Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2644-1209
Case Report(ISSN: 2644-1209) 
Treatment Of Idiopathic Choroidal Neovascular Membrane in Young Female Patient by Intravitreal Aflibercept Injection Volume 1 - Issue 3
Alper Halil Bayat1,Selim Bölükbaşı1, Gamze Maden1*, Akın Çakır1, Burak Erden1, Mehmet Egemen Karatas2 and Mustafa Nuri Elçioğlu1
- 1Department of Ophthalmology, Okmeydanı Research&Traning Hospital, University of Health Sciences, Istanbul, Turkey
- 2Department of Ophthalmology, Sisli Hamidiye Etfal Training and Research Hospital, Istanbul, Turkey
Received: May 26, 2018; Published: June 06, 2018
*Corresponding author: Gamze Maden, Department of Ophthalmology, Sisli Hamidiye Etfal Training and Research Hospital, Istanbul, Turkey
DOI: 10.32474/TOOAJ.2018.01.000116
Abstract
This case is about idiopathic choroidal neovascular membrane (CNV) in a 30 year old female patient who presented with visual loss in the right eye for one month. The initial vision acuity (VA) of the patient was 1/10. In the fundus fluorescein angiography (FFA) and optical coherence tomography (OCT) of the patient, staining and macular leakage consistent with CNV in the peripapillary region were detected. Intravitreal injection of aflibercept was performed on the patient’s eye. At the first month follow-up, the patient’s VA was 10/10.
Abbrevations: CNV: Choroidal Neovascular Membrane; VA: Vision Acuity; OCT: Optical Coherence Tomography; FFA: Fundus Fluorescein Angiography
Introduction
In patients younger than 50 years, CNV usually develops due to secondary causes such as trauma, angioid streaks, inflammation, pathologic myopia, ocular histoplasmosis [1]. Apart from this, some young patients develop CNV without any reason. This group is called idiopathic CNV [2]. CNV in these patients respond better to treatment than age related macular degeneration[3]. In the literature, idiopathic CNV has been reported in a small number of young patients[4]. This report is about a case in which a 30 years old young healthy patient with idiopathic CNV responded well to intravitreal aflibercept treatment.
Case report
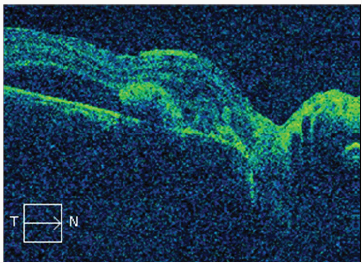
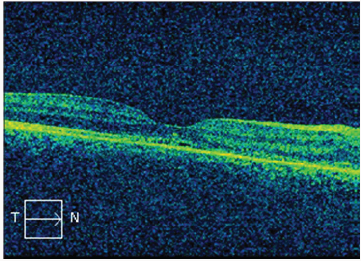
The patient who was 30 years old female applied to our clinic with loss of vision in the right eye. The initial VA was 1/10. The patient was not traumatized or had any disease story. Visual acuity was normal in the patient’s left eye. There was not any pathology in the anterior segment of the patient. In the posterior segment of the right eye, the peripapillary resemble the CNV like appearance and hemorrhage was observed under the retina. Left eye was normal. In the FFA of the patient, peripapillary region-compatible CNV staining was observed in the late period (Figure 1). In OCT, CNV and subretinal fluid of the macula were detected (Figure 2). On this basis, all blood tests, serologies and chest radiographs of the patient were drawn to distinguish possible inflammatory causes. There was not any inflammatory pathology in the results. Intravitreal injection of aflibercept was applied to the patient for treatment. On the first month of treatment the patient was found to have vision 10/10 and the OCT showed decreased fluid. The patient received a second dose of aflibercept. At the second month of treatment the patient was found to have visual impairment 10/10 and no fluid in OCT (Figure 3). At the 6th month of the visit, vision is still at 10/10, and no fluid is found in OCT.
Figure 1: Peripapillary CNV and subretinal hemorrhage appearance in fundus color photograph, hyperfluorescence appearance in early phase of FFA due to CNV and hyperfluorescence appearance in late phase due to leakage.
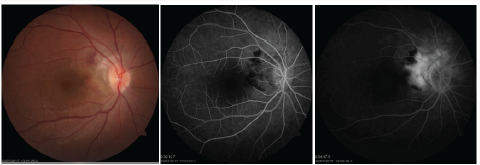
Figure 3: The patient’s second-month control, OCT image shows that the fluid is regressing after treatment.
Discussion
There are many reasons in the etiology of CNV, but the underlying pathology of these causes is the defect in the bruch’s membrane. A good biomicroscopic examination and all laboratory tests should be performed to distinguish the etiologic causes of the patient. Despite all this, no systemic disease or vitreous retinal pathology could be detected. There are several case reports of idiopathic CNV in the current literature [5,6]. There are options in current treatment of CNV such as ocular photodynamic therapy, thermal laser therapy and anti-vascular endothelial growth hormone (anti-VEBF). Mandal et al. they performed intravitreal bevacizumab injection in a report of 32 eyes with idiopathic CNV patients and 19 of them had improved VA [7]. Carreno E et al. [8] have demonstrated the efficacy of intravitreal ranibizumab in patients with idiopathic CNV. In this case, we wanted to demonstrate the efficacy of aflibercept injection in patient with idiopathic peripapillary CNV. While the initial VA of the patient with acute visual loss was 1/10, the VA after the first injection was 10/10, but the subretinal fluid persisted in OCT. After the second dose of aflibercept injection, the patient’s VA was maintained at 10/10, whereas there was not any subretinal fluid in the OCT. The patient was not injected with a third dose. The final VA at the 6th month was found to be 10/10 and no subretinal fluid was found in OCT.
Conclusion
In conclusion, intravitreal aflibercept injection was found to be effective in the patient with idiopathic CNV. Prospective and randomized clinical trials are needed to better understand efficacy of aflibercept treatment in the idiopathic CNV.
References
- Cohen SY, Laroche A, Leguen Y, Soubrane G, Coscas GJ (1996) Etiology of choroidal neovascularization in young patients. Ophthalmology 103(8): 1241-1244.
- Ho AC, Yannuzzi LA, Pisicano K, DeRosa J (1995) The natural history of idiopathic subfoveal choroidal neovascularization. Ophthalmology 102(5): 782-789.
- Lindblom B, Andersson T (1998) The prognosis of idiopathic choroidal neovascularization in persons younger than 50 years of age. Ophthalmology 105(10): 1816-1820.
- Cakir M, Cekiç O, Yilmaz OF (2009) Intravitreal bevacizumab for idiopathic choroidal neovascularisation. J AAPOS 13(3): 296-298.
- Kumar A, Prakash G, Singh RP (2004) Transpupillary thermotherapy for idiopathic subfoveal choroidal neovascularization. Acta Ophthalmol Scand 82(2): 205-208.
- Inoue M, Kadunosono K, Watanabe Y (2010) Results of one year follow up examinations after intravitreal Bevacizumab for idiopathic choroidal neovascularisation, Bevacizumab for idiopathic choroidal neovascularisation. Retina 30: 733-738.
- Mandal S, Garg S, Venkatesh P, Mithal C, Vohra R, et al. (2007) Intravitreal bevacizumab for subfoveal idiopathic choroidal neovascularization. Arch Ophthalmol 125(11): 1487-1492.
- Carreño E, Moutray T, Fotis K, Lee RW, Dick AD, et al. (2016) Phase IIb clinical trial of ranibizumab for the treatment of uveitic and idiopathic choroidal neovascular membranes. Br J Ophthalmol 100(9): 1221-1226.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...