisfaction following total knee arthroplasty. Knee 20(6): 442-446.
- Jacobs C A, Christensen C P, Karthikeyan T (2014) Patient and intraoperative factors influencing satisfaction two to five years after primary total knee arthroplasty. J Arthroplasty 29(8): 1576-1579.
- Goudie S, Deakin A, Ahmad A, Maheshwari R, Picard F (2011) Flexion contracture following primary total knee arthroplasty: risk factors and outcomes. Orthopedics 34(12): e855-859.
- Collados Maestre I, Lizaur Utrilla A, Martinez Mendez D, Marco Gomez L, Lopez Prats F (2016) Concomitant low back pain impairs outcomes after primary total knee arthroplasty in patients over 65 years: a prospective, matched cohort study. Arch Orthop Trauma Surg 136(12): 1767-1771.
- Sauder N, Galea V, Rojanasopondist P, Colon Iban Y, Florissi I, et al. (2019) Regional differences between the US, Scandinavia, and South Korea in patient demographics and patient-reported outcomes for primary total knee arthroplasty. Arch Orthop Trauma Surg.
- Jacobs C A, Christensen C P (2014) Factors influencing patient satisfaction two to five years after primary total knee arthroplasty. J Arthroplasty 29(6): 1189-1191.
- Nakahara H, Okazaki K, Mizu Uchi H, Hamai S, Tashiro Y, et al. (2015) Correlations between patient satisfaction and ability to perform daily activities after total knee arthroplasty: why aren't patients satisfied? J Orthop Sci 20(1): 87-92.
- Goh G, Liow M, Bin Abd Razak H, Tay D, Lo N, et al. (2017) Patient-Reported Outcomes, Quality of Life, and Satisfaction Rates in Young Patients Aged 50 Years or Younger After Total Knee Arthroplasty. J Arthroplasty 32(2): 419-425.
- Ha C, Park Y, Song Y, Kim J, Park Y (2016) Increased Range of Motion Is Important for Functional Outcome and Satisfaction After Total Knee Arthroplasty in Asian Patients. J Arthroplasty 31(6): 1199-1203.
- Benditz A, Maderbacher G, Zeman F, Grifka J, Weber M, et al. (2017) Postoperative pain and patient satisfaction are not influenced by daytime and duration of knee and hip arthroplasty: a prospective cohort study. Arch Orthop Trauma Surg 137(10): 1343-1348.
- Clement N, Walker L, Bardgett M, Weir D, Holland J, et al. (2018) Patient age of less than 55 years is not an independent predictor of functional improvement or satisfaction after total knee arthroplasty. Arch Orthop Trauma Surg 138(12): 1755-1763.
- Kunze K, Akram F, Fuller B, Zabawa L, Sporer S, Levine B (2019) Internal Validation of a Predictive Model for Satisfaction After Primary Total Knee Arthroplasty. J Arthroplasty 34(4): 663-670.
- Van Onsem S, Van Der Straeten C, Arnout N, Deprez P, Van Damme G, et al. (2016) A New Prediction Model for Patient Satisfaction After Total Knee Arthroplasty. J Arthroplasty 31(12): 2660-2667.e2661.
- Al Omran A S (2014) The Quality of Life (QOL) after Total Knee Arthroplasties among Saudi Arabians: A Pilot Study. Int J Biomed Sci 10(3): 196-200.
- Thambiah M, Nathan S, Seow B, Liang S, Lingaraj K (2015) Patient satisfaction after total knee arthroplasty: an Asian perspective. Singapore Med J 56(5): 259-263.
- Loth F, Giesinger J, Giesinger K, Howie C, Hamilton D (2019) Single-item satisfaction scores mask large variations in pain, function and joint awareness in patients following total joint arthroplasty. Eur J Orthop Surg Traumatol 30(2): 267-274.
- Shannak O, Palan J, Esler C (2017) A regional registry study of 216 patients investigating if patient satisfaction after total knee arthroplasty changes over a time period of five to 20years. Knee 24(4): 824-828.
- Harland N J, Dawkin M J, Martin D (2015) Relative utility of a visual analogue scale vs. a six-point Likert scale in the measurement of global subject outcome in patients with low back pain receiving physiotherapy. Physiotherapy101(1): 50-54.
- Mills K, Falchi B, Duckett C, Naylor J (2019) Minimal change in physical activity after lower limb joint arthroplasty, but the outcome measure may be contributing to the problem: a systematic review and meta-analysis. Physiotherapy 105(1): 35‐45.
- Paxton R, Melanson E, Stevens Lapsley J, Christiansen C (2015) Physical activity after total knee arthroplasty: A critical review. World J Orthop 6(8): 614-622.
- Arnold J B, Walters J L, Ferrar K E (2016) Does Physical Activity Increase After Total Hip or Knee Arthroplasty for Osteoarthritis? A Systematic Review. J Orthop Sports Phys Ther 46(6): 431-442.
- Rastogi R, Davis A, Chesworth B (2007) A cross-sectional look at patient concerns in the first six weeks following primary total knee arthroplasty. Health Qual Life Outcomes 5: 48.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...