Lupine Publishers Group
Lupine Publishers
Research ArticleOpen Access
To Compare the Retinal and Choroidal Thickness in Fuchs Uveitis Syndrome Patients with Healthy Controls Using Optical Coherence Tomography Seen at Tertiary Care Center Volume 3 - Issue 3
Khalid Khan1, Priyanka2*, Mansi Kishnani2 and Mihika Dube3
- 1Associate Professor, Department of Ophthalmology, Chirayu Medical College and Hospital, India
- 2Assistant Professor, Department of Ophthalmology, Chirayu Medical College and Hospital, India
- 3Assistant Professor, Department of Ophthalmology, RKDF medical college and hospital, India
Received:November 15, 2021; Published:November 23, 2021
Corresponding author: Priyanka, Assistant Professor, Department of Ophthalmology, Chirayu medical college and hospital, Bhopal, India
DOI: 10.32474/TOOAJ.2021.03.000164
Abstract
Purpose: To compare the retinal and choroidal thickness in Fuchs Uveitis Syndrome patients with healthy controls using optical coherence tomography seen at tertiary care center.
Method: 16 patients with unilateral Fuchs Uveitis Syndrome (FUS) and 20 healthy control subjects were enrolled in this retrospective study. Spectral domain optical coherence tomography was used to measure the central foveal thickness (CFT), retinal nerve fiber layer (RNFL) thickness and sub foveal choroidal thickness (SFCT) of the eyes with FUS and compared with the unaffected fellow eye and healthy controls.
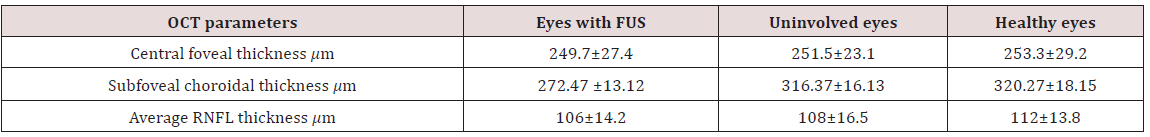
Results: The mean age of the patients was 35.2 ± 8 years. Seven patients (60%) were male, and nine (40%) were female. Diffuse stellate keratic precipitates (KPs) were seen in all patients. Mild anterior chamber reaction was noted 62.5%. Heterochromia was observed in 87.5% of the eyes, cataract in 43.8% of the eyes, and vitreous cells and debris in 37.5% of the eyes. The mean CFT was (249.7 ± 27.4𝜇m) in affected eyes, (251.5± 23.1 𝜇m) in unaffected eyes of FUS and (253.3 ± 29.2 𝜇m) in healthy control which were statistically insignificant on comparison (𝑝 value > 0.05). The mean SFCT was significantly thinner in eyes with FUS (272.47 ± 13.12 μm) than in the fellow eyes without FUS (316.37 ± 16.13 μm; p = 0.04). and control (320.27 ± 18.15). The average RNFL thickness was found to be (106 ± 14.2 μm) in eyes with FUS, (108 ± 16.5μm) in eyes without FUS and (112 ±13.8μm) in healthy control which were statistically not significant (p value > 0.05).
Conclusion: We conclude that affected eyes in patients with FUS tend to have thinner choroids as compared to unaffected fellow eyes which is consistent with previous studies. It might be associated with chronic inflammation induced choroidal is chaemic changes. Future studies using swept source OCT will further improve precision to get choroid findings more accurate.
Keywords:Choroid; Fuchs Uveitis Syndrome; SD-OCT; Retinal Nerve Fiber Layer
Introduction
Fuchs’ uveitis syndrome (FUS) is an intraocular inflammatory condition that involves anterior segment, lens, vitreous humor and optic disc. It accounts for 2-11% of all uveitis cases [1]. Although many genetic, immunological, vascular and sympathetic theories have been proposed, recent studies show evidence of rubella or herpes simplex virus, toxoplasma association in some cases of FUS [2]. It is a frequently unilateral and typical age at presentation is 30-40 years [3,4]. The diagnostic criteria include stellate keratic precipitates (KPs) scattered diffusely all over cornea, chronic lowgrade anterior chamber reactions, iris atrophy with or without heterochromia, absence of posterior synechiae, vitreous opacities and macular edema [5]. It affects both genders equally and the prognosis is usually good [6]. Iris atrophy and heterochromia are due to atrophy and depigmentation of all iris layers, although it is not pathognomonic. Recently, fluorescein angiography (FA) had provided better information about the posterior segment involvement in FUS [7-9]. Optical Coherent Tomography (OCT) is a routinely employed noninvasive tool in detecting most posterior pole retinal abnormalities. The Enhanced Depth Imaging (EDI) in spectral domain (SD) OCT and swept source (SS) OCT allow visualizing the choroid more accurately [10,11]. Some studies documented the changes in choroidal thickness using EDI-OCT in uveitic conditions, such as Vogt–Koyanagi–Harada (VKH) disease, Behçet disease (BD), ocular sarcoidosis providing remarkable information about disease activity [12,13]. The natural course of the disease is slow to progress, without substantial reduction of visual acuity until significant vitreous opacities or cataract develop. FUS is often misdiagnosed or diagnosed delay leading to posterior subcapsular opacity and elevated IOP mainly due to long-term corticosteroid therapy. There are very few reports in the literature comparing macular, RNFL and choroidal thickness in FUS patients. The purpose of the current study was to measure central foveal thickness (CFT), subfoveal choroidal thickness (SFCT) and retinal nerve fiber layer (RNFL) thickness, in patients with FUS and to compare these with the unaffected fellow eyes and the age, sex and refractive equivalent-matched healthy controls. To the best of our knowledge, it is the first comparative study to evaluate SFCT and other parameters in FUS using spectral domain SD-OCT on FUS from central India.
Material and Methods
This retrospective study was conducted at a tertiary care center from central India. The medical records of 16 patients with FUS and 20 healthy controls between september 2018 and august 2021 were reviewed. Data including age, sex, ocular and medical history, ophthalmic examination, laboratory work-up and OCT parameters were retrieved from patient record. Aii patients had best-corrected visual acuity (BCVA), slit-lamp biomicroscopy, Goldmann applanation tonometry and dilated fundoscopy. The inclusion criteria were diagnosed unilateral FUS based on clinical findings and fundus sufficient for its visualization on clinical examination. Bilateral FUS, history of previous ocular surgery, eyes with dense cataract or media opacity obscuring the visualization of choroid, presence of a coexisting ocular or systemic disease and use of any topical or systemic medications. were excluded from study. The control group consisted of age-, sex-, and refractive equivalent-matched healthy controls who visited ophthalmology clinic for routine examination. The laboratory investigations included complete blood counts, angiotensin converting enzyme, mantoux test and venereal disease research laboratory tests etc. To exclude other causes of anterior or intermediate uveitis. The CFT and RNFL thickness of eyes with FUS were evaluated with SD-OCT and compared with the unaffected fellow eyes and healthy controls. The EDI mode was used to evaluate SFCT. SFCT was defined as the vertical distance from the outermost hyperreflective line of the retinal pigment epithelium (RPE) to choroid-sclera junction under the center of the fovea and was measured using the calipers available within the software. The RNFL thickness (from the inner margin of the internal limiting membrane to the outer margin of the RNFL layer) was automatically segmented using software version. Average RNFL was used for analysis. Statistical analyses were performed with R version 4.0.5. Data were recorded as the mean ± standard deviation (SD). Quantitative data was analyzed using one way analysis of variance (ANOVA) test. An independent 𝑡-test and Chi-square test were used to compare variables between patients with FUS and healthy control subjects. A value of 𝑝< 0.05 was considered to be statistically significant for all analyses.
Results
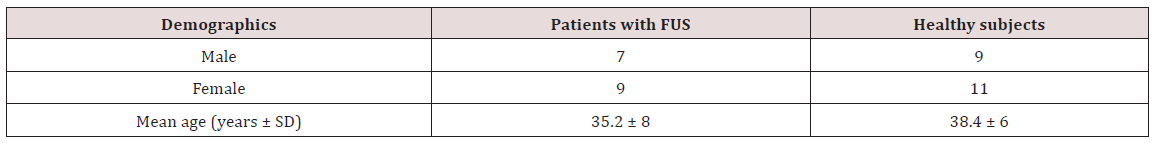
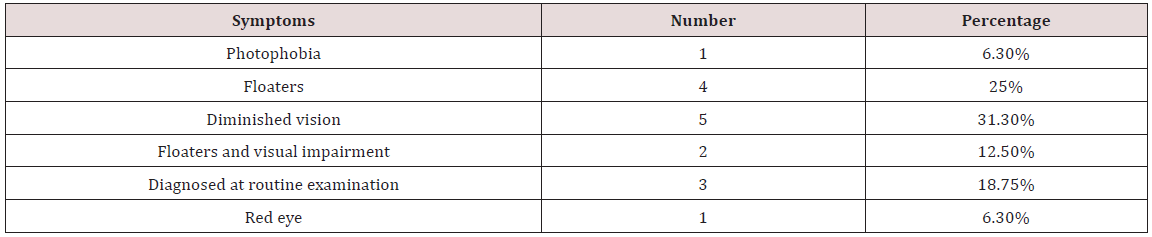
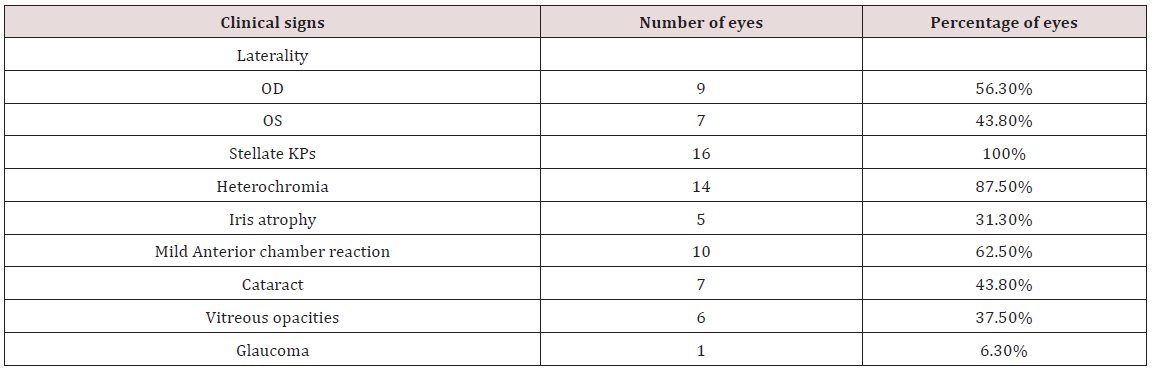
16 patients with FUS (9 females and 7 males) and 20 healthy control subjects (11 females and 9 males) were included for analysis in this study. The mean age of FUS patients was 35.2±8 years, while it was 38.4± 6years for controls, which was statistically insignificant (𝑝>0.05) (Table 1). Gender differences in both groups were also statistically insignificant (𝑝>0.05). Blurred vision and floaters were the most frequent presenting symptoms {5 patients, (31.3%) and 4 patients (25%) respectively}. Other symptoms included red eye (1 patient, 6.3%), photophobia (1 patient, 6.3%). Three patients were asymptomatic (18.75%), and the diagnosed during a routine eye examination (Table 2). Iris atrophy was present in 5 patients. Heterochromia was present in 14 patients. Cataract was present in 7 patients. Stellate keratic precipitates were noted in all patients. Mild anterior chamber reactions were seen in 10 patients. Vitreous cells or debris were observed in 6 patients (Table 3). The cause of visual impairment was cataract in all cases. The central foveal thickness was 249.7±27.4𝜇m in the affected eyes, 251.5±23.1 𝜇m in the unaffected eyes of FUS patients, and 253.3±29.2 𝜇m in control subjects. There were no significant differences in central foveal thickness between the affected and unaffected eyes of FUS patients (𝑝 = 0.93) or between the affected eyes of FUS patients and the eyes of control subjects (𝑝 = 0.9). The mean SFCT was found to be 272.47 ± 13.12μm in eyes with FUS and 316.37± 16.13μm in eyes without FUS (p = 0.04) and 320.27 ± 18.15𝜇m in the eyes of healthy control subjects. There was choroidal thinning at fovea in the affected eyes of FUS patients compared with the unaffected eyes or control subjects, Average RNFL thickness was 106 ±14.2𝜇m in the affected eyes of FUS patients, 108±16.5𝜇min the unaffected eyes of FUS patients, and 112 ± 13.8𝜇m in the eyes of healthy control subjects (Table 4). No significant differences in RNFL thickness were observed between the affected and unaffected eyes of FUS patients (𝑝 = 0.92) or between the affected eyes of FUS patients and the eyes of control subjects (𝑝 = 0.76)
Discussion
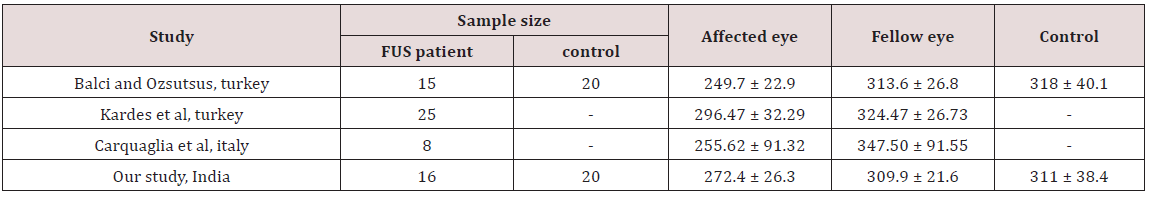
To our knowledge, very few comparative studies on FUS patients have been done till yet. In the present study, we compared central foveal thickness, retinal nerve fiber layer and subfoveal choroidal thickness between the affected eyes, the unaffected eyes of FUS patients and healthy controls from central India. Although we found choroidal thinning at fovea in the affected eyes of FUS patients compared with the unaffected eyes of FUS patients or control subjects, there was no statistically significant difference in RNFL and central foveal thickness. FUS was first described in 1906, recent studies have focused on various viral agents and the etiology of FUS remains controversial. In FUS, persistence of chronic lowgrade inflammation for years leads to various degrees of atrophy of the iris and ciliary body. As the choroid being more vulnerable to the effects of the inflammatory and vascular diseases than other tissues, imaging of choroid is important for understanding the pathophysiology of various diseases. EDI mode using SD-OCT devices enables cross-sectional, high resolution better visualization of the choroid. Many studies have documented the effect of various acute and chronic ocular inflammatory conditions on choroidal abnormalities. Nakayama et al. showed that choroidal thickness as a marker for the degree of choroidal inflammation in acute Vogt- Koyanagi-Harada disease using EDI-OCT [14]. Kim et al. found an increase in subfoveal choroidal thickness in the acute phase of Behcet’s posterior uveitis [15]. Multiple studies suggest that increased blood flow and choroidal effusion is the mechanism responsible for choroidal thickening in acute inflammation [16,17]. However, Coskun et al. observed the thinning of subfoveal choroid in chronic Behcet’sassociated posterior uveitis probably due to chronic inflammation induced fibrosis [18]. Very few studies from Turkey and Italy like Balci and Ozsutsus, Kardes et al. and Carquaglia et al. showed the comparison between the affected and fellow eye in FUS patients [19-21] (Table 5). The study by Kardes et al. had findings consistent with the study of Balci and Ozsutsus. We propose that chronic anterior chamber and vitreous inflammation in eyes with FUS may affect choroidal perfusion, which may result in ischaemic changes leading to atrophy and fibrosis of the choroid tissue, thereby reducing choroidal thickness. Limitations of our study is being retrospective nature and small sample size. We have used SD OCT in this study and with advent of new imaging methods designed specifically for the choroid, SS OCT which allows examination of the choriocapillaris, and larger choroidal vessels more clearly can further improve precision to determine the inner and outer boundaries of the choroid findings in the future. To conclude, we found subfoveal thinner choroid in FUS as compared to uninvolved fellow eyes, but we could not find a statistically significant comparison of foveal and RNFL thickness in FUS versus unaffected eye. Our findings are also consistent with those of previous studies. As this is the first analysis of its kind from central India, longitudinal studies with large sample size would help in more understanding of the effect of chronic inflammation on the choroid in FUS in future.
References
- A Rodriguez, M Calonge, M Pedroza Seres (1996) Referral patterns of uveitis in a tertiary eye care center. Archives of Ophthalmology 114(5): 593-599.
- MT de Abreu, R Belfort Jr, PS Hirata (1982) Fuchs’ heterochromic cyclitis and ocular toxoplasmosis. American Journal of Ophthalmology 93(6): 739-744.
- Kazokoglu H, Onal S, Tugal Tutkun I (2008) Demographic and clinical features of uveitis in tertiary centers in Turkey. Ophthalmic Epidemiol 15(5): 285-293.
- Rathinam SR, Namperumalsamy P (2000) Global variation and pattern changes in epidemiology of uveitis. Indian J Ophthalmol 55(3): 173-183.
- NP Jones (1993) Fuchs’ heterochromic uveitis: an update. Survey of Ophthalmology 37(4): 253-272.
- Mohamed Q, Zamir E (2005) Update on Fuchs’ uveitis syndrome. Curr Opin Ophthalmol 16(6): 356-363.
- Kardes E, SezginAkçay BI, Unlu C, Ergin A (2017) Choroidal thickness in eyes with Fuchs uveitis syndrome. OculImmunolInflamm 25(2): 259-266.
- Bouchenaki N, Herbort CP (2010) Fluorescein angiographic findings and clinical features in Fuchs’ uveitis. Int Ophthalmol 30(5): 511-519.
- Bouchenaki N, Herbort CP (2010) Fluorescein findings and clinical features in Fuchs’ uveitis. Int Ophthalmol 30(5): 511-519.
- AlamS, Zawadzki RJ, Choi S (2006) Clinical application of rapid serial fourier-domain optical coherence tomography for macular imaging. Ophthalmology 113(8): 1425-1431.
- de Boer JF, Leitgeb R, Wojtkowski M (2017) Twenty-five years of optical coherence tomography: the paradigm shift in sensitivity and speed provided by Fourier domain OCT invited. Biomed Opt Express 8: 3248-3280.
- Nakayama M, Keino H, Okada AA, (2012) Enhanced depth imaging optical coherence tomography of the choroid in Vogt-Koyanagi-Harada disease. Retina 32(10): 2061-2069.
- Coskun E, Gurler B, Pehlivan Y (2013) Enhance Depth Imaging Optical Coherence Tomography Findings in Behçet Disease. OculImmunolInflamm 21(6): 440-445.
- M Nakayama, H Keino, AA Okada (2012) Enhanced depth imaging optical coherence tomography of the choroid in Vogt- Koyanagi-Harada disease. Retina 32(10): 2061-2069.
- Kim M, Kim H, Kwon HJ (2013) Choroidal thickness in Behçet’s uveitis: an enhanced depth imaging-optical coherence tomography and its association with angiographic changes. Invest Ophthalmol Vis Sci 54(9): 6033-6039.
- N Akcar, F G¨oktekin, A ¨ Ozer, C Korkmaz (2010) Doppler sonography of ocular and carotid arteries in Behcet patients. Journal of Clinical Ultrasound 38(9): 486-492.
- M Kim, SS Kim, HJ Kwon, HJ Koh, SC Lee (2012) Association between choroidal thickness and ocular perfusion pressure in young, healthy subjects: enhanced depth imaging optical coherence tomography study. Investigative Ophthalmology and Visual Science 53(12): 7710-7717.
- E Coskun, B Gurler, Y Pehlivan (2013) Enhanced depth imaging optical coherence tomography findings in Behcet disease. Ocular Immunology and Inflammation 21(6): 440-445.
- Balci O, Ozsutcu M (2016) Evaluation of retinal and choroidal thickness in Fuchs’ uveitis syndrome. J Ophthalmol 2016: 1657078.
- Cerquaglia A, Iaccheri B, Fiore T (2016) Full-thickness choroidal thinning as a feature of Fuchs uveitis syndrome: quantitative evaluation of the choroid by enhanced depth imaging optical coherence tomography in a cohort of consecutive patients. Graefes Arch ClinExpOphthalmol 254(10): 2025-2031.
- Kardes E, Sezgin Akçay BI, Unlu C, Ergin A (2017) Choroidal thickness in eyes with Fuchs uveitis syndrome. OculImmunolInflamm 25(2): 259-266.