Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2638-6003
Review Article(ISSN: 2638-6003) 
A literature review of the treatment options for Idiopathic Adhesive Capsulitis of the Shoulder Volume 4 - Issue 5
Rómulo Silva1*, Alice Pimentel2 and Manuel Gutierres3
- 1Department of Orthopedics, Alto Minho Local Health Unit, Viana do Castelo Maria Alice Gomes Conde Pimentel, Portugal
- 2Department of General Surgery, Centro Hospitalar do Baixo Vouga, Aveiro, Portugal
- 3Department of Orthopedics, Professor at Faculty of Medicine, University of Porto, Centro Hospitalar de São João, Portugal
Received: December 22, 2020; Published:January 07, 2021
Corresponding author:Rómulo Silva, Department of Orthopedics, Unidade Local de Saúde do Alto Minho, Estrada de Santa Luzia, 50 - Viana do Castelo, Portugal
DOI: 10.32474/OSMOAJ.2021.04.000199
<
Abstract
Goal: Systematic review of current therapeutic options for Idiopathic Adhesive Capsulitis of the shoulder (IAC).
Materials and Methods: Research carried out in the MEDLINE / Pubmed database using MeshTerms: “adhesive capsulitis”, “frozen shoulder”, “treatment”. The articles in Portuguese or English published were selected, after which non-relevant articles were excluded based on the title, reading of the abstract and full article.
Results: Physical therapy has proven to be beneficial, either isolated or concomitantly with other therapeutic approaches. Options like capsular distention, manipulation under anesthesia and arthroscopic surgery have reported good results, especially in refractory cases. No significant benefits were found with the use of oral corticosteroids, NSAIDs or acupuncture. New treatment options are currently being tested with promising results.
Conclusions: There are several effective options for the treatment of Adhesive Capsulitis. In the early stages, conservative measures should be chosen, with special emphasis on physical therapy within the limits of pain associated with low-dose intraarticular injection of corticosteroids. In refractory cases, more invasive treatment options should be suggested namely capsular distension and manipulation under anesthesia.
Keywords: Adhesive Capsulitis; Frozen Shoulder; Diagnosis; Treatment
Introduction
Adhesive capsulitis is a pathology characterized by a
spontaneous onset of insidious and diffuse pain in the shoulder
associated with progressive restriction of active and passive
motion of the glenohumeral joint [1]. Almost 150 years after its first
description, it remains an uncertain entity. The proper terminology,
used for the first time in 1945, is also controversial, since this
condition is related to the contraction and thickening of the
glenohumeral capsule, in particular the coracohumeral ligament
in the rotator’s interval [1, 2]. The disease is classified as primary
and secondary. The primary entity has an unknown etiology and
will be addressed in this review [3]. Secondary adhesive capsulitis
is caused by an event or triggering condition such as trauma,
surgery or a systemic condition such as diabetes mellitus, thyroid
abnormalities, etc. [2]. Diabetes mellitus has the most established
connection, with an estimated incidence of adhesive capsulitis
in 20% of this population [4]. The prevalence of this pathology
in the general population is believed to be 2-5%. However, it is
believed that the true prevalence is actually inferior and difficult to
determine, not only because vague and insidious symptoms lead to
numerous diagnostic errors, but also because most studies include
specific comorbidities with a greater incidence of IAC than within
the general population [2, 3, 5, 6].
This pathology occurs mainly between the 4th and 6th decade
of life and is thought to be more frequent in women [7]. Some argue that it affects the non-dominant side more often and that
in about 20-30% of cases it recurs on the contralateral shoulder,
usually in the first 5 years after the resolution of the primary
condition [1, 3, 7-10]. Although considered a benign condition,
with a self-limiting pattern and resolution within 2 to 3 years, it is
estimated that 20-50% of the cases continue with mild to moderate
pain and restricted movement over a period of up to 10 years [4,
11]. The etiology of adhesive capsulitis also remains uncertain
and theories vary. However, the evidence points to a chronic
inflammatory response with subsequent capsular fibrosis that
possibly involves increased deposition of cytokines such as TGF-β,
PDGF, TNF-α and IL-1 [1-3, 7]. There are also studies that advocate
an association with Dupuytren’s contracture that may involve the
same abnormalities. The changes found include: contraction and
fibrosis of the coracohumeral ligament, thickening and fibrosis
of the rotator’s interval, contraction of the anterior and inferior
capsule, decrease in joint volume, obliteration of the axillary recess
and neovascularization [2, 3]. The evolution of this pathology can
be divided into three phases. The acute initial phase (freezing
phase) is characterized by the insidious appearance of diffuse pain
and restriction of the range of motion of the glenohumeral joint,
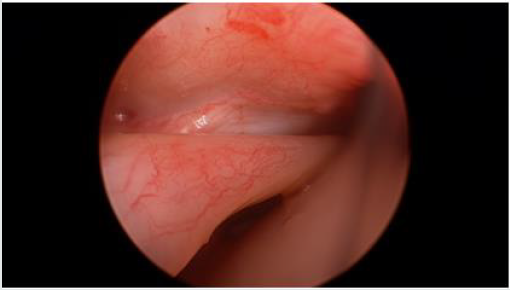
which lasts for about 10 to 36 weeks (Figure1). In the second phase
(frozen phase), for about 4 to 12 months, the pain slightly decreases
but the movement restriction continues, with almost total loss of
external rotation. In the resolution phase (thawing phase) there
is spontaneous progressive improvement in the range of motion
and resolution of pain. This last phase has an average duration
of 30 months (12 to 42 months) [3, 6-8]. Numerous studies have
attempted to determine which treatment is the most effective for
adhesive capsulitis. However, currently, despite the various options,
there is still no consensus among the authors regarding the most
advantageous treatment and at what stages of the disease it should
be performed [4, 12, 13]. Most of the evidence is inconclusive due
to the precarious methodology of the studies [14].
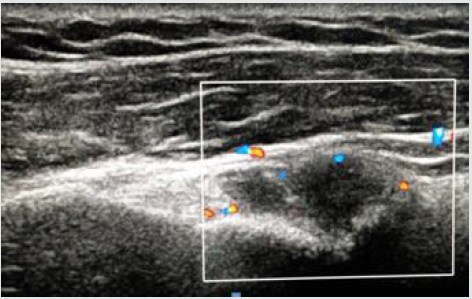
Figure 1: Arthroscopy - signs of synovitis and tenosynovitis characteristic of phase 1 of adhesive capsulitis
Diagnosis
There is no standard diagnostic method for this condition, which is based on clinical examination, exclusion of differential diagnosis, normal radiographic appearance and findings on ultrasound, magnetic resonance imaging (MRI) and arthrographic magnetic resonance imaging (arthroMRI) [2, 15]. The early diagnosis of adhesive capsulitis is extremely important since it allows the institution of therapy before the progression of thickening and contracture of the capsule observed in advanced stages [15]. Clinically, an insidious diffuse pain with at least four weeks that interferes with the activities of daily life should be investigated. Night pain is also common, with the patient complaining of more severe pain while sleeping on the affected side. Painful restriction of active and passive motion of the glenohumeral joint is also frequent, with special emphasis on external rotation (more than 50% of restriction) and elevation (less than 100ᴼ) [1, 3]. Radiographs do not normally show any changes, except for a slight periarticular osteopenia of the humeral head and neck, which can occasionally be found [1, 3, 7,15]. The most important role of radiography is the possibility of ruling out other pathologies such as calcifying tendinitis of the rotator cuff, osteoarthritis, avascular necrosis or fractures that can also cause painful movement restriction and be misdiagnosed as adhesive capsulitis [15, 16]. For a more accurate diagnosis, ultrasound, MRI or ArtroRM are usually necessary [15]. With the use of ultrasound, the diagnosis can be suspected by a thickening of the structures in the rotator’s interval, namely of the coracoumeral ligament, and restriction of the motion of the supraspinatus tendon during abduction. With echodoppler, synovial inflammation can be readily detected (Figure 2), which has advantages when compared with MRI and ArtroMRI since it is less expensive, faster, more dynamic and easily accessible [2, 3, 15].
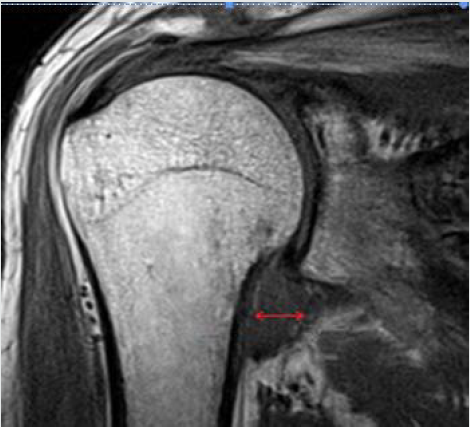
MRI is an effective non-invasive diagnostic tool, not only for cases where this condition is suspected, but also provides information that can help the surgeon differentiate between the different stages of the disease [3,15,17]. Although it is not diagnostic, some argue that the degree of capsular thickening, measured in the axillary recess, can be correlated with the clinical stage of adhesive capsulitis [16]. Among other findings, several characteristics of this condition can be seen: thickening of the coracohumeral and capsular ligament in the rotator’s interval and axillary recess (greater than 4 mm) and obliteration of the subcoracoid space by the thickened capsule (Figure 3). Thus, MRI allows for early diagnosis, determining the pathophysiological stage and ruling out differential diagnosis [15]. ArtroMRI allows for visualization of basic disease characteristics, namely the thickening of the coracohumeral ligament and the capsule, possibly with greater precision than the MRI, but also to detect decreased joint volume [1,3,15]. However, some claim that both MRI and ArtroMRI, despite the useful findings, are not indicated as a means of diagnosis for adhesive capsulitis and should only be used as a method of excluding other intra-articular pathologies [3].
Treatment
A great variety of therapeutic options are available for the treatment of adhesive capsulitis. During the early stages, where pain predominates, treatment should be directed towards pain relief and patients should be advised to limit activities according to their tolerance [7]. The secondary objective is to improve the range of motion [4] and restore the ability to perform the daily activities.
Conservative Treatment
Conservative treatment, such as physical therapy, is recommended in the freezing phase [4, 6]. Most patients will recover with this initial management [16, 18, 63]. The conservative approach has a wide range of modalities, with well documented results.
Physiotherapy
Isolated physiotherapy is a widely accepted treatment option,
which can also be used as a complement to other therapeutic
modalities [1, 3], with some reports considering it to be crucial
for success [4]. Currently, various techniques are used, such as
the application of moist heat, strengthening exercises, stretching
and manual exercises [7, 19, 20]. Several studies have compared
these modalities with different conclusions, making it difficult to
determine which is the most beneficial [4, 9,20]. Most studies in
which comparisons were made between two interventions did not
detect significant differences between the techniques [21]. In several
investigations, the techniques of high and low grade glenohumeral
mobilization were compared, with significant improvement after
12 months for both approaches. Some authors concluded that the
intensive approach was significantly more effective in restoring
mobility and reducing disability [20-22]. In contrast, others
argue that the amount of force applied should be adjusted to the
patient’s condition, limited to their tolerance, because if excessive
force is applied, it can produce extreme pain, periarticular injury
or abandonment of treatment, thus, one should opt for prolonged
progressive low-load stretches, a method considered safe and
effective [7, 9, 23].
In a study with level I evidence, the effectiveness of three
different physical therapy modalities was compared: group
physiotherapy, individual physiotherapy and home exercise
program. Not only was there a greater degree of symptomatic
improvement in the shoulder, but also better anxiety control with
group physiotherapy. There were also benefits in relation to costeffect
and self-management in this group. However, standard
physical therapy remains a good alternative and has been shown
to be significantly better than unsupervised home exercises [6].
In another study with level II evidence in which regular physical
therapy was compared with a new contraction technique, the new
approach demonstrated greater recovery of the function of the
glenohumeral joint when compared to the group of normal physical
therapy. However, further studies are needed to validate this conclusion [24]. Some authors advise a Multimodal Care program
that includes mobilization, shoulder orthoses and stretches
with strengthening exercises, which appears to be beneficial for
symptomatic relief, although the evidence seems limited [25, 26].
Horst, et al. compared structural-oriented (conventional)
physical therapy with an activity-oriented physiotherapeutic
treatment, concluding that therapy based on performing activities
appears to be more effective for pain reduction and the ability to
perform daily life activities than conventional treatment methods
[64]. When compared to ad initium arthroscopy, physical therapy
produces similar results, but without surgical aggression and with
a better cost-benefit ratio [27]. Lamplot, et al. in a level III cohort
study [57] found a decrease in the need of a second intra-articular
injection in the patients who underwent physical therapy following
the first injection, underlining the major role of physiotherapy in
the treatment of IAC.
Intra-Articular Injection of Corticosteroids
Corticosteroids have been administered to the glenohumeral
joint in several ways, namely anterior, lateral and / or posterior
approach [4, 28]. Although clinically it is common practice to use an
injection via an anterior or posterior approach, studies comparing
different techniques have not found significant differences in the
improvement of pain or range of motion [11, 29]. Cho, et al. [60] in
a randomized trial study found that the efficacy of corticosteroid
injection into the subacromial space in IAC was inferior to intraarticular
injection up to 12 weeks. However, a combination of
injection sites had an additive effect on the benefits in the internal
rotation angle There is no agreement regarding the optimal dose of
intra-articular corticosteroids. Yoon et al. did not detect a significant
difference between the low (20 mg) or high (40 mg) dose groups,
indicating, due to its side effects, the preferential use of low dose
corticosteroids for the treatment of adhesive capsulitis [30].
A limitation of the use of intra-articular corticosteroids is the
fact that blind injections can be inaccurate in about 60% of cases.
The current use of ultrasound or fluoroscopy-guided injection
can overcome this problem [8, 16]. It has been shown in several
studies that this practice improves accuracy and results compared
to the “blind-technique” [3, 31]. There is evidence that the initial
corticosteroid injection can reduce pain and improve range of
motion in the short term and that its benefit can be increased in
the short and medium term when these injections are followed by
physical therapy [11, 21, 57]. Kraal et al. in a two center, randomized
controlled trial, found that additional physiotherapy after
corticosteroid injection improves ROM and functional limitations
in early-stage IAC up to the first three months, underlining the good
results of these techniques combined [61].
When compared as isolated treatments, there is strong
evidence in benefit of corticosteroid injection in the short term (4-6
weeks), compared to isolated physical therapy, but not in the long term [11, 22, 30, 32, 33]. In a study that compared the injection of
corticosteroids and the benefit of isolated intra-articular analgesics,
significant improvements were found with the administration of
corticosteroids [22]. Hettrich et al. showed that corticosteroid
injections decreased fibromatosis and myofibroblasts in the
shoulders with IAC [58]. On the other hand, some studies conclude
that this form of treatment has results similar to isolated physical
therapy or more invasive treatments such as MUA and arthroscopy
[29, 32, 34], confirming the high degree of controversy surrounding
this disease.
Echography-Guided Capsular Distension
Ultrasound-guided interventions have several strong points like the lack of radiation and the possibility of real time visualization of the needle’s trajectory. This technique has advantages when compared to fluoroscopy, CT and MRI since these are less practical, more time consuming and involve radiation or a specific needle [35]. One of the modalities of capsular distention is based on the use of hyaluronic acid. The ideal time between injections is one week and the effects are usually seen after the second injection [36]. In a study comparing this approach with the injection of corticosteroids, it was found to be more effective in favor of distension with hyaluronic acid in passive external rotation (10ᴼ) at 2 and 6 weeks, with no significant differences in pain relief or in function recovery. This study also concluded that this approach is a good alternative to intra-articular injection of corticosteroids and can be especially useful in patients with diabetes mellitus or contraindicated to the use of corticosteroids [37]. Calis et. al. also concluded that this approach is effective in the treatment of adhesive capsulitis when compared to isolated corticosteroid injection, physical therapy and exercise [36]. Ultrasound-guided capsular hydrodistension is a procedure that aims to distend the capsule contracted by increasing pressure by injecting large amounts of sodium chloride into the glenohumeral joint [9]. There is evidence that it provides relief from pain and improves range of motion, especially when it is followed by physical therapy [29, 38]. Other studies have found that saline distension with or without concomitant corticosteroids are more effective than MUA, describing better results after 6 months with this procedure, with less risk, and resulting in a higher level of satisfaction on the part of patients. However, the effects do not seem to persist beyond 6-12 weeks [9, 29, 39, 40].
Artrographic Capsular Distension
This technique can be performed with sodium chloride, local anesthetic, steroids, contrast or air. It should be reserved for patients who do not improve despite physical therapy [22]. It is also considered a good therapeutic option for rapid symptom relief. Better results were observed when followed by physical therapy [38]. There was no significant difference in the efficacy of capsular distention with or without corticosteroids in most investigations [39, 41]. However, Rysns et al. when comparing distension with corticosteroid injection with placebo saline injection to determine whether the results were due only to the increase in volume, found a significant improvement with the concomitant use of corticosteroids [32].
Extracorporeal Shockwave Therapy
The use of Extracorporeal Shock Wave Therapy (ESWT) in the treatment of several shoulder diseases, namely in calcific tendinopathy of the rotators cuff, is well documented. Several studies evaluate its usefulness in IAC, with positive effects such as a quicker return to daily activities and quality-of-life improvement [66, 67], at least in the short-term. El Naggar, et al. compared the effectiveness of radial extracorporeal shock-wave therapy versus ultrasound-guided low-dose intra-articular steroid injection in in diabetic patients, concluding that in the short-term follow-up ESWT was superior to a low-dose intra-articular steroid injection in improving function and pain in diabetic patients with shoulder IAC [68], therefore validating it as an alternative to steroid injections in diabetic patients with this pathology. This particular usefulness of ESWT in diabetic patients has also been documented in other studies [69, 70]. Many prospective randomized trials are underway to further validate ESWT as a treatment option in IAC, especially in the diabetic population.
Other
Oral non-steroidal anti-inflammatory drugs, although widely used in the initial / inflammatory phases for pain relief in the short term, did not prove their benefit when compared with placebo [3, 7, 9]. Prednisone at a dose of 40 to 60 mg / day for two to three weeks provides faster relief of symptoms in the short term, but their effects are not significant after 6 weeks and there is no evidence that they shorten the duration of disease [28]. Some studies have concluded that there may be a moderate short-term benefit with acupuncture associated with exercise [22], however the usefulness of this therapeutic approach remains undetermined [21]. Calcitonin is a polypeptide hormone secreted from parafollicular cells of the thyroid that has been used for pain control in several pathologies. Although its pathophysiology is not totally clear, it is thought to diminish the inflammatory response and increase endorphins’ release [71, 72]. Rouhani, et al. in a double-blinded randomized controlled trial compared intranasal calcitonin versus placebo for 6 weeks and found great improvement of shoulder pain, ROM, and functional scores in the calcitonin group [71]. Currently the dose recommendation is 200 U (1 puff) daily [73]. Regarding future approaches, Badalamente, et al. [53, 54] published two papers evaluating the applicability of extra-articular collagenase injections in the anterior shoulder capsule. In a placebo controlled doubleblind RCT, they found improvements in shoulder motion, functional score and pain control in the collagenase group in their 1.8 years follow up. In a randomized pilot study comparing subcutaneous adalimumab with local corticosteroids, Schydlowsky et al. found no benefits with the anti-TNF agent in the treatment of frozen shoulder [55] These new treatment approaches for IAC must undergo further investigation, but, if developed, could also play a role in the management of other arthrofibrosis [56].
Surgical Treatment
Surgical treatment of adhesive capsulitis is considered after failure of conservative treatment. It is estimated that 10% of patients do not respond to non-invasive treatment [25, 26]. There are no defined guidelines for this transition. However, regardless of the chosen conservative treatment, a surgical approach is only considered after about 6 months of non-surgical treatment without clinical improvement [3, 4, 8, 12, 16, 42]. Its benefit in refractory / severe adhesive capsulitis is proven and well documented [43], and some studies have found that in patients with high risk factors such as diabetes mellitus, and those who suffer chronic symptoms or bilaterally affected, early surgery is beneficial [65]. In a recent questionnaire to health professionals, only 3% recommended surgical treatment in the acute phase, while 47% recommended it in the second and third stages of the disease [4]. Surgical treatments should be complemented with an appropriate physical therapy scheme [63]. Some advocate the initiation of immediate postoperative physiotherapy, with light isometric exercises after 1-2 weeks and isotonic exercises in the following 2-3 weeks. Ideally the range of motion without complete restriction should be achieved in 12 to 16 weeks [4].
Manipulation Under Anesthesia
This procedure involves stabilizing the shoulder blade with flexion, abduction and adduction, followed by maximum internal and external rotation. Some studies advocate good results with this technique, mainly in terms of range of motion [44], others have not found significant differences in comparison with other treatments [45]. There is modest evidence of the benefit of MSA in relieving pain and recovering mobility when followed by physical therapy [46]. However, some authors have not found significant differences in the improvement of pain, function, disability or range of motion in the short, medium or long term between isolated MUA and exercise-associated MUA when compared to physical therapy alone [21, 45]. When compared with arthroscopy, better results were observed with arthroscopic distention at 6 months [21]. However, more recently, Schoch et al. in a study with the largest series of patients undergoing surgical treatment of adhesive capsulitis with a direct comparison between MUA, MUA/Capsular release (CR), and CR alone, found significant improvement of the ROM in all surgical modalities, however, the MUA group had the greatest external rotation, postoperatively [59]. MUA has been associated with several intra-articular iatrogenic complications such as humeral fracture, glenohumeral dislocation, brachial plexus injury rotator cuff injury and hemarthrosis [4, 46, 47]. Nonetheless, some argue that these lesions have no clinical relevance or that they can be minimized by performing the technique properly [44, 47]. Others advise that this procedure should be avoided in patients with osteoporosis, osteopenia or previous MUA recurrence [46]. Another limitation of manipulation is the fact that stretching the tissues can cause severe pain after the end of the anesthesia effect, leading to delays in recovery [8].
Arthroscopy
Arthroscopy allows the distension of the glenohumeral joint to be combined with a series of other procedures, such as adhesions release, opening of the rotator’s interval, circular capsulotomy and section of the coracohumeral ligament. This procedure must be followed by physiotherapy [2]. Several studies have supported the role of this approach as safe and effective in the treatment of adhesive capsulitis [27, 48, 49]. Several authors support the use of arthroscopy, claiming that, in addition to the good results obtained, it makes it possible to deepen and confirm the diagnosis by a complete assessment of the shoulder joint during the procedure [4, 8]. Some, on the contrary, argue that currently the evidence does not support the use of this technique [50], underlining the prevalent controversy in the treatment of this pathology. Recent investigations have not shown greater benefits in range of motion with more extensive release of the capsule (anterior release vs. Anterior plus posterior release) [9, 62]. Sivasubramanian et al. made a systematic review and meta-analysis which suggests that less extensive releases may result in better functional and pain scores. The addition of a posterior release appears to increase early internal rotation, but doesn’t maintain that benefit over time. No benefit was found with the complete 360 release [62]. Some authors suggest that arthroscopic distension can be associated with concomitant manipulation, with improved outcomes [8]. In a study comparing arthroscopy plus manipulation against isolated intraarticular corticosteroid injection, both approaches were effective in improving pain and range of motion. However, the objectives were achieved sooner by the group that underwent arthroscopy (6 weeks vs 12 weeks) [51]. Grant, et al. compared arthroscopic distention with MUA finding a small benefit in favor of arthroscopy alone or in association with manipulation, advising this technique due to the lower number of complications [52]. On the other hand, Jerosch et al. concluded that this therapy has a greater benefit in reducing pain and improving movement, even in the long term, being a valuable, more precise, controlled option with fewer complications than manipulation [12].
Open Surgery
Surgical treatments have changed from open to arthroscopic procedures and, therefore, the open technique, although effective, has fallen into disuse [4]. It is rarely used nowadays, but may be beneficial in cases refractory to MUA and arthroscopy [9].
Conclusion
Idiopathic adhesive capsulitis is an extremely painful and limiting pathology of the shoulder, which, despite the abundant published literature, remains controversial in many aspects. Its etiology is unknown, but synovial inflammation of the glenohumeral joint and subsequent progressive capsular fibrosis is believed to occur. The correct diagnosis of this condition is a crucial step in patient orientation. Although the diagnosis is mostly clinical, ultrasound, MRI and ArtroMRI have gained increasing importance, as they more accurately allow ruling out other conditions. Despite the various therapeutic options available, there is still no global consensus among authors regarding the most appropriate approach for the treatment of IAC of the shoulder and there is a need for high-level, definitive evidence to elaborate definitive approach guidelines. Initially, conservative measures should always be chosen, with the majority of patients recovering with non-surgical treatment. There is evidence that demonstrates the effectiveness of physical therapy, being considered by many authors as an essential component of treatment. Corticosteroid injection is an effective form of treatment, especially when guided by ultrasound, with evidence of its benefit in the short, but not long term (after 6 weeks). Lower dosages have been advised in order to minimize its possible adverse effects. ESWT is gaining popularity in the treatment of diabetic and refractory cases, with many studies underway to further validate its importance. Calcitonin and collagenase are two relatively new approaches to the disease, with promising results. Ultrasound-guided capsular distention with hyaluronic acid appears to be useful in the treatment of adhesive capsulitis, being mainly suitable in patients with Diabetes Mellitus or in those with contraindications to corticosteroids. Hydrodistension is an effective method, with results similar to MUA, but with a lower rate of complications, although its effect does not seem to last beyond 6-12 weeks. Arthrographic capsular distention is considered a good option for rapid pain relief, especially in cases refractory to physical therapy. Oral corticosteroids, while providing short-term pain relief, do not appear to shorten the duration of the disease. The association of corticosteroid injection guided by ultrasound with physiotherapy, demonstrated a statistically significant improvement, being advocated by many as the ideal approach for early stages.Surgical treatment should be reserved for cases with unsatisfactory results with conservative approaches, that is, after about 6 months without clinical improvement. Regardless of the surgical therapeutic option, it should be followed by rehabilitation physiotherapy.
MUA and arthroscopy are effective in the treatment of idiopathic adhesive capsulitis, especially in severe and complicated cases. MUA, although very popular in the past, has recently gained some skepticism because of the frequently associated complications.
Conflict of Interest and Funding
Nothing to declare.
References
- Abstract
- Introduction
- Conclusion
- Conflict of Interest and Funding
- References
- Brue S, Valentin A, Forssblad M, Werner S, Mikkelsen C, et al. (2007) Idiopathic adhesive capsulitis of the shoulder: a review. Knee Surg Sports Traumatol Arthrosc 15(8): 1048-1054.
- Lewis J (2014) Frozen shoulder contracture syndrome - Aetiology, diagnosis and management. Man Ther 20(1): 2-9.
- Hsu JE, Anakwenze OA, Warrender WJ, Abboud JA (2011) Current review of adhesive capsulitis. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons 20(3): 502-514.
- Sharma S, Leo Jacobs (2011) Management of frozen shoulder - conservative vs surgical? Ann R Coll Surg Engl 93(5): 343-344.
- Bunker TD (1997) Frozen shoulder: unravelling the enigma. Ann R Coll Surg Engl 79(3): 210-213.
- Russell S, Jariwala A, Conlon R, Selfe J, Richards J, et al. (2014) A blinded, randomized, controlled trial assessing conservative management strategies for frozen shoulder. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons 23(4): 500-507.
- Dias R, Cutts S, Massoud S (2005) Frozen shoulder. Bmj 331(7530): 1453-1456.
- Manske RC, Prohaska D (2008) Diagnosis and management of adhesive capsulitis. Curr Rev Musculoskelet Med 1(3-4): 180-189.
- Neviaser AS, Hannafin JA (2010) Adhesive capsulitis: a review of current treatment. Am J Sports Med 38(11): 2346-2356.
- Hand GC, Athanasou NA, Matthews T, Carr AJ (2007) The pathology of frozen shoulder. J Bone Joint Surg Br 89(7): 928-932.
- Blanchard V, Barr S, Cerisola FL (2010) The effectiveness of corticosteroid injections compared with physiotherapeutic interventions for adhesive capsulitis: a systematic review. Physiotherapy 96(2): 95-107.
- Jerosch J, Nasef NM, Peters O, Mansour AM (2013) Mid-term results following arthroscopic capsular release in patients with primary and secondary adhesive shoulder capsulitis. Knee Surg Sports Traumatol Arthrosc 21(5): 1195-1202.
- Dundar U, Toktas H, Cakir T, Evcik D, Kavuncu V, et al. (2009) Continuous passive motion provides good pain control in patients with adhesive capsulitis. Int J Rehabil Res 32(3): 193-198.
- Hanchard NC, Goodchild L, Thompson J, O'Brien T, Davison D, et al. (2012) Evidence-based clinical guidelines for the diagnosis, assessment and physiotherapy management of contracted (frozen) shoulder: quick reference summary. Physiotherapy 98(2): 117-120.
- Harris G, Bou-Haidar P, Harris C (2013) Adhesive capsulitis: review of imaging and treatment. J Med Imaging Radiat Oncol 57(6): 633-643.
- Ewald A (2011) Adhesive capsulitis: a review. Am Fam Physician 83(4): 417-422.
- Sofka CM, Ciavarra GA, Hannafin JA, Cordasco FA, Potter HG, et al. (2008) Magnetic resonance imaging of adhesive capsulitis: correlation with clinical staging. Hss j 4(2): 164-169.
- Rill BK, Fleckenstein CM, Levy MS, Nagesh V, Hasan SS, et al. (2011) Predictors of outcome after nonoperative and operative treatment of adhesive capsulitis. Am J Sports Med 39(3): 567-574.
- Kelley MJ, Shaffer MA, Kuhn JE, Michener LA, Seitz AL, et al. (2013) Shoulder pain and mobility deficits: adhesive capsulitis. J Orthop Sports Phys Ther 43(5): A1-31.
- Vermeulen HM, Rozing PM, Obermann WR, le Cessie S, Vliet Vlieland TP, et al. (2006) Comparison of high-grade and low-grade mobilization techniques in the management of adhesive capsulitis of the shoulder: randomized controlled trial. Phys Ther 86(3): 355-368.
- Maund E, Craig D, Suekarran S, Neilson A, Wright K, et al. (2012) Management of frozen shoulder: a systematic review and cost-effectiveness analysis. Health Technol Assess 16(11): 1-264.
- Favejee MM, Huisstede BM, Koes BW (2011) Frozen shoulder: the effectiveness of conservative and surgical interventions--systematic review. Br J Sports Med 45(1): 49-56.
- Donatelli R, Ruivo RM, Thurner M, Ibrahim MI (2014) New concepts in restoring shoulder elevation in a stiff and painful shoulder patient. Phys Ther Sport 15(1): 3-14.
- Paul A, Rajkumar JS, Peter S, Lambert L (2014) Effectiveness of sustained stretching of the inferior capsule in the management of a frozen shoulder. Clin Orthop Relat Res. 472(7): 2262-2268.
- Hand C, Clipsham K, Rees JL, Carr AJ (2008) Long-term outcome of frozen shoulder. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons 17(2): 231-236.
- Levine WN, Kashyap CP, Bak SF, Ahmad CS, Blaine TA, et al. (2007) Nonoperative management of idiopathic adhesive capsulitis. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons 16(5): 569-573.
- Berghs BM, Sole-Molins X, Bunker TD (2004) Arthroscopic release of adhesive capsulitis. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons 13(2): 180-185.
- Buchbinder R, Hoving JL, Green S, Hall S, Forbes A, et al. (2004) Short course prednisolone for adhesive capsulitis (frozen shoulder or stiff painful shoulder): a randomised, double blind, placebo controlled trial. Ann Rheum Dis 63(11): 1460-1469.
- Jacobs LG, Smith MG, Khan SA, Smith K, Joshi M, et al. (2009) Manipulation or intra-articular steroids in the management of adhesive capsulitis of the shoulder? A prospective randomized trial. Journal of shoulder and elbow surgery/American Shoulder and Elbow Surgeons 18(3): 348-353.
- Yoon SH, Lee HY, Lee HJ, Kwack KS (2013) Optimal dose of intra-articular corticosteroids for adhesive capsulitis: a randomized, triple-blind, placebo-controlled trial. Am J Sports Med 41(5): 1133-1339.
- Lee HJ, Lim KB, Kim DY, Lee KT (2009) Randomized controlled trial for efficacy of intra-articular injection for adhesive capsulitis: ultrasonography-guided versus blind technique. Arch Phys Med Rehabil 90(12): 1997-2002.
- Ryans I, Montgomery A, Galway R, Kernohan WG, McKane R, et al. (2005) A randomized controlled trial of intra-articular triamcinolone and/or physiotherapy in shoulder capsulitis. Rheumatology (Oxford) 44(4): 529-535.
- Sheridan MA, Hannafin JA (2006)Upper extremity: emphasis on frozen shoulder. Orthop Clin North Am 37(4): 531-539.
- Tveita EK, Tariq R, Sesseng S, Juel NG, Bautz-Holter E, et al. (2008) Hydrodilatation, corticosteroids and adhesive capsulitis: a randomized controlled trial. BMC Musculoskelet Disord 9: 53.
- Martinoli C, Bianchi S, Prato N, Pugliese F, Zamorani MP, et al. (2003) US of the shoulder: non-rotator cuff disorders. Radiographics 23(2): 381-401.
- Calis M, Demir H, Ulker S, Kirnap M, Duygulu F, et al. (2006) Is intraarticular sodium hyaluronate injection an alternative treatment in patients with adhesive capsulitis? Rheumatol Int 26(6): 536-540.
- Park KD, Nam HS, Lee JK, Kim YJ, Park Y, et al. (2013) Treatment effects of ultrasound-guided capsular distension with hyaluronic acid in adhesive capsulitis of the shoulder. Arch Phys Med Rehabil 94(2): 264-270.
- Buchbinder R, Youd JM, Green S, Stein A, Forbes A, et al. (2007) Efficacy and cost-effectiveness of physiotherapy following glenohumeral joint distension for adhesive capsulitis: a randomized trial. Arthritis Rheum 57(6): 1027-1037.
- Buchbinder R, Green S, Youd JM, Johnston RV, Cumpston M, et al. (2008) Arthrographic distension for adhesive capsulitis (frozen shoulder). The Cochrane database of systematic reviews 1: Cd007005.
- Quraishi NA, Johnston P, Bayer J, Crowe M, Chakrabarti AJ, et al. (2007) Thawing the frozen shoulder. A randomised trial comparing manipulation under anaesthesia with hydrodilatation. J Bone Joint Surg Br 89(9): 1197-2000.
- Buchbinder R, Green S (2004) Effect of arthrographic shoulder joint distension with saline and corticosteroid for adhesive capsulitis. Br J Sports Med 38(4): 384-385.
- Drakos MC, Green DM, Dodson CC, Allen AA, Warren RF (2008) Shoulder dislocation after mobilization procedures for adhesive capsulitis. Orthopedics 31(12).
- Chen J, Chen S, Li Y, Hua Y, Li H, et al. (2010) Is the extended release of the inferior glenohumeral ligament necessary for frozen shoulder? Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association 26(4): 529-535.
- Farrell CM, Sperling JW, Cofield RH (2005) Manipulation for frozen shoulder: long-term results. Journal of shoulder and elbow surgery/American Shoulder and Elbow Surgeons 14(5): 480-484.
- Kivimaki J, Pohjolainen T (2001) Manipulation under anesthesia for frozen shoulder with and without steroid injection. Arch Phys Med Rehabil 82(9): 1188-1190.
- Ng CY, Amin AK, Narborough S, McMullan L, Cook R, et al. (2009) Manipulation under anaesthesia and early physiotherapy facilitate recovery of patients with frozen shoulder syndrome. Scott Med J 54(1): 29-31.
- Loew M, Heichel TO, Lehner B (2005) Intraarticular lesions in primary frozen shoulder after manipulation under general anesthesia. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons 14(1): 16-21.
- Baums MH, Spahn G, Nozaki M, Steckel H, Schultz W, et al. (2007) Functional outcome and general health status in patients after arthroscopic release in adhesive capsulitis. Knee Surg Sports Traumatol Arthrosc 15(5): 638-644.
- Cinar M, Akpinar S, Derincek A, Circi E, Uysal M, et al. (2010) Comparison of arthroscopic capsular release in diabetic and idiopathic frozen shoulder patients. Archives of orthopaedic and trauma surgery 130(3): 401-406.
- Dattani R, Ramasamy V, Parker R, Patel VR (2013) Improvement in quality of life after arthroscopic capsular release for contracture of the shoulder. Bone Joint J 95-b(7): 942-946.
- De Carli A, Vadala A, Perugia D, Frate L, Iorio C, et al. (2012) Fabbri M, et al. Shoulder adhesive capsulitis: manipulation and arthroscopic arthrolysis or intra-articular steroid injections? Int Orthop 36(1): 101-106.
- Grant JA, Schroeder N, Miller BS, Carpenter JE (2013) Comparison of manipulation and arthroscopic capsular release for adhesive capsulitis: a systematic review. Journal of shoulder and elbow surgery/American Shoulder and Elbow Surgeons 22(8): 1135-1145.
- Badalamente MA, Wang E (2006) Enzymatic capsulotomy for adhesive capsulitis of the shoulder. Paper presented at American Academy of Orthopaedic Surgeons annual meeting 117494-8181.
- Wang ED, Badalamente MA, Mackenzie S, Michael Skyhar, James Tursi, et al. (2015) Phase 2a Study of Safety/Efficacy of Collagenase (CCH) in Patients with Adhesive Capsulitis. The Journal Of Hand Surgery 40(9): e50.
- Schydlowsky P, Szkudlarek M, Madsen OR (2012) Treatment of frozen shoulder with subcutaneous TNF-alpha blockade compared with local glucocorticoid injection: a randomised pilot study. Clin Rheumatol 31(8): 1247-1251.
- Le HV, Lee SJ, Nazarian A, Rodriguez EK (2017) Adhesive capsulitis of the shoulder: review of pathophysiology and current clinical treatments. Shoulder Elbow 9(2): 75-84.
- Lamplot JD, Lillegraven O, Brophy RH (2018) Outcomes From Conservative Treatment of Shoulder Idiopathic Adhesive Capsulitis and Factors Associated With Developing Contralateral Disease. Orthop J Sports Med 6(7): 2325967118785169.
- Hettrich CM, DiCarlo EF, Faryniarz D, Vadasdi KB, Williams R, et al. (2016) The effect of myofibroblasts and corticosteroid injections in adhesive capsulitis. J Shoulder Elbow Surg 25(8): 1274-1279.
- Schoch B, Huttman D, Syed UA, Patel MS, Lazarus MD, et al. (2020) Surgical Treatment of Adhesive Capsulitis: A Retrospective Comparative Study of Manipulation Under Anesthesia and/or Capsular Release. Cureus 12(7): e9032.
- Cho CH, Kim du H, Bae KC, Lee D, Kim K, et al. (2016) Proper site of corticosteroid injection for the treatment of idiopathic frozen shoulder: Results from a randomized trial. Joint Bone Spine 83(3): 324-329.
- Kraal T, Sierevelt I, van Deurzen D, van den Bekerom MP, et al. (2018) Corticosteroid injection alone vs additional physiotherapy treatment in early stage frozen shoulders. World J Orthop 9(9): 165-172.
- Sivasubramanian H, Chua CXK, Lim SY, Manohara R, Wen Dennis NZ, et al. (2020) Prem Kumar V, Poh KS. Arthroscopic Capsular Release to treat idiopathic frozen shoulder: How much release is needed? Orthop Traumatol Surg Res pp. 102766.
- Date A, Rahman L (2020) Frozen shoulder: overview of clinical presentation and review of the current evidence base for management strategies. Future Sci OA 6(10): FSO647.
- Horst R, Maicki T, Trąbka R, Albrecht S, Schmidt K, et al. (2017) Activity- vs. structural-oriented treatment approach for frozen shoulder: a randomized controlled trial. Clin Rehabil 31(5): 686-695.
- Eljabu W, Klinger HM, von Knoch M (2016) Prognostic factors and therapeutic options for treatment of frozen shoulder: a systematic review. Arch Orthop Trauma Surg 136(1): 1-7.
- Vahdatpour B, Taheri P, Zade AZ, Moradian S (2014) Efficacy of extracorporeal shockwave therapy in frozen shoulder. Int J Prev Med 5(7): 875-881.
- Chen CY, Hu CC, Weng PW, Huang YM, Chiang CJ, et al. (2014) Extracorporeal shockwave therapy improves short-term functional outcomes of shoulder adhesive capsulitis. J Shoulder Elbow Surg 23(12): 1843-1851.
- El Naggar TEDM, Maaty AIE, Mohamed AE (2020) Effectiveness of radial extracorporeal shock-wave therapy versus ultrasound-guided low-dose intra-articular steroid injection in improving shoulder pain, function, and range of motion in diabetic patients with shoulder adhesive capsulitis. J Shoulder Elbow Surg 29(7): 1300-1309.
- Muthukrishnan R, Rashid AA, Al-Alkharji F (2019) The effectiveness of extracorporeal shockwave therapy for frozen shoulder in patients with diabetes: randomized control trial. J Phys Ther Sci 31(7): 493-497.
- Santoboni F, Balducci S, D’Errico V, Jonida Haxhi, Mario Vetrano et al. (2017) Extracorporeal shockwave therapy improves functional outcomes of adhesive capsulitis of the shoulder in patients with diabetes. Diabetes Care 40(2): e12-e13.
- Rouhani A, Mardani-Kivi M, Bazavar M, Mahmood Barzgar, Ali Tabrizi, et al. (2016) Calcitonin effects on shoulder adhesive capsulitis. Eur J Orthop Surg Traumatol 26(6): 575-580.
- Yang R, Deng H, Hou J, Li W, Zhang C,et al. (2020) Investigation of salmon calcitonin in regulating fibrosis-related molecule production and cell-substrate adhesion in frozen shoulder synovial/capsular fibroblasts. J Orthop Res 38(6): 1375-1385.
- Redler LH, Dennis ER (2019) Treatment of Adhesive Capsulitis of the Shoulder. Journal of the American Academy of Orthopaedic Surgeons 27(12): e544-e554.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...