Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2638-6003
Research Article(ISSN: 2638-6003) 
Caring for the Professional Basketball Athlete: A Conceptual Framework Volume 5 - Issue 4
Brian Serrano*, D.C., Ph.D., CCSP, ATC, CSCS
- Performance Health Coordinator, Windy City Bulls, USA
Received: November 16, 2021 Published: November 24, 2021
Corresponding author: Brian Serrano, Performance Health Coordinator, Windy City Bulls, USA
DOI: 10.32474/OSMOAJ.2021.05.000219
Abstract
Purpose: The professional basketball player presents a unique challenge that must be approached with a conceptual lens
between the sports medicine and sports performance staff.
Methods: The author used a combination of subjective and objective methods to determine the primary clinicians on the sports
medicine staff. The sports performance staff was also investigated using the standards set forth by respective organizations such
as the NSCA. Lastly, data and frameworks were combined to come up with a new integrative algorithm in caring for these specific
athletes.
Results/Conclusion: Results indicated the sports medicine staff consists primarily of physician, athletic trainers, and physical
therapists. The sports performance staff consists of a strength and conditioning specialists (CSCS), obtained through the NSCA.
The key components of the conceptual framework were Communication, Collaboration, and being open to Feedback for optimal
performance healthcare.
Applications to sport: The professional basketball athlete invests time, money, and energy into their career. Similarly,
organizations/teams are continually looking for ways to increase the standard of care for their athletes, especially with the amount
of investment trending into millions of dollars. Through seamless integration and constant communication, the sports medicine and
performance staff can create a novel, better framework in caring for their athletes.
Keywords: Sports Medicine; Sports Performance; Athletic Training; Strength; Conditioning
Introduction
The world of professional basketball has evolved over the last 50 years to become its own industry [1]. The industry of professional sports has become lucrative and generates millions of dollars per year [2]. This income generating industry has rightfully spread to its athletes, who are now worth tens or hundreds of millions of dollars [3]. Similarly, this has also spread into the sports medicine and sports performance staff [4]. The sports medicine and performance staffs in professional sport have evolved from being largely singular and unidimensional, to multi-disciplinary and multidimensional team [5]. The sports medicine staff has evolved from having primarily one certified athletic trainer (ATC) to now having multiple Athletic Trainers along with other types of clinicians [5]. The field of sports performance has evolved from experience-based coached to becoming recognized via national level certifications such as the NSCA (National Strength and Conditioning Association) and their CSCS (Certified Strength and Conditioning Specialist [6,7]. However, for the growth each respective field had experienced, they still exist in silos or a rudimentary form of integration. As clinicians and practitioners within the realm of sports medicine and performance, we must strive to provide the highest standard of care to our athletes. The professional basketball athlete is no different and thus, this paper seeks to put forth a new conceptual framework in making this happen.
Sports Medicine
The field of sports medicine has experienced a tremendous amount of growth that is evident by the expansion of degree options, as well as types of clinicians being employed in the professional basketball setting [8,9]. The early beginnings of sports medicine saw the mainstay of the team consisting of one physician and one athletic trainer. The role of the physician was to function as the leader of the team while the athletic trainer handled the day-to-day operations and medical care of the players within the organization [10]. We now see athletic trainers taking on expanded roles due to increased education and experiences [11]. Along with the addition of other health care providers such as physical therapists, chiropractors, and massage therapists. For example, physical therapists now have a role in corrective exercise and post-operative rehabilitation in athlete care [12]. Chiropractors have also seen expanded roles in their contribution to the sports medicine staff through manual therapy, spinal, and joint manipulation/mobilization [13]. Lastly, massage therapists have emerged as experts within the field of manual therapy in performance healthcare [14]. For athletic trainers specifically, the transition into the entry-level master’s and increased recognition of the DAT (Doctor of Athletic Training) degree means AT’s can now function as the team captain of the medical team and direct athletes in where to receive their care [15].
Sports Performance
The field of strength and conditioning has largely been influenced by organizations like the NSCA (National Strength and Conditioning Association) and the CSCS certification [16,17]. Beyond this, the standard in education to coach at the professional level is having a master’s degree [18]. The role of the strength and conditioning coach has evolved drastically over the last 2 decades [19]. For example, the role used to primarily involve coaching and cueing exercises. Now, strength and conditioning coaches still have the foundational responsibility of teaching proper exercise form with the additional duties of programming and even delving into sport science [20,22]. Although the field of sport science is and should be respected as its own field because of its complexities into epidemiology, biostatics, and biomechanics among other things [23]. It should also be pointed out that strength and conditioning coaches are increasingly being asked and expected to fill these roles depending on the structure and resources of the team/ organization. These responsibilities can range from subjective readiness questionaries to more complex full athlete profiles [24].
The Current State of Sports Medicine and Performance
As we can see from a macroscopic view, the field of sports medicine and performance is naturally intertwined and becomes more so as the value of athletes increases, and every aspect of their performance become increasingly scrutinized by both internal and external stakeholders [25]. With this information, one would imagine that both staffs are very integrated and function as one team. However, this is the exception and not the rule. Although, there has been a positive trend in this direction where athletic trainers, physical therapists, and strength and conditioning coaches discuss ideas and treatment plans for their athletes, there is still a large gap [26]. For example, the usual high performance medical model consists of the following. The athletic trainer refers an athlete to the team physician who then performs their assessment, requests imaging, and comes up with a diagnosis and treatment plan. The treatment plan is then carried out by the athletic trainer in the sense of manual therapy/modalities, then early-stage rehab exercises with the physical therapist, and then the late-stage rehab (return to play) by the strength and conditioning coach [27,28]. While this model can be effective, it focuses on dichotomous progressions where the practitioner can feel underutilized and the athlete lacking a continuity of care. In this paper, the author proposes using a combination of clinical experience and best practice guidelines a new high-performance clinical model.
Methods
The High-Performance HealthCare Model
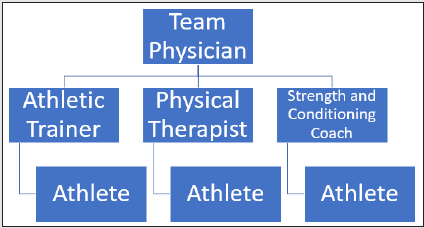
The High-Performance HealthCare Model has evolved over the last 10 years thanks to the enormous contribution of organizations such as the United States Olympic and Paralympic Committee (USOPC) [29,30]. The USOPC works in a multi-disciplinary model that includes various clinicians such as sports medicine physicians, physical therapists, athletic trainers, and strength and conditioning coaches working together [29,30]. Professional organizations have been quick to adapt to this model such as in Baseball (MLB) and Football (NFL) where athlete care is led by a medical director and then handed off to the appropriate practitioner depending on where the athlete is in their return to play process [4]. Due to the initial success of this model, you can see integrated sports medicine and performance model also incorporated into collegiate athletics. As is usually true, Division 1 schools were the first to adopt then into Division 2 and 3 [31]. While this model has many positive aspects as investigated by clinical outcomes papers, there are some drawbacks to this approach. Some drawbacks include a lack on direct continuity, a dichotomous field of thinking, and being siloed into a specific profession. The biggest drawback to this approach is the same athlete being viewed a different entity be each practitioner (Figure 1).
The Multi-Disciplinary Model
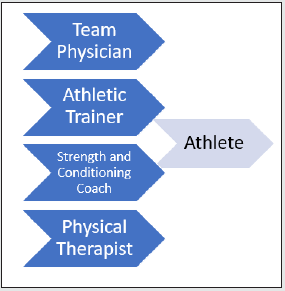
Recently, because of the success of the High-Performance Healthcare Model (HPHM), there was a derivative in the form of the Multi-Disciplinary Model [32,33]. This model draws on the strength of having multiple practitioners within one organization and brings their ideas together [34,35]. For example, a multi-disciplinary team may consist of clinicians such as: physicians, chiropractors, physical therapists, athletic trainers, and strength and conditioning coaches. Using the example of a post-surgical athlete striving to return to performance [35]. This would begin with the physician setting early healing and rehabilitation guidelines for the staff to use. The physical therapist would work with the athlete performing basic range of motion and manual therapy in this stage. The athletic trainer would then take over with pain relieving modalities and continue to work on gaining full range of motion and working on basic strength. Once the athlete has regained full range of motion and has a functional level of muscular strength and endurance, they get handed off to the strength and conditioning coach [36]. The role of the strength and conditioning role in this model is to prepare the athlete for return to unrestricted sport. While this model as previously stated has a great foundation in taking the perspectives and expertise of various practitioners, it still lacks true integration. Instead, this model seems to propose a timeline where after a certain criterion is met, the work of that clinician is finished. For example, after the acute healing phase the physical therapist has completed working with the athlete (Figure 2).
Results
A Novel Integrated Approach
This novel way to care for the professional basketball athlete combine and considers the shortcomings of previous medical models. In this model, each clinician and practitioner will have a continual involvement in the well-being of the athlete in their road to performance [37,38]. This continuum approach has several advantages from both an internal and external standpoint. From an internal standpoint, being able to consult and discuss ideas can be a valuable learning experience and promote inter-professional learning [39]. From an external standpoint, each stakeholder is directly involved in athlete progress from day one which is much different than previous models. For example, the strength and conditioning coach knows the type of injury/surgery the athlete has received, and the type of acute activities being performed. This sets a better foundational understanding and appreciation for the coach as the athlete will reach them later in the return to performance spectrum (Figure 3).
Discussion
The field of sports medicine and performance continues to involve every day, with the roles of clinicians and practitioners becoming more specialized and overlapped more than ever34,36. In professional Basketball, this becomes more prominent as members of the staff at this level must be able to possess abilities much higher than their respective license/certification. For example, physical therapists must be great at rehabilitation, but also have at least an intermediate understand of strength and conditioning principles. Similarly, the athletic trainer must be great in in their clinical evaluation and diagnosis skills while being able to possess manual therapy skills [40]. Just as important, even though the field of sport science is its own, strength and conditioning coaches are increasingly expected to be proficient at capturing and interpreting data for coaches and front office staff [20,21]. These changes in the field are only elevated at the professional level for aspiring practitioners looking to work in this setting. As mentioned previously, the push for elevated education across the medical and performance sector has seen a higher standard of care for athletes. This has been seen first in the physical therapist profession going from master to doctorate and most recently the athletic training transition to the entry-level masters [41,42]. The strength and conditioning certification can be obtained through an undergraduate degree but the standard in the professional and collegiate athletic level is to be CSCS certified with a master’s degree. Furthermore, the construct of this novel approach allows better communication between all member of the staff. For example, instead of getting bits and pieces of information from each practitioner regarding athlete progression/status. This new model allows full communication from the time injury occurs or the athlete comes out of surgery. By incorporating this model of performance care, a higher standard of care and faster return to performance can be possible.
Conclusions
This paper explores the preciseness of performance healthcare within the sport of Basketball. Basketball is a unique sport because its total roster size is relatively small which allows for rapport building and establish a great professional relationship. From an objective standpoint, the coordination of care is also challenged by the number of practitioners and thus biases present within a staff. However, as with any professional sport, the amount of external and internal stakeholders grows making keeping everyone abreast of pertinent information difficult. Once stressors like travel, poor sleep, and game density are accounted for in professional basketball, caring for the athlete becomes a challenging task. This new model proposed by the author allows full integration between the medical and performance staff through better communication, practitioner relationships, and direct involvement.
Applications in Sport
The landscape of professional basketball is trending towards larger medical and performance staffs, more stakeholders, and higher amount of total revenue. This presents a monumental challenge to the people charged with keeping its athletes healthy. However, through using an overlapping approach where each respective practitioner has all information regarding athlete status and is directly involved in its decision-making process. This will be a more effective model of performance healthcare for the professional basketball athlete.
References
- Ann Scheck McAlearney, Julie Robbins, Andrew N Garman, Paula H Song (2013) Implementing high-performance work practices in healthcare organizations: qualitative and conceptual evidence. Journal of Healthcare Management 58(6): 446-462.
- Antonietti R [2006] Human Capital, Sports Performance and Salary Determination of Professional Athletes. SSRN Electronic Journal.
- Dietl HM, Franck E, Lang M, Rathke A [2012] SALARY CAP REGULATION IN PROFESSIONAL TEAM SPORTS. Contemporary Economic Policy 30(3): 307-319.
- Romero MG, Pitney WA, Brumels K, Mazerolle SM [2018] Role Strain, Part 1: Experiences of Athletic Trainers Employed in the Professional Sports Setting. Journal of Athletic Training 53(2):184-189.
- Diakogeorgiou E, Ray RR, Brown S, Hertel J, Casa DJ [2021] The Evolution of the Athletic Training Profession. Kinesiology Review 10(3): 308-318.
- Simenz CJ, Dugan CA, Ebben WP [2005] STRENGTH AND CONDITIONING PRACTICES OF NATIONAL BASKETBALL ASSOCIATION STRENGTH AND CONDITIONING COACHES. Journal of Strength and Conditioning Research 19(3): 495-504.
- Ebben WP, Blackard DO (2001) Strength and Conditioning Practices of National Football League Strength and Conditioning Coaches. Journal of Strength and Conditioning Research 15(1): 48-58.
- Lakshmi SN, Narisetti S, Lakshmi B, Narisetti S (2020) Sports medicine market-growth factors and forecasts 7(1): 117-128.
- Sports Medicine Today on JSTOR. Accessed November 11 2021.
- Brumels K, Beach A (2008) Professional Role Complexity and Job Satisfaction of Collegiate Certified Athletic Trainers. Journal of Athletic Training 43(4): 373-378.
- Delforge GD, Behnke RS (1999) The History and Evolution of Athletic Training Education in the United States. Journal of Athletic Training 34(1): 53.
- Furze JA, Tichenor CJ, Fisher BE, et al. (2016) Physical Therapy Residency and Fellowship Education: Reflections on the Past, Present, and Future. Physical Therapy 96(7): 949-960.
- Sports Chiropractic in Canada-ProQuest. Accessed November 11 2021.
- Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ (2009) The mechanisms of manual therapy in the treatment of musculoskeletal pain: A comprehensive model. Manual Therapy 14(5): 531-538.
- van Lunen BL, Clines SH, Reems T, Eberman LE, Hankemeier DA, et al. (2021) Employability in Academe for Athletic Trainers with the Doctor of Athletic Training Degree. Journal of Athletic Training. 56(3): 220-226.
- SURVEY: Does being C.S.C.S.-certified make a difference? : Strength & Conditioning Journal. Accessed November 11 2021.
- THE NATIONAL STRENGTH AND CONDITIONING ASSOCIATION IS THE PREFERRED CERTIFICATION FOR PERSONAL TRAINING EMPLOYMENT IN SOUTHEASTERN MASSACHUSETTS - ProQuest. Accessed November 11, 2021.
- Dorgo S (2009) Unfolding the Practical Knowledge of an Expert Strength and Conditioning Coach: 4(1): 17-30.
- Tod DA, Bond KA, Lavallee D (2012) Professional development themes in strength and conditioning coaches. Journal of Strength and Conditioning Research 26(3): 851-860.
- Bourdon PC, Cardinale M, Murray A, et al. (2017) Monitoring Athlete Training Loads: Consensus Statement. International Journal of Sports Physiology and Performance 12(s2): S2-161.
- Gabbett TJ, Nassis GP, Oetter E, et al. (2017) The athlete monitoring cycle: a practical guide to interpreting and applying training monitoring data. British Journal of Sports Medicine 51(20): 1451-1452.
- Seshadri DR, Li RT, Voos JE, et al. (2019) Wearable sensors for monitoring the internal and external workload of the athlete. npj Digital Medicine 2(1): 1-18.
- Fullagar HHK, McCall A, Impellizzeri FM, Favero T, Coutts AJ (2019) The Translation of Sport Science Research to the Field: A Current Opinion and Overview on the Perceptions of Practitioners, Researchers and Coaches. Sports Medicine 49(12):1817-1824.
- Shurley JP, Todd JS, Todd TC (2017) The science of strength: Reflections on the national strength and conditioning association and the emergence of research-based strength and conditioning. Journal of Strength and Conditioning Research 31(2): 517-530.
- Woods CT, McKeown I, O’Sullivan M, Robertson S, Davids K (2020) Theory to Practice: Performance Preparation Models in Contemporary High-Level Sport Guided by an Ecological Dynamics Framework. Sports Medicine-Open 6(1): 1-11.
- Tod DA, Bond KA, Lavallee D (2012) Professional development themes in strength and conditioning coaches. Journal of Strength and Conditioning Research 26(3): 851-860.
- Taberner M, Allen T, Cohen DD (2019) Progressing rehabilitation after injury: consider the ‘control-chaos continuum.’ British Journal of Sports Medicine 53(18): 1132-1136.
- Buckthorpe M, Frizziero A, Roi GS (2019) Update on functional recovery process for the injured athlete: return to sport continuum redefined. British Journal of Sports Medicine 53(5): 265-267.
- Wiese-bjornstal DM, Smith AM, Shaffer SM, Morrey MA (2008) An integrated model of response to sport injury: Psychological and sociological dynamics 10(1): 46-69.
- Dijkstra HP, Pollock N, Chakraverty R, Alonso JM (2014) Managing the health of the elite athlete: a new integrated performance health management and coaching model. British Journal of Sports Medicine. 48(7): 523-531.
- Goodman A, Mazerolle SM, Eason CM (2017) Organizational Infrastructure in the Collegiate Athletic Training Setting, Part II: Benefits of and Barriers in the Athletics Model. Journal of Athletic Training 52(1): 23-34.
- Ekberg O, Persson NH, Abrahason PA, Westlin NE, Lilja B (1988) Longstanding Groin Pain in Athletes A Multidisciplinary Approach. Sports Medicine 6(1): 56-61.
- Arvinen-Barrow M, Walker N (2013) The psychology of sport injury and rehabilitation. The Psychology of Sport Injury and Rehabilitation 1-210.
- Tanaka MJ, Szymanski LM, Dale JL, Dixit S, Jones LC (2019) Team Approach: Treatment of Injuries in the Female Athlete: Multidisciplinary Considerations for Women’s Sports Medicine Programs. JBJS reviews 7(1): e7.
- Peeler J, Leiter J, MacDonald P (2010) Accuracy and reliability of anterior cruciate ligament clinical examination in a multidisciplinary sports medicine setting. Clinical Journal of Sport Medicine 20(2): 80-85.
- Thompson B, MacAuley D, McNally O, O’Neill S (2004) Defining the sports medicine specialist in the United Kingdom: a Delphi study. British Journal of Sports Medicine 38(2): 214-217.
- Theberge N (2008) The integration of chiropractors into healthcare teams: a case study from sport medicine. Sociology of Health & Illness 30(1): 19-34.
- Reiman MP, Lorenz DS (2011) INTEGRATION OF STRENGTH AND CONDITIONING PRINCIPLES INTO A REHABILITATION PROGRAM. International Journal of Sports Physical Therapy 6(3): 241.
- Bosch B, Mansell H (2015) Interprofessional collaboration in health care: Lessons to be learned from competitive sports 148(4): 176-179.
- Botto T, Schorr M, Daniel Lema J (2005) Integrating Web-Based Technology to Assist and Enhance Instruction, Assessment, and Application of Problem-Based Learning for Manual Therapy Techniques Used in Athletic Training and Sport Medicine.
- WA P (2012) Requiring professional athletic training programs at the post-baccalaureate level: considerations and concerns. Athl Train Educ J 7(1): 4-10.
- Mazerolle SM, Bowman TG, Pitney WA (2015) Multistakeholder Perspectives on the Transition to a Graduate-Level Athletic Training Educational Model. Journal of Athletic Training 50(9): 964-976.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...